What can we learn from AOANJRR 2014 annual report?
Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) was founded in 1998. It was introduced in a staged manner commencing in South Australia on the 1st of September, 1999 and fully implemented across the country by mid 2002. In June 2009, Federal Parliament passed legislation to enable the government to recover funding costs from the orthopaedic industry. All data is validated against information reported to the government and by using this approach the AOANJRR obtains information on over 98% of hip and knee replacements undertaken in Australia, which is almost a complete dataset of hip and knee replacements.
There are four types of data collected for each joint replacement. Type I data includes patient’s identification, basic patient details, type of joint replacement, primary or revision arthroplasty, details of the prostheses, and the identity of the hospital and surgeon. This data is the basic and minimum data set required, it also has been proven to be the most useful to date. It can be analyzed for survival rate/revision rate for different arthroplasties, which can be interpreted in all aspects of arthroplasty, particularly in the quality and utility of different prostheses. Type II data is about additional data on the patient, which includes: perioperative treatment (antibiotics and anticoagulants), comorbidities, the American Society of Anesthesiologists Physical Status classification system (ASAs) score, surgical approach, the use of computer-assisted surgery and many more. This data is widely collected by many joint registries and can provide useful clinic information that can direct clinical treatment perioperatively. Type III data includes post-operative clinical assessment as well as patient-reported pain, function and satisfaction. Type IV data includes radiographic data which is heavily utilised by surgeons. The usability of the later two types of data are not fully disclosed or extensively reported. This is due to the labour intensive requirements for collecting these two types of data. For this reason the last two types of data are usually the focus of institutional registries and not the national joint registry.
Many hospitals or medical care groups hold their own database for joint replacements, these institutional registries collect all types of data and can give precise and valuable information including reports of longitudinal institutional experience and individual case findings, which are especially useful for unusual complications or comorbidities. This data has been used to influence changes in clinical practice with improvement in clinical care. These institutional registries, therefore, are excellent platforms for clinical prospective and retrospective research. Compared to the institutional registries, the national joint registry has the ability to provide more valuable information for national health care insurance and policy makers, such as: (I) very detailed information on patterns of implant usage and performance; (II) surveillance of implants performance that is nation wide and across all surgeons; (III) identification of the behavior of new implants with the ability to detect earlier outlier implant performance, which is almost impossible using smaller institutional based registries. AOANJRR was the first registry to demonstrate the high failure rate of large head (greater than 32 mm) metal-on-metal (MOM) prostheses (1), this alarm was confirmed by other national registries and finally induced a worldwide recall of ASR by the Depuy Company as well as other large head MOM devices.
AOANJRR collects type I and II data for the annual national report, with the time of first revision and national mortality used as key measures, these data can estimate the revision rate of each procedure by Kaplan-Meier analysis, these results provide the guidance for health care policy of the Australian government. In the 2014 annual report, there are 891,208 primary and revision hip and knee replacements, which increased by 91,393 arthroplasties compared to the 2013 annual report. The annual report from AOANJRR shows the data and results from the previous year, it does not attempt to explain the meaning of these results, and allows for subjective interpretation of the results by different surgeons or groups depending on their personal understanding. Therefore, the following results are the data from authors’ views and readers are encouraged to interpret these results from their own experiences.
The 2014 annual report contains 410,767 hip replacements, with an additional 40,180 replacements compared to the 2013 annual report. Hip arthroplasty has gained great success after Charley invented the low-friction joint that was thought to be the greatest advance in orthopaedic surgery of the 20th century. With new philosophy, technique and implants, there have been some advancement in recent years, whether these new theoretic innovations correlate into real clinic advantage still under investigation. In this paper, we report on the results from AOANJRR and share our opinion on how they relate to best practice in China.
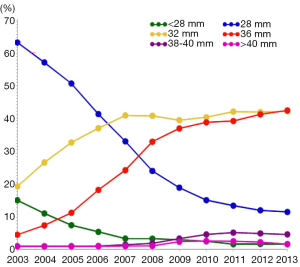
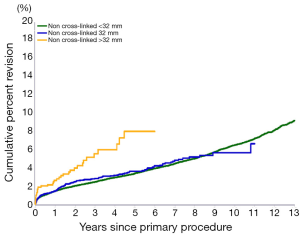
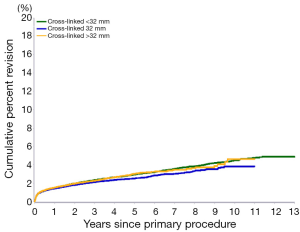
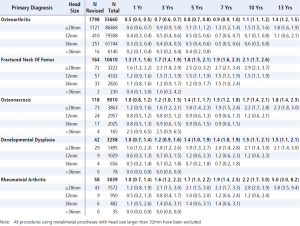
For total hip replacements, dislocation is the most common complication in first four years and the second most common complication overall (25.0%). Large femoral head size has been demonstrated to increase the stability of hip and decrease resultant dislocation rate. For this reason 32 and 36 mm femoral head sizes are now used more frequently for THA, and ≤28 mm heads has become much less common in recent years (Figure 1). Larger femoral heads are associated with thinner liners and increased wearing which are negative factors for survivorship. The introduction of cross-linked polyethylene has been beneficial to the outcome of THA. The AOANJRR reports that the rate of revision increases with head size for non cross-linked polyethylene implants. For cross-linked polyethylene, 32 mm head size has the lowest revision rate and there is no difference between less than 32 mm and greater than 32 mm (Figures 2,3). This phenomenon is also the same for ceramic on ceramic bearing surfaces. Furthermore, the results even show that head sizes larger than 32 mm are not associated with a reduced rate of revision for dislocation (Figure 4). Following these data and the reality of our country, we suggest 32 mm metal femoral heads are the treatment of choice for Chinese patients due to its relative lower price and better survival.
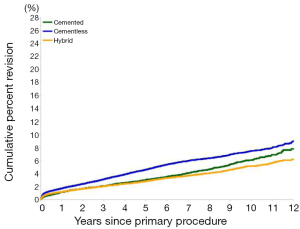
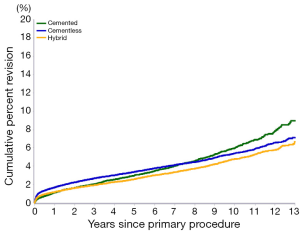
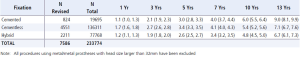
Over recent decades, the data from the joint registry supports cemented fixation. The 2013 report also showed cemented fixations had lower revision rates compared to cementless fixation (Figure 5). After advancements in surgical skills and technique as well as implant improvements, the 2014 report appears to provide a breaking point in this argument. The hybrid fixation is still the best choice in THA for OA, but cementless fixation demonstrates an advantage after 3 years (Figure 6). The cumulative revision at 13 years is 6.7% for hybrid, 7.1% for cementless and 9.0% for cemented fixation (Figure 7). Following these results, we suggest a cementless acetabular cup for all cases, and then surgeon’s preference for either a cemented or cementless femoral stem.
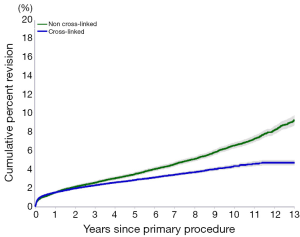
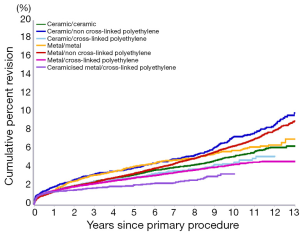
In the area of bearing surfaces, it has been demonstrated that the cross-linked polyethylene (XLPE) is superior to non cross-linked polyethylene (Figure 8), this advantage increases with time and the cumulative revision rate at thirteen years is 4.7% and 9.2% respectively. Although the ceramic bearing surface has large theoretical advantages of less wearing, this advantage has not correlated into clinic advantage, metal/XLPE has the lowest revision rate (4.7%) compared to the alternatives over a 13-year cumulative revision rate (Figure 9). Following these data and the reality of our country, we recommend a 32 mm metal femoral head with XLPE as the treatment of choice for Chinese patients because of its relative lower price and better survival.
The 2014 annual report contains 480,440 knee replacements, with an additional 51,212 replacements compared to the 2013 annual report. Although knee replacement is mature technique useful in treating many clinical problems for all kinds of patients, there are still some controversies to be resolved.
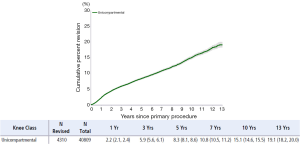
Unicompartmental knee arthroplasty (UKA) has become more and more popular in adult reconstruction, the advocators believe it is less invasive, allows quicker rehabilitation and better satisfaction compared with total knee replacements. Unicompartmental knee arthroplasty is rare in Australia compared with other countries in the world with only 41,250 (8.59%) over 13 years and the use of UKA continues to decline. In 2013, the number of UKA decreased by 2.7% compared to 2012 and 49.5% compared to 2003. As a percentage of all knee arthroplasties, UKA has decreased from 14.5% in 2003 to 4.1% in 2013. The reason for this phenomenon is that the revision rate of UKA is much higher than TKA, the cumulative revision rate of UKA’s undertaken for osteoarthritis was 19.1% at 13 years (Figure 10), and this revision rate is unacceptably high compared to TKAs (6.8% for OA at 13 years), The first reason for revision is not the progression of OA, which surgeons were concerned about, but the loosening/lysis of the prosthesis (45.3%).
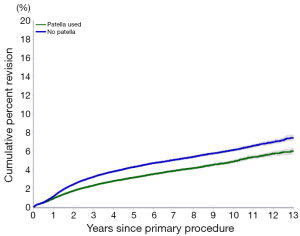
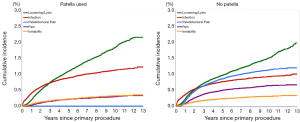
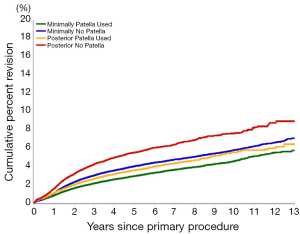
The need for patellar replacement in TKA is still a question that has not been solved over the decades. The 2013 annual report disclosed a lower rate of revision following primary total knee replacement when patellar prosthesis is used. This data has undergone detailed analysis in the 2014 annual report. For rheumatoid arthritis, the revision rate for patella replacement versus no patella replacement was 5.4% and 6.0% at 13 years respectively, which is of no statistical significance. For osteoarthritis, the revision rate for patella use versus no patella use was 6.0% and 7.4% respectively (Figure 11). The higher rate of revision when patella prosthesis is not used was due to, increased revision for patellofemoral pain, pain, and patella erosion, as patellofemoral pain was rare with a patella replacement (Figure 12).
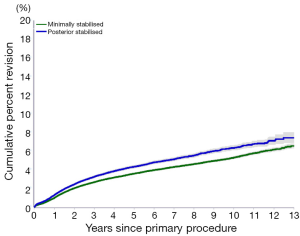
Whether the surgeon needs to resect the PCL during TKA has also been debated for decades. The choice for PCL resection affects the stability of the implants; cruciate retention (CR) implants have less stability than cruciate sacrificing (CS) implants. In China, CS implants are the more popular choice, but in Australia, CR implants are the first choice except for more complicated cases, the reason for this is the revision rate of CS implants is always higher than CR implants (Figure 13). When we consider both the stability of the knee and patella replacements, the results from the AOANJRR demonstrate that CR TKA with a patella replacement have the lowest revision rate compared to the other three combinations (Figure 14).
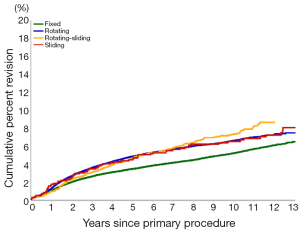
Fixed bearing prosthesis have been utilised in clinic for decades and produces wonderful results, but there exists a paradox between compatibility and constriction, higher compatibility brings out higher constriction which will cause greater loosening. Mobile bearing surfaces were invented to resolve this problem, allowing a combination of high compatibility while limiting constriction. Mobile bearing, therefore, theoretically appears to be the better choice in TKA. The AOANJRR reports do not support these theoretical merits. The data demonstrates that the revision rate of mobile bearing prostheses is higher than fixed bearing prostheses (Figure 15). This is the reason why fixed bearing is still the treatment of choice in Australia.
We have discussed some topics that continue to be widely debated worldwide, these topics have yet to reach a consensus and require further investigation. The data from the joint registry have many more cases than clinical trials and meta-analysis because they are generated from national databases, making the findings more compelling when the government formulates healthcare policy. In Australian public hospitals where the government covers all the healthcare expenses, the surgeon should use reliable implants and would be required to justify their reason for choosing an implant with higher revision rates. Although the data reports from the AOANJRR are not legally binding mandates dictating surgeon choice of prosthesis, they do give surgeons valuable information that cannot be elucidated through clinic trial and meta-analyses alone.
The joint registry does not give the surgeons the answers to all the clinical questions and the data from the joint registry cannot tell surgeons the functional outcomes of the operations. The joint registry also does not analyse all the radiographs during the operation and follow-up. The joint registry is not a good platform for clinic research as it can only give us retrospective data, although the data can be retrieved much more quickly than these through clinic trials. For this reason there will always be a need for ongoing clinical trials looking for answers to specific clinical questions.
A new difficult situation has been raised, the data in the AOANJRR regarding revision rate is calculated using Kaplan-Meier analysis, but in recent articles in Clinical Orthopaedic Related Research (CORR) some researchers have found the Kaplan-Meier analysis may overestimate the risk of revision in arthroplasty (2,3). Although we have not confirmed the conclusions from these articles, it is definitely a question worthy of further investigation. Fortunately, AOANJRR has reported on this problem and the need to consider competing risk with death particular as the follow up time increases. However, it is important to understand that the relative comparison remains whether or not the risk is overestimated as it is overestimated equally in all groups being compared.
Another limitation of this article is all the data analysed is from the AOANJRR, where the data is derived from Australia, which is inherently different to the Chinese race and culture. There are some differences between the two races, such as a higher BMI in Australia and a lower incidence of osteoarthritis in China where the main indications for THA is femoral neck fractures and femoral head avascular necrosis. Most of AOANJRR data is from THA for osteoarthritis and so there may be some differences in outcomes among different diagnoses. Furthermore, Chinese patients often have more serious deformities and functional problems prior to undergoing the total joint arthroplasty because of the differences in healthcare systems that also impacts on the results and revision rate of arthroplasties.
We must emphasize that our analysis and interpretation of the AOANJRR are based on the authors’ personal understanding and clinical knowledge. All the data are from AOANJRR 2014 annual report, the readers can download the free report from the official website and check the data you are interested in. We are happy to discuss differences of opinion if you have some alternative suggestions.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Graves SE, Rothwell A, Tucker K, et al. A multinational assessment of metal-on-metal bearings in hip replacement. J Bone Joint Surg Am 2011;93 Suppl 3:43-7. [PubMed]
- Martin CT, Callaghan JJ, Gao Y, et al. What Can We Learn From 20-year Followup Studies of Hip Replacement? Clin Orthop Relat Res 2015. [Epub ahead of print]. [PubMed]
- Lacny S, Wilson T, Clement F, et al. Kaplan-Meier Survival Analysis Overestimates the Risk of Revision Arthroplasty: A Meta-analysis. Clin Orthop Relat Res 2015. [Epub ahead of print]. [PubMed]