Lung abscess-etiology, diagnostic and treatment options
Introduction
Lung abscess is defined as a circumscribed area of pus or necrotic debris in lung parenchima, which leads to a cavity, and after formation of bronchopulmonary fistula, an air-fluid level inside the cavity (1).
Lung abscess is in the group of lung infections such as lung gangrene and necrotizing pneumonia which is characterized with multiple abscesses (2).
The clinical signs and therapy of lung abscess was described for the first time by Hippocrates. In pre-antibiotic era, one third of patients with lung abscess would die, the other third of patients would recover fully, and the rest of them would survive with sequels such as chronic lung abscess, pleural empyema or bronchiectasis (3). In that time, surgery was considered as the only effective therapy, and today most of the patients will be fully recovered only with antibiotic therapy.
Hundred years ago, mortality from lung abscess was about 75% of patients (4). Open drainage of lung abscess decreased mortality on 20-35% and with antibiotic therapy mortality drop on about 8.7% (5). At the same time, progress in oral and dental hygiene declined the incidence of lung abscesses. Today, aspiration from oral cavity is considered the major cause of lung abscesses as well as poor oral and dental hygiene (6).
In pre antibiotic era, lung abscess was caused by one type of bacteria, and today almost in all cases is caused by poly microbial flora (2).
Lung abscess can be divided on acute (less than 6 weeks) and chronic (more than 6 weeks). It can be called primary as a result of aspiration of oropharyngeal secretions (dental/periodontal infection, para nasal sinusitis, disturbance states of consciousness, swelling disorders, gastro-oesophageal reflux disease, frequent vomiting, necrotizing pneumonia's or in immunocompromised patients. Secondary lung abscesses occurred in bronchial obstructions (by tumor, foreign body or enlarged lymph nodes), with coexisting lung diseases (bronchiectasis, bullous emphysema, cystic fibrosis, infected pulmonary infarcts, lung contusion), then spreading from extrapulmonary sites-hematogenous (abdominal sepsis, infective endocarditis, infected canula or central venous catheter, septic thromboembolisms) or by direct spreading (broncho-oesophageal fistula, subphrenic abscess) (6).
Based on way of spreading, lung abscess can be bronchogenic (aspiration, inhalation) and haematogenic-dissemination from other infected sites.
Division of lung abscesses:
- According to the duration:
- Acute (less than 6 weeks);
- Chronic (more than 6 weeks);
- By etiology:
- Primary (aspiration of oropharyngeal secretions, necrotizing pneumonia, immunodeficiency);
- Secondary (bronchial obstructions, haematogenic dissemination, direct spreading from mediastinal infection, from subphrenium, coexisting lung diseases);
- Way of spreading:
- Brochogenic (aspiration of oropharyngeal secretions, bronchial obstruction by tumor, foreign body, enlarged lymph nodes, congenital malformation);
- Haematogenic (abdominal sepsis, infective endocarditis, septic thromboembolisms).
Aspiration of oropharyngeal secretions:
- Dental/peridental infection;
- Para nasal sinusitis;
- Disturbance states of consciousness;
- Swelling disorders;
- Gastro-oesophageal reflux disease;
- Frequent vomiting;
- Intubated patients;
- Patients with tracheostomy;
- Nervous recurrent paralysis;
- Alcoholism.
Haematogenic dissemination:
- Abdominal sepsis;
- Infective endocarditis;
- Intravenous drug abuse;
- Infected cannula or central venous catheter;
- Septic thromboembolisms.
Coexisting lung diseases:
- Bronchiectasis;
- Cystic fibrosis;
- Bullous emphysema;
- Bronchial obstruction by tumor, foreign body or enlarged lymph nodes;
- Congenital malformations (pulmonary sequestration, vasculitis, cystitis);
- Infected pulmonary infarcts;
- Pulmonary contusion;
- Broncho-oesophageal fistula
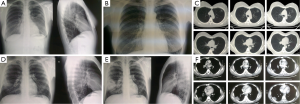
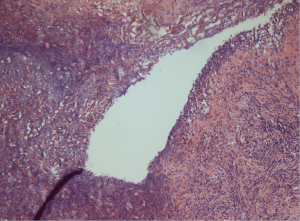
Acute lung abscess is usually circumscribed with not so well-defined surrounding to lung parenchyma, fulfilled with thick necrotic detritus (Figure 1). Histologically, in central parts of abscess there are necrotic tissue mixed with necrotic granulocytes and bacteria. Around this area there are preserved neutrophillic granulocytes with dilated blood vessels and inflammatory oedema (Figure 2).
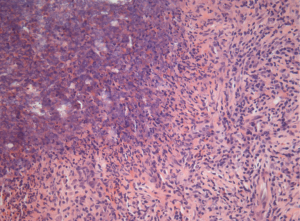
Chronic lung abscess is usually irregular star-like shape with well-defined surrounding to lung parenchyma, fulfilled with grayish line or thick detritus (Figure 3). In the centre of abscess is located pus wit or without bacteria. Around abscess is located pyogenic membrane through which white blood cells are migrating to abscess cavitation. Around pyogenic membrane lymphocytes, plasma cells and histiocytes are placed in connective tissue (Figure 4).
Contributing factors for lung abscess are: elderly, dental/peridental infections (gingivitis-with bacterial concentration >1011/mL), alcoholism, drug abuse, diabetes mellitus, coma, artificial ventilation, convulsions, neuromuscular disorders with bulbar dis functions, malnutrition, therapy with corticosteroids, cytostatics or immunosuppressants, mental retardation, gastro-oesophageal reflux disease, bronchial obstruction, inability to cough, sepsis (7-9).
In over 90% cases of lung abscess poly microbial bacteria can be found (10). From anaerobic bacteria in lung abscess predominant isolates being gram-negative Bacteroides fragilis, Fusobacterium capsulatum and necrophorum, gram-positive anaerobic Peptostreptococcus and microearophillic streptococci. From aerobic bacteria predominant isolates in lung abscess being Staphylococcus aureus [including methicillin resistant staphylococcus aureus (MRSA)], Streptococcus pyogenes and pneumonia, Klebsiella pneumonia, Pseudomonas aeruginosa, Haemophilus influenza (type B), Acinetobacter spp, Escherichia coli, and Legionela (11-13).
Anaerobic bacteria have been for decades the most dominant type of bacteria in lung abscess with Streptococcus spp (Streptococcus pneumonia serotype 3 i Streptococcus anginosus complex). During the last decade the most isolated type bacteria in lung abscess, especially in Taiwan has been Klebsiella pneumonia, so it is very important to have specific antibiotic therapy for that type of bacteria (14,15). Staphylococcus aureus is the most common isolated etiologic pathogen of lung abscess in children (16,17).
Etiologic pathogen for lung abscess might be, as well Mycobacterium spp, Aspergillus, Cryptococcus, Histoplasma, Blastomyces, Coccidoides, Entamoeba histolytica, Paragominus westermani. Actinomyces and Nocardia asteroides are known as important etiologic pathogens of lung abscess and they require a longer duration (6 months) of antibiotic administration (18).
Predictive parts of lung as common sites for lung abscess have been apical segment of lower lobe of right and sometimes of left lung, then lateral part of posterior segment of right upper lobe—axillary sub segment, and middle lobe in case of vomiting and aspiration in prone position—this is typically for alcoholic persons. In 75% of all lung abscesses, they are located in posterior segment of right upper lobe or in apical segment of lower lobe of both lungs (5).
Etiological, abscesses occurred after oropharyngeal aspiration is localized in posterior segments of the lungs, and there are no patterns for hematological dissemination of lung abscesses.
Initially, aspiration secretion is localized in distal parts of bronchi causing localized pneumonitis (16,17). In the next 24 to 48 hours (h) a larger area of inflammation with necrotic debris will develop. Invasive bacterial toxins, vasculitis, venous thrombosis and proteolytic enzymes from neutrophilic granulocytes will make a colliquative necrotic focus (19).
If the infective lung tissue affects visceral pleura, a pyopneumothorax or pleural empyema will develop. In case of adequate antibiotic therapy and good immunologic status of patient, the chronic inflammatory reaction will circumscribe the process. In case of inadequate or delayed antibiotic therapy, poor general condition of patient, a sepsis can occur. If there is connection with the bronchus, necrotic detritus will empty the abscesses cavity and radiological sign of air-fluid level will occur.
In case of favorable outcome, a necrotic tissue will be eliminated by lysis and phagocytosis and granulation tissue will make a scar tissue.
In case of adverse outcome, infection will spread around the lung tissue and pleural, mediastinal or cutaneous fistula can occur. In chronic abscess a necrotic detritus will be usually reabsorb and fibrosis and calcification can occur.
Signs and symptoms
Early signs and symptoms of lung abscess cannot be differentiate from pneumonia and include fever with shivering, cough, night sweats, dispnea, weight loss and fatigue, chest pain and sometimes anemia. At the beginning cough is non-productive, but when communication with bronchus appears, the productive cough (vomique) is the typical sign (20,21). Cough remains productive, sometimes followed by hemoptysis. In patients with chronic abscess clubbing fingers can appear.
Differential diagnosis includes excavating tuberculosis and mycosis, but seldom can been seen radiological sign of gas-liquid level. Pulmonary cystic lesions, such as intrapulmonary located bronchial cysts, sequestration or secondary infected emphysematous bullae can be difficult to differentiate, but localization of lesion and clinical signs can indicate the appropriate diagnosis. Localized pleural empyema can be distinguished by using CT scan or ultrasound (22).
Excavating bronchial carcinomas such as squamocellular or microcellular carcinoma are usually presented with thicker and irregular wall comparing to infectious lung abscess (23) (Figure 5). Absence of febricity, purulent sputum and leukocytosis can indicate the carcinoma and not the infective disease (24). Radiological sign of air-fluid level can be seen and in hydatid cyst of lung (25,26) (Figure 6).
Differential diagnosis:
- Excavating bronchial carcinoma (squamocellular or microcellular);
- Excavating tuberculosis;
- Localized pleural empyema;
- Infected emphysematous bullae;
- Cavitary pneumoconiosis;
- Hiatus hernia;
- Pulmonary hematoma;
- Hydatid cyst of lung;
- Cavitary infarcts of lung;
- Wegener’s granulomatosis.
Diagnostic bronchoscopy is a part of diagnostic protocol for taking the material for microbiological examination and to confirm intrabronchial cause of abscess-tumor or foreign body. Sputum examination is useful for identification of microbiological agents or confirmation of bronchial carcinoma (27).
Therapy
Standard conservative therapy for lung abscess with anaerobic bacteria is clindamycin (600 mg IV on 8 h), who showed, in several clinical trials superiority to penicillin in terms of rates of response, duration of fever and time to resolution of putrid sputum (28). Some types of Bacteroides species and Fusobacterium species can produce β-lactamase, so they are resistant to penicillin. About 15-20% of anaerobic bacteria who are responsible for lung abscess formation are resistant to penicillin only, so alternative is combination of penicillin and clavulanate or combination of penicillin and metronidazole (29).
Metronidazole, as a single therapy does not appear to be particularly effective, due to poly microbial flora, presumably microaerophilic streptococci, such as Streptococcus milleri (30).
Recommended combinations of antibiotics for lung abscess are combination of β-lactam with inhibitors of β-lactamase (ticarcilin-clavulanate, ampicillin-sulbactam, amoxicillin-clavulanate, piperacilin-tazobactam), chloramphenicol, imipenem or meropenem, second generation of cephalosporins (cefoxitin, cefotetan), newer generation of fluoroquinolones-moxifloxacin, who shoved to be as effective as combination ampicillin-sulbactam (31).
Macrolide (erythromycin, clarithromycin, azithromycin) have very good therapeutic effect on poli microbial bacteria in lung abscess, except on fusobacterium species. Vancomycin is very effective for gram-positive anaerobic bacteria.
Aminoglycosides are not recommended in treatment of lung abscess since they poorly pass through fibrous pyogenic membrane of chronic abscess.
It is recommended to treat lung abscess with broad spectrum antibiotics, due to poly microbial flora, such as Clindamycin (600 mg IV on 8 h) and then 300 mg PO on 8 h or combination ampicilin/sulbactam (1.5-3 gr IV on 6 h) (32).
Alternative therapy is piperacilin/tazobactam 3.375 gr IV on 6 h or Meropenem 1 gr IV on 8 h (33).
For MRSA it is recommended to use linezolid 600 mg IV on 12 h or vancomycin 15 mg/kg BM on 12 h (34).
Effective answer to antibiotics therapy can be seen after 3-4 days, general condition will improve after 4-7 days, but completely healing, with radiographic normalization can be seen after two months.
If there is no improvement of general condition or radiographic finding, it is necessary to perform bronchoscopy due to some other etiological factor and change the antibiotics.
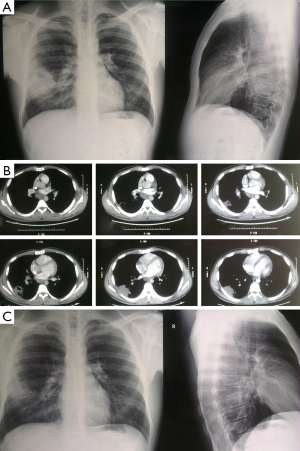
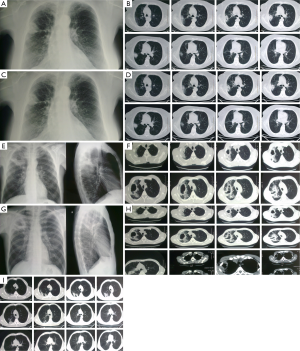
The duration of antibiotics therapy depends on the clinical and radiographic response of the patient. Antibiotics therapy should last at least until fever, putrid sputum and abscess fluid have resolved, usually between 5-21 days for intravenous application of antibiotics and then per oral application, in total from 28 to 48 days (14) with periodically radiographic and laboratory controls. Effects of antibiotic therapy on radiographic finding of lung abscess (Figure 7A-C).
Bronchoscopy should be the integral part of the algorithm for diagnostic and therapy of lung abscess. General supporting measures include hyper caloric diet, correction of fluids and electrolytes and respiratory rehabilitation with postural drainage. Drainage procedures include percussion and positioning to increase drainage through the airways. Lung abscess often will rupture spontaneously into the airways, which aids in clearing the infection, but also may result in spread of the infection to other parts of the lung.
Abscess greater than 6 cm in diameter or if symptoms lasts more than 12 weeks with appropriate therapy, have little chances for only conservative healing, and surgical therapy should be considered, if general condition allows. Options for surgery are: chest tube drainage or surgical resection of lung abscess with surrounding tissue.
Endoscopic drainage of lung abscesses is described as an alternative to chest tube drainage and is performed during the bronchoscopy with usage of laser. It was recommended for the patients with poor general condition, coagulopathies and for the abscesses with central locations in lungs. One of the possible complication of these technique is a spillage of necrotic detritus in other parts of the lungs (35,36).
Per cutaneous trans thoracic tube drainage is easy to do surgical procedure in local anaesthesia, and nowadays it is recommended to perform it ultrasound or computerized tomography (CT) scan control (37,38). The first one was described in 1938 for treatment of tuberculosis lung cavities. It was later used routinely in the management of lung abscesses, before the antibiotic era and became the treatment of choice (39). Per cutaneous chest tube drainage of lung abscess is indicated in about 11-21% patients after failure of antibiotics therapy (40).
Chest tube drainage, as a definitive therapy for lung abscess is present in about 84% of patients, with complication rate of drainage about 16% and mortality about 4% (39). Complications of tube drainage are spillage the necrotic detritus and infection in pleura with formation of pyopneumothorax, empyema or bronchopleural fistula or bleeding.
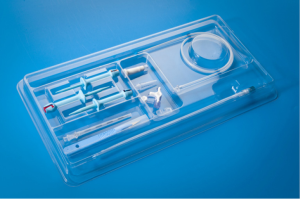
Per cutaneous trans thoracic tube drainage of lung abscess is performed in local anesthesia with or without ultrasound control (41,42). Chest tube drainage with trocar (Figure 8) is highly effective surgical procedure, but Seldinger technique (Figure 9) is recommended due to lesser complications (43). Chest tube drainage with trocar is recommended for thoracic surgeons, especially if during the procedure trocar passes through lung tissue.
The usage of intra-cavitary fibrinolytic agents (streptokinase, urokinaze) is not recommended, due to possibility of bronchopulmonary or bronchopleural fistula can occur (44). Average duration for tube drainage of lung abscess is about 10-16 days, and in case of prolong air leak, tube can be attach to Heimlich valve (Figures S1,S2).
In case of pleural space obliteration, with peripheral localisation of lung abscess, it is possible to perform pneumostomy or cavernostomy-open drainage of abscess (Monaldi procedure) but due to its invasiveness seldom is performed (35).
Surgical resection of lung abscess is the therapy of choice for about 10% of patients. Indications for surgical resection of lung abscess can be divided on acute and chronic.
Acute indications are: hemoptysis, prolonged sepsis and febricity, bronchopleural fistula, rupture of abscess in pleural cavity with pyopneumothorax/empyema.
Chronic indications are: unsuccessfully treated lung abscess more than 6 weeks, suspicion on cancer, cavitary larger than 6 cm, leukocytosis in spite of antibiotics.
Lobectomy is the resection of choice for large or central position of abscess. Atypical resection or segmentectomy are satisfactory procedures, if it is possible to remove complete abscess and if necessary surrounding lung tissue with necrotizing pneumonia (45).
Results of surgical treatment depend mostly of general condition and immunity of patient. Elderly patients, malnutrition and alcoholism are poor prognostic factors. Mortality rate after surgical resections is about 11-28% (35).
Minimal invasive surgical procedures, such as video assisted thoracoscopy is a method of choice for peripheral localization of lung abscess and without pleural adhesions and fibrothorax. Results of this surgical procedure are satisfactory, but this intervention requires general anesthesia, double lumen endotracheal tube or single-lumen endotracheal tube with insufflation of carbon dioxide. One of the possible complications is spillage of necrotic detritus in pleural cavity (46).
Overall mortality in lung abscess treatment is about 2.0-38.2% (17) with important role of patient age, malnutrition, comorbidity, immunity, appropriate and timely antibiotics and supportive therapy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Seo H, Cha SI, Shin KM, et al. Focal necrotizing pneumonia is a distinct entity from lung abscess. Respirology 2013;18:1095-100. [PubMed]
- Yazbeck MF, Dahdel M, Kalra A, et al. Lung abscess: update on microbiology and management. Am J Ther 2014;21:217-21. [PubMed]
- Bartlett JG. The role of anaerobic bacteria in lung abscess. Clin Infect Dis 2005;40:923-5. [PubMed]
- Schweigert M, Dubecz A, Stadlhuber RJ, et al. Modern history of surgical management of lung abscess: from Harold Neuhof to current concepts. Ann Thorac Surg 2011;92:2293-7. [PubMed]
- Moreira Jda S, Camargo Jde J, Felicetti JC, et al. Lung abscess: analysis of 252 consecutive cases diagnosed between 1968 and 2004. J Bras Pneumol 2006;32:136-43. [PubMed]
- Puligandla PS, Laberge JM. Respiratory infections: pneumonia, lung abscess, and empyema. Semin Pediatr Surg 2008;17:42-52. [PubMed]
- Gonçalves AM, Menezes Falcão L, Ravara L. Pulmonary abcess, a revision. Rev Port Pneumol 2008;14:141-9. [PubMed]
- Magalhães L, Valadares D, Oliveira JR, et al. Lung abscesses: review of 60 cases. Rev Port Pneumol 2009;15:165-78. [PubMed]
- Ando K, Okhuni Y, Matsunuma R, et al. Prognostic lung abscess factors. Kansenshogaku Zasshi 2010;84:425-30. [PubMed]
- Stock CT, Ho VP, Towe C, et al. Lung abscess. Surg Infect (Larchmt) 2013;14:335-6. [PubMed]
- Bartlett JG. Anaerobic bacterial infection of the lung. Anaerobe 2012;18:235-9. [PubMed]
- Wang JL, Chen KY, Fang CT, et al. Changing bacteriology of adult community-acquired lung abscess in Taiwan: Klebsiella pneumoniae versus anaerobes. Clin Infect Dis 2005;40:915-22. [PubMed]
- Pande A, Nasir S, Rueda AM, et al. The incidence of necrotizing changes in adults with pneumococcal pneumonia. Clin Infect Dis 2012;54:10-6. [PubMed]
- Takayanagi N, Kagiyama N, Ishiguro T, et al. Etiology and outcome of community-acquired lung abscess. Respiration 2010;80:98-105. [PubMed]
- Nicolini A, Cilloniz C, Senarega R, et al. Lung abscess due to Streptococcus pneumoniae: a case series and brief review of the literature. Pneumonol Alergol Pol 2014;82:276-85. [PubMed]
- Brook I. Anaerobic pulmonary infections in children. Pediatr Emerg Care 2004;20:636-40. [PubMed]
- Patradoon-Ho P, Fitzgerald DA. Lung abscess in children. Paediatr Respir Rev 2007;8:77-84. [PubMed]
- Yildiz O, Doganay M. Actinomycoses and Nocardia pulmonary infections. Curr Opin Pulm Med 2006;12:228-34. [PubMed]
- Tsai YF, Ku YH. Necrotizing pneumonia: a rare complication of pneumonia requiring special consideration. Curr Opin Pulm Med 2012;18:246-52. [PubMed]
- Yen CC, Tang RB, Chen SJ, et al. Pediatric lung abscess: a retrospective review of 23 cases. J Microbiol Immunol Infect 2004;37:45-9. [PubMed]
- Chan PC, Huang LM, Wu PS, et al. Clinical management and outcome of childhood lung abscess: a 16-year experience. J Microbiol Immunol Infect 2005;38:183-8. [PubMed]
- Lin FC, Chou CW, Chang SC. Differentiating pyopneumothorax and peripheral lung abscess: chest ultrasonography. Am J Med Sci 2004;327:330-5. [PubMed]
- Dursunoğlu N, Başer S, Evyapan F, et al. A squamous cell lung carcinoma with abscess-like distant metastasis. Tuberk Toraks 2007;55:99-102. [PubMed]
- Mahmood N, Azam H, Ali MI, et al. Pulmonary hydatid cyst with complicating Aspergillus infection presenting as a refractory lung abscess. Clin Med Insights Case Rep 2011;4:63-8. [PubMed]
- Toleti S, Subbarao M, Dwarabu P. Hydatid disease of the lung presenting with hemoptysis and simulating a lung abscess. Trop Parasitol 2012;2:69-70. [PubMed]
- Schiza S, Siafakas NM. Clinical presentation and management of empyema, lung abscess and pleural effusion. Curr Opin Pulm Med 2006;12:205-11. [PubMed]
- Nagashima O, Sasaki S, Nanba Y, et al. Analysis of predominant bacterial species and clinical backgrounds in lung abscess patients. Nihon Kokyuki Gakkai Zasshi 2011;49:623-8. [PubMed]
- Bartlett JG. How important are anaerobic bacteria in aspiration pneumonia: when should they be treated and what is optimal therapy. Infect Dis Clin North Am 2013;27:149-55. [PubMed]
- Fernández-Sabé N, Carratalà J, Dorca J, et al. Efficacy and safety of sequential amoxicillin-clavulanate in the treatment of anaerobic lung infections. Eur J Clin Microbiol Infect Dis 2003;22:185-7. [PubMed]
- Hecht DW. Anaerobes: antibiotic resistance, clinical significance, and the role of susceptibility testing. Anaerobe 2006;12:115-21. [PubMed]
- Ott SR, Allewelt M, Lorenz J, et al. Moxifloxacin vs ampicillin/sulbactam in aspiration pneumonia and primary lung abscess. Infection 2008;36:23-30. [PubMed]
- Allewelt M, Schüler P, Bölcskei PL, et al. Ampicillin + sulbactam vs clindamycin +/- cephalosporin for the treatment of aspiration pneumonia and primary lung abscess. Clin Microbiol Infect 2004;10:163-70. [PubMed]
- Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 2007;44 Suppl 2:S27-72. [PubMed]
- David MZ, Daum RS. Community-associated methicillin-resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic. Clin Microbiol Rev 2010;23:616-87. [PubMed]
- Herth F, Ernst A, Becker HD. Endoscopic drainage of lung abscesses: technique and outcome. Chest 2005;127:1378-81. [PubMed]
- Shlomi D, Kramer MR, Fuks L, et al. Endobronchial drainage of lung abscess: the use of laser. Scand J Infect Dis 2010;42:65-8. [PubMed]
- Yunus M. CT guided transthoracic catheter drainage of intrapulmonary abscess. J Pak Med Assoc 2009;59:703-9. [PubMed]
- Kelogrigoris M, Tsagouli P, Stathopoulos K, et al. CT-guided percutaneous drainage of lung abscesses: review of 40 cases. JBR-BTR 2011;94:191-5. [PubMed]
- Wali SO. An update on the drainage of pyogenic lung abscesses. Ann Thorac Med 2012;7:3-7. [PubMed]
- Mueller PR, Berlin L. Complications of lung abscess aspiration and drainage. AJR Am J Roentgenol 2002;178:1083-6. [PubMed]
- Feller-Kopman D. Ultrasound-guided thoracentesis. Chest 2006;129:1709-14. [PubMed]
- Liu YH, Lin YC, Liang SJ, et al. Ultrasound-guided pigtail catheters for drainage of various pleural diseases. Am J Emerg Med 2010;28:915-21. [PubMed]
- Kuhajda I, Zarogoulidis K, Kougioumtzi I, et al. Tube thoracostomy; chest tube implantation and follow up. J Thorac Dis 2014;6:S470-9. [PubMed]
- Hogan MJ, Coley BD. Interventional radiology treatment of empyema and lung abscesses. Paediatr Respir Rev. 2008;9:77-84. [PubMed]
- Pagès PB, Bernard A. Lung abscess and necrotizing pneumonia: chest tube insertion or surgery? Rev Pneumol Clin 2012;68:84-90. [PubMed]
- Nagasawa KK, Johnson SM. Thoracoscopic treatment of pediatric lung abscesses. J Pediatr Surg 2010;45:574-8. [PubMed]