Histopathological correlations of appendectomies: a clinical audit of a single center
Introduction
Appendicitis is a common acute surgical emergency with over 40,000 cases in the UK every year (1) and the estimated life time risk of appendicitis in the USA is 8.6% and 6.7% for males and females respectively (2). The diagnosis of appendicitis is largely clinical and appendectomy is the treatment of choice. Delayed diagnosis of appendicitis could lead to complications like perforated appendix, peritonitis, sepsis, increased morbidity and mortality (3,4). Right iliac fossa pain can be a presenting complaint of different pathologies that may mimic appendicitis especially in the female population causing diagnostic difficulties and often leads to negative appendectomies.
There is variation between institutions in the practice of routine histopathological examination of appendectomy specimens. Arguments against the practice include the rarity of incidental pathologies that may impact on treatment and also the financial implications of routine histopathological assessments (5,6). Histological examination of appendix specimens is routinely done in our institution hence the need to correlate the histopathological findings with the clinical diagnosis of appendicitis.
Methods
Data of patients who had appendectomies during the study period between January and December 2013 was retrieved from the surgical database. Study population characteristics and the histopathology reports of the appendectomy specimens were retrieved from the computer records. The primary outcome measure was appendicitis confirmed by histopathology.
Negative appendectomy was defined as a post-operative appendix specimen for suspected appendicitis that was however microscopically normal on histopathological examination without evidence of inflammation, tumors and parasitic infestation (7-10). Fibrous obliteration of the lumen of the appendix and reactive lymphoid hyperplasia without evidence of inflammation was not included as abnormal findings (8,11). The variables in the data were summarized using appropriate summary statistics. Analysis of the data was carried out by IBM SPSS version 20.
Results
Study population
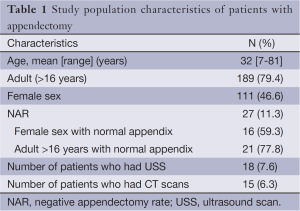
Overall 238 appendectomies were performed during the study period. The mean age of the patients was 32 years (range, 7-81 years). Adult patients (>16 years) represented 79.4% of the study population. The female sex accounted for 46.6% of all the patients (Table 1).
Full table
Histopathology findings
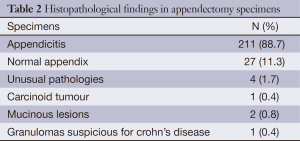
Of the 238 resected appendix, 211 (88.7%) had histopathology findings consistent with appendicitis which was variously reported as acute suppurative appendicitis, transmural inflammation of the appendix with or without fecalith and gangrenous perforated appendix. Four cases of fibrous obliteration of the lumen of the specimen without evidence of inflammation were reported.
Approximately 1.7% of the 238 specimens were unusual pathologies other than inflammation of the appendix (Table 2) and two mucinous lesions were reported. One of the findings suggestive of mucinous cystadenoma was reported as “specimen is covered with fibrous exudate. A nodule of 10 mm in maximum dimension is seen. Focally dilated appendiceal lumen is lined with mildly atypical epithelium which is thrown into convoluted folds. Mucin extravasation with a single gland within tissue is seen all suggestive of cystadenoma with low grade dysplasia associated with acute appendicitis”. One case of carcinoid tumor at the tip of the appendix which was synaptophysin and chromogranin positive was reported. The negative appendectomy rate (NAR) was 11.3%. The female sex accounted for 59.3% of the negative appendectomies. Adults (>16 years) represented 77.8% of the negative appendectomies (Table 1).
Full table
Imaging
Of the total number of the patients with suspected appendicitis, 7.6% [18] had abdominal ultrasound scan (USS) and the female sex accounted for 94% of patients who had abdominal USS. Three and seven patients were reportedly positive and negative for appendicitis on USS respectively. Eight patients were reported as inconclusive on USS. Correlating the USS findings with the histopathological findings, the three patients reported as positive on USS were truly positive on histopathology. Five patients of seven USS negative cases had positive histopathological report and five patients of eight USS inconclusive patients also had positive histopathological report.
The proportion of patients who had CT scans was 6.3% [15] and all the 15 patients had CT scan findings consistent with acute appendicitis. The CT scan findings correlated with the histopathological findings of appendicitis.
Discussion
This study reviews the histopathological findings of resected appendix specimens. Appendectomy is a common surgical procedure for the management of acute appendicitis. NAR, a recognized consequence of appendectomy varies from 6% to 40% in the literature (8,12,13). The suggested acceptable rate of negative appendectomy is 20% (4,11) and the NAR for this study was 11.3%. The high rates of negative appendectomy was considered acceptable to avoid missing cases of appendicitis and the possible sequelae of appendicitis such as perforation, peritonitis, abscess formation, peritonitis and sepsis (11). Arguments against acceptable high rates of negative appendectomies have been made with the observation of attendant significant clinical and financial consequences (14).
Flum and Koepsell reported the findings of a retrospective analysis of 261,134 patients who underwent non-incidental appendectomies with a NAR of 15.3% [39,901]. When compared with patients with appendicitis, negative appendectomy was associated with a significantly longer length of stay (5.8 vs. 3.6 days, P<0.001), infectious complications rate (2.6% vs. 1.8%, P<0.001) case fatality rate (1.5% vs. 0.2%, P<0.001) and total charge-admission ($18,780 vs. 10,584, P<0.001). An estimated $741.5 million in total hospital charges resulted from admissions in which a negative appendectomy was performed (15). Hence NAR has been recognized as a quality metric in the management of acute appendicitis.
The incidence of negative appendectomies has reportedly been on the decline with large database studies as low as 6-8.4% (9,16) and single institution studies as low as 1.7-7% (10,17). The documented decline in NAR notably coincided with increased use of imaging especially computed tomography and laparoscopy as diagnostic tools for appendicitis (18). Low NAR have been attributed to the use of computed tomography by some studies (10,11,17), however, a definitive causal relationship has not been established.
CT has a sensitivity of 90-100%, specificity of 91-99% and positive predictive value of 95-97%. CT has also proven to be superior to USS in the diagnosis of suspected appendicitis (4) and this observation is consistent with the findings of this study which suggests that USS negative and USS inconclusive reports are not reliable. The contributory role of imaging in the low incidence of NAR has been further supported by the findings of Raja et al. in an 18-year review. They observed significant reduction in NAR from 23% in 1990 to 1.7% in 2007 and this reduction occurred with the significant increase of preoperative CT from 1% to 97.5% in the same period (10). Our study reinforces the importance of history taking, clinical examination, basic laboratory investigations and the selective use of imaging in the diagnosis of acute appendicitis.
Higher NAR in the female sex compared to the male sex have been reported by multiple studies (7-9,19,20). Seetahal et al. in a 10-year review of a nationally representative sample of 475,651 cases of appendectomy reported that women accounted for 71.6% of the negative appendectomies (16). This is consistent with the findings of this study in which females accounted for approximately 60% of the negative appendectomies. Reasons adduced for this observation includes the gynecological conditions that could mimic the presentation of acute appendicitis. Ovarian cysts, leiomyoma, endometriosis, benign ovarian neoplasms, malignant ovarian disease, pelvic adhesions have been reportedly misdiagnosed as acute appendicitis in women (16).
Histopathological examination of resected appendix specimens helps to confirm the diagnosis of appendicitis and also unravels other incidental pathologies that may impact on the management of patients. The consequences of unusual pathological findings in the literature include gastroenterology follow up, periodic surveillance, anti-tuberculosis medications, helminthic treatment, right colectomy and palliative care (21).
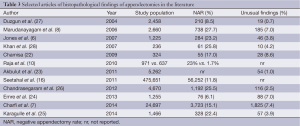
The incidence of unusual pathologies in our study is low (1.7%) and this is consistent with the findings in the literature (21-28) (Table 3). Unusual pathologies in our study include mucinous lesions, carcinoid tumor and granulomatous lesions suspicious for crohn’s disease which is consistent with findings reported in the literature. Documented unusual pathologies found on histological examination of resected appendix in the literature includes endometriosis, primary or secondary adenocarcinoma, neurofibroma, lymphomas, granulomatous conditions suspicious for tuberculosis and crohn’s disease, eosinophilic appendicitis, E.vermicularis and actinomycosis of the appendix (7,21,29,30). The observation of 1,825 unusual pathologies in the retrospective review of 24,697 appendectomy specimens is in support of the continued use of routine histopathological examination of resected appendix (7). A systematic review of 19 studies on the usefulness of routine histopathological examination of appendectomy specimens also observed that the incidence of unexpected findings in appendectomy specimens is low and intra-operative diagnosis alone appears insufficient for identifying unexpected disease and it is subject to great variation (21).
Full table
Conclusions
In conclusion, appendectomy in the female sex contributes to high NARs which may be lowered by utilizing combined clinical assessment and selective diagnostic imaging modalities. Unusual pathologies on histopathological examination of the appendix which could potentially impact on management of the patients justify the continued routine histopathological examination of resected appendix.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Hospital episodes Statistics. Admitted Patient Care, England. 2012-2013. Procedures and Interventions. Available online: http://www.hscic.gov.uk/catalogue/PUB12566/hosp-epis-stat-admi-proc-2012-13-tab.xlsx
- Addiss DG, Shaffer N, Fowler BS, et al. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 1990;132:910-25. [PubMed]
- Hale DA, Molloy M, Pearl RH, et al. Appendectomy: a contemporary appraisal. Ann Surg 1997;225:252-61. [PubMed]
- Zoarets I, Poluksht N, Halevy A. Does selective use of computed tomography scan reduce the rate of "white" (negative) appendectomy? Isr Med Assoc J 2014;16:335-7. [PubMed]
- Matthyssens LE, Ziol M, Barrat C, et al. Routine Surgical Pathology in General Surgery. Br J Surg 2006;93:362-8. [PubMed]
- Jones AE, Phillips AW, Jarvis JR, et al. The value of routine histopathological examination of appendicectomy specimens. BMC Surg 2007;7:17. [PubMed]
- Charfi S, Sellami A, Affes A, et al. Histopathological findings in appendectomy specimens: a study of 24,697 cases. Int J Colorectal Dis 2014;29:1009-12. [PubMed]
- Marudanayagam R, Williams GT, Rees BI. Review of the pathological results of 2660 appendicectomy specimens. J Gastroenterol 2006;41:745-9. [PubMed]
- SCOAP Collaborative, Cuschieri J, Florence M, et al. Negative appendectomy and imaging accuracy in the Washington State Surgical Care and Outcomes Assessment Program. Ann Surg 2008;248:557-63. [PubMed]
- Raja AS, Wright C, Sodickson AD, et al. Negative appendectomy rate in the era of CT: an 18-year perspective. Radiology 2010;256:460-5. [PubMed]
- Webb EM, Nguyen A, Wang ZJ, et al. The negative appendectomy rate: who benefits from preoperative CT? AJR Am J Roentgenol 2011;197:861-6. [PubMed]
- Slotboom T, Hamminga JT, Hofker HS, et al. Intraoperative motive for performing a laparoscopic appendectomy on a postoperative histological proven normal appendix. Scand J Surg 2014;103:245-8. [PubMed]
- Panagiotopoulou IG, Parashar D, Lin R, et al. The diagnostic value of white cell count, C-reactive protein and bilirubin in acute appendicitis and its complications. Ann R Coll Surg Engl 2013;95:215-21. [PubMed]
- Bijnen CL, Van Den Broek WT, Bijnen AB, et al. Implications of removing a normal appendix. Dig Surg 2003;20:115-21. [PubMed]
- Flum DR, Koepsell T. The clinical and economic correlates of misdiagnosed appendicitis: nationwide analysis. Arch Surg 2002;137:799-804; discussion 804. [PubMed]
- Seetahal SA, Bolorunduro OB, Sookdeo TC, et al. Negative appendectomy: a 10-year review of a nationally representative sample. Am J Surg 2011;201:433-7. [PubMed]
- Rao PM, Rhea JT, Rattner DW, et al. Introduction of appendiceal CT: impact on negative appendectomy and appendiceal perforation rates. Ann Surg 1999;229:344-9. [PubMed]
- Mariadason JG, Wang WN, Wallack MK, et al. Negative appendicectomy rate as a quality metric in the management of appendicitis: impact of computed tomography, Alvarado score and the definition of negative appendicectomy. Ann R Coll Surg Engl 2012;94:395-401. [PubMed]
- Raman SS, Osuagwu FC, Kadell B, et al. Effect of CT on false positive diagnosis of appendicitis and perforation. N Engl J Med 2008;358:972-3. [PubMed]
- Flum DR, McClure TD, Morris A, et al. Misdiagnosis of appendicitis and the use of diagnostic imaging. J Am Coll Surg 2005;201:933-9. [PubMed]
- Swank HA, Eshuis EJ, Ubbink DT, et al. Is routine histopathological examination of appendectomy specimens useful? A systematic review of the literature. Colorectal Dis 2011;13:1214-21. [PubMed]
- Chamisa I. A clinicopathological review of 324 appendices removed for acute appendicitis in Durban, South Africa: a retrospective analysis. Ann R Coll Surg Engl 2009;91:688-92. [PubMed]
- Akbulut S, Tas M, Sogutcu N, et al. Unusual histopathological findings in appendectomy specimens: a retrospective analysis and literature review. World J Gastroenterol 2011;17:1961-70. [PubMed]
- Emre A, Akbulut S, Bozdag Z, et al. Routine histopathologic examination of appendectomy specimens: retrospective analysis of 1255 patients. Int Surg 2013;98:354-62. [PubMed]
- Yabanoglu H, Caliskan K, Ozgur Aytac H, et al. Unusual findings in appendectomy specimens of adults: retrospective analyses of 1466 patients and a review of literature. Iran Red Crescent Med J 2014;16:e12931. [PubMed]
- Chandrasegaram MD, Rothwell LA, An EI, et al. Pathologies of the appendix: a 10-year review of 4670 appendicectomy specimens. ANZ J Surg 2012;82:844-7. [PubMed]
- Duzgun AP, Moran M, Uzun S, et al. Unusual findings in appendectomy specimens: evaluation of 2458 cases and review of the literature. Indian J Surg 2004;66:221-6.
- Khan OA, Morhan A, Jegatheeswaran S, et al. Routine pathological analysis of appendicectomy specimens – is it justified? Acta Chir Belg 2007;107:529-30. [PubMed]
- Ojo OS, Udeh SC, Odesanmi WO. Review of the histopathological findings in appendices removed for acute appendicitis in Nigerians. J R Coll Surg Edinb 1991;36:245-8. [PubMed]
- Lee SY, Kwon HJ, Cho JH, et al. Actinomycosis of the appendix mimicking appendiceal tumor: a case report. World J Gastroenterol 2010;16:395-7. [PubMed]


