Robotic thoracic surgery of the right posterior inferior mediastinal mass
Clinical data
Medical history
The patient was admitted due to “a mediastinal mass found during health check-up four months ago”. Four months ago, she was admitted in a local hospital due to gas poisoning, during which CT showed a right posterior mediastinal mass. Later she was then discharged after the gas poisoning was resolved. She then visited our hospital for surgical treatment. She has a previous history of hypertension for 20 years and diabetes for 7 years. She underwent resection of uterine myoma 10 years ago.
Physical examination
No positive sign was detected during the physical examination at admission.
Auxiliary examination
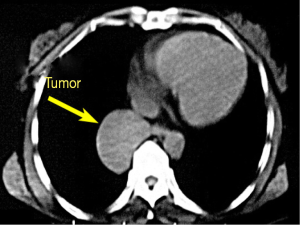
Chest CT: an ovoid cystic mass sized 5.5 cm × 4.0 cm was found at the right posterior inferior mediastinum. The lesion had homogenous density and smooth margin (Figure 1).
Pre-operative preparation
Conventional skin preparation was performed. The potential locations of the ports were marked on the skin.
Procedures
Anesthesia and body position
After the induction of general anesthesia, the patient was placed in a left lateral decubitus position under double-lumen endotracheal intubation. She was fixed in a Jackknife position, with the head slightly leaned forward.
Surgical procedures
- Incisions: a 1.2-cm camera port was created in the 5th intercostal space at right anterior axillary line. Two 0.8-cm working ports were created in the 3th intercostal space between the right middle axillary line and the posterior axillary line and in the 8th intercostal space between the posterior axillary line and the subscapular line, respectively (Figure 2).
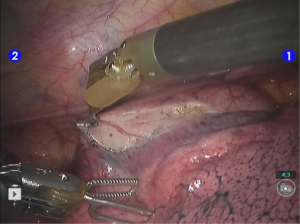
- Exploration of the thoracic cavity and insertion of the robot arms: the endoscopic airtight trocar was inserted through the camera port to establish 8-mmHg artificial pneumothorax, then the robotic endoscope was inserted for inspecting the thoracic cavity. Under the endoscopic monitoring, the robot trocars were separately inserted via the two working ports, so as to place the #1 robotic arm (right hand) and the #2 robotic arm (left hand). The #1 robotic arm was connected with the unipolar cautery hook, and the #2 robotic arm with fenestrated bipolar forceps (Figure 3).
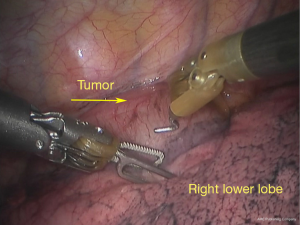
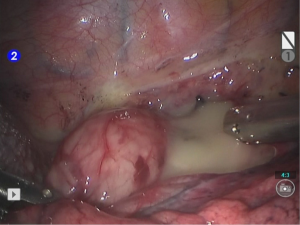
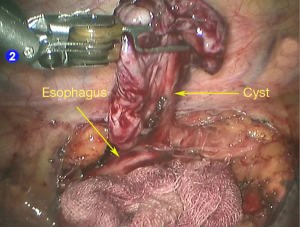
- Inspection of the lesion and its relationship with the neighboring tissues/organs: there was no adhesion or effusion inside the pleural cavity. The lesion was located in the right posterior inferior mediastinum and adhered to the posterior basal segment of the lower lobe of the right lung (Figure 4).
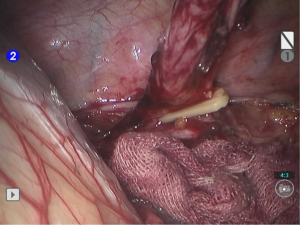
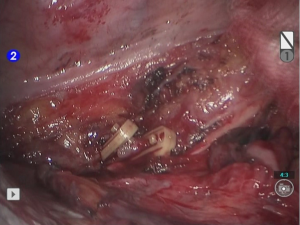
- Open the mediastinal pleura (Figure 5).
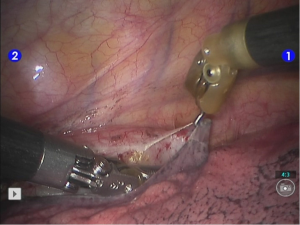
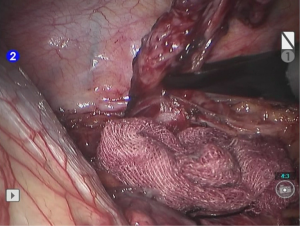
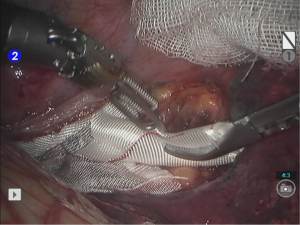
- Dissociate the tumor (Figures 6,7,8).
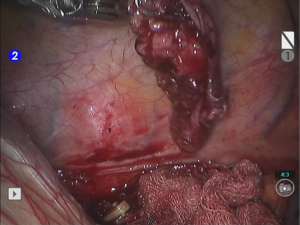
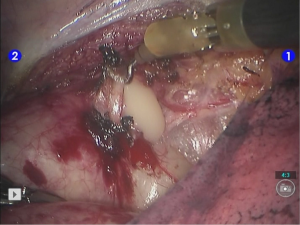
- Handle the esophagus adhesions (Figures 9,10).
- Resection of tumor (Figures 11,12).
- Hemostasis of the tumor bed (Figures 13,14).
- After the robot system was withdrawn, the thoracic drainage tube was indwelled at the camera port. Close the chest after sputum suctioning and lung recruitment. The intraoperative blood loss was about 10 mL; no blood was transfused.
Postoperative treatment
After the surgery, the patient received symptomatic treatment under routine general anesthesia. No antibiotic or hemostatic agent was applied.
Pathological diagnosis
The specimen was sized 4.0 cm × 2.0 cm × 1.0 cm. It had a grey-red surface, with cystic cutting margin. The cyst had smooth walls and was moderately hard. Pathological diagnosis was the right posterior mediastinal bronchogenic cyst.
Acknowledgements
Disclosure: The authors declare no conflict of interest.