
Combination of mini locking plate and nitinol arched shape-memory connector for purely lateral malleolus fractures: technique and clinical results
Introduction
Ankle fractures are among the most common skeletal injuries seen in clinical practice and constitute 3.92% of all fractures. With an annual incidence of up to 174 cases per 10,000 people, ankle fractures constitute 3.92% of all fractures (1-3). Purely lateral malleolus fractures, or isolated distal fibular fractures, account for 50.8% of ankle fractures and the incidence is increasing year by year (4).
For a long period of time, surgeons managed minimal displacement of lateral malleolus fractures using conservative treatment (5); however, based on a literature review, the majority of surgeons now prefer to use surgical treatment (6). Open reduction with internal fixation (ORIF) has become the gold standard treatment for these fractures (4,7). In recent years, according to the Biological Osteosynthesis (BO) principle, minimally invasive techniques with elastic fixation have been proposed (8,9).
Besides direct reduction of small fractures for plate insertion, stress stimulation is important for healing. By distributing, continuous, dynamic compression forces to the bone fragments through its two arms, the Nitinol (Ni-Ti) arched shape-memory connector (ASC) achieves the goal of accelerating fracture healing (10-12). Ni-Ti shape-memory alloys first appeared in the 1960s and have since been widely used in the neurosurgical (13), cardiovascular (14), and orthopedic fields (15). With its shape-memory effect, corrosion resistance, wear resistance, super-elasticity, and favorable biocompatibility, nitinol is an innovative material that has been used for internal fixation since the 1990s (12,13,15-17). Treatment that combines mini locking plates fixation with ASC meets the requirements of the BO principle, and could accelerate the healing process with minimal invasiveness. Furthermore, in view of the common skin irritation complications of lateral malleolus fractures, both mini locking plates and the ASC take up little space and can stimulate the skin to a minimum. Therefore, these combinations could represent a new advance in the orthopedic trauma field.
Because this new treatment has not been the focus of an article to date, the current study aimed to introduce the particularity of the ASC combined with mini locking plates and retrospectively evaluated the efficacy and clinical outcomes of the new treatment in purely lateral malleolus fractures. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/atm-20-4055).
Methods
Participants
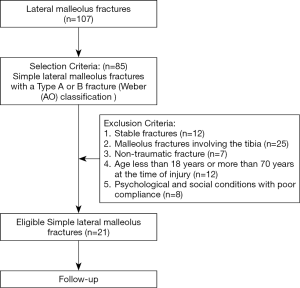
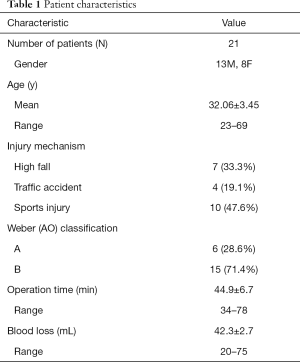
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Ethics of Biomedicine Research of Second Military Medical University. (NO.: 112012098) and informed consent was taken from all individual participants. Between January, 2015, and February, 2017, 107 patients with lateral malleolus fractures were assessed for eligibility. The inclusion criteria included simple lateral malleolus fractures with a Type A or B fracture [Weber (AO) classification]. The exclusion criteria were: (I) stable fractures; (II) malleolus fractures involving the tibia; (III) non-traumatic fracture; (IV) aged <18 years or >70 years at the time of injury; and (V) psychological and social conditions with poor compliance. Eventually, 21 patients (13 males, 8 females) were enrolled. A flowchart of the study is shown in Figure 1. The mean age of the patients was 32.06±3.45 years (range, 23–69 years). The causes of fracture were sports (10/21, 47.6%), a high fall (7/21, 33.3%), and traffic accidents (4/21, 19.1%).
Structure and working principles of the ASC
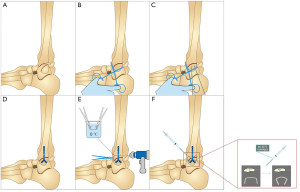
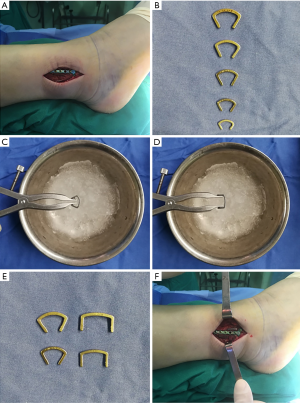
The ASC device (Lanzhou Ximai Memory Alloy Co., Ltd., Lanzhou, China) was designed for the desired feature of continuous compression to promote bone healing and manufactured with 2-mm-thick Ni-Ti shape-memory alloy (with a Ni content of 50–53%). The device memorizes the original cold-forging shape and can be restored to the pre-deformation shape by heating. The shape change quantity is about 8%. The device is processed with one-way thermal treatment and a 33±2 °C reversion temperature to connect the compression hooks and embracing arms with the main plate. Before implantation, the ASC is placed in 0–4 °C ice water for cooling to allow plastic deformation of the Ni-Ti alloy, as the ASC is malleable at lower temperatures (martensite phase). When the fixation is completed, 40–50 °C water is used to warm the device and stimulate its memory mechanical functions (austenite phase), which provides the continuous lateral compressive force. Simple illustrations of the mini-locking plate and ASC application process are shown in Figure 2 and the working process of the ASC is shown in the Video 1.

Surgical procedure
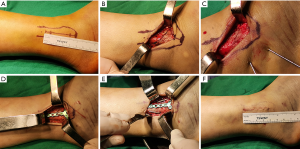
Under lumbar anesthesia, we took the lateral position of the patient’s fracture, placed an indwelling catheter, routinely disinfected it, and prepared a sterile surgical area for an anterolateral approach. A longitudinal lateral skin incision (<6 cm) was made to expose the periosteum of the fibula. After clearing necrotic bone debris and soft tissues, the damaged fibula was corrected through traction and held with bone forceps. Two Kirschner wires were crossed and implanted in the appropriate location for temporary fixation. The ASC was placed in ice water (0–4 °C) to enable the Ni-Ti alloy ability to be shaped. We selected a correctly shaped mini locking plate, pushing the plate toward the lateral border of the fibula and centering on the fibula with good bone contact. After definitive alignment, the locked screws were inserted into holes that were drilled avoiding the fracture line. Next, two holes were drilled on both the anterior and posterior sides of the fracture site; two ASCs were required for stable fixation, with the arms embedded in the holes. After being fixed into the bone, the ASCs were heated with 40–50 °C water to stimulate reversion of the fibula to its original shape. Figure 3 shows a schematic overview of all the procedures. The two arms of the ASCs generated a continuous compression force on the fracture line. The subcutaneous tissues and skin were closed in the usual manner. Active exercises with restricted weight lifting started on the first postoperative day. A gradual increase in weight and range of motion was then permitted; full weight lifting was permitted after clinical assessment of soft tissues and ankle function and X-ray evaluation. Bone healing was confirmed when the fracture area was pain-free and the cortices were bridged by visible callus in the anteroposterior and lateral views. Typical cases presented in Figure 4 and Figure 5.
Clinical outcomes evaluation
Follow-up and radiographic assessments were routinely performed at 4, 8, and 12 weeks after ASC implantation. Long-term postoperative review was conducted for 12–18 months. The follow-up radiographic images of one of the patients are shown in Figure 6. The American Orthopedic Foot and Ankle Society (AOFAS) score was used to evaluate impairments and activity limitations, comprising four different scores for pain, activity, functional limitations, and footwear, as well as examiner-reported data about alignment, gait, and motion (17). The patients were evaluated by AOFAS score after clinical healing during follow-up. All of the clinical assessments and evaluations of postoperative complications were performed by independent observers, and the results were independently interpreted by two senior attending doctors.

Statistical analysis
This study was a cross-sectional study. All data were counted the average and standard deviation were calculated using SPSS (20.0 version) software.
Results
The mean surgical time was 44.9±6.7 min (range, 34–78 min) and the average blood loss was 42.3±2.7 mL (range, 20–75 mL). All wounds healed uneventfully without deep or superficial skin infection. Based on postoperative radiographic assessment, the articular reduction of the lateral malleolus fractures was classified as anatomical (17 cases), acceptable (<2 mm step, 4 cases) or poor (>2 mm, 0 cases). None of the patients showed a postoperative articular gap or step >2 mm.
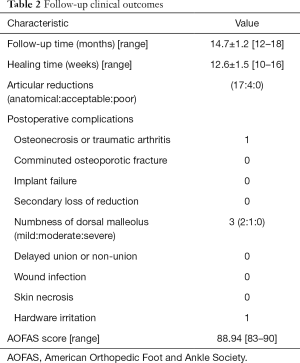
The patients were followed for an average of 14.7±1.2 months (range, 12–18 months). No patients showed loss of reduction, and all of the lateral malleolus fractures healed after an average of 12.6±1.5 weeks (range, 10–16 weeks). At the most recent follow-up, the mean AOFAS score was 88.94±1.2 (range, 83–90). The rate of complications in this study was 5/21 (23.8%); 3 patients felt numbness after the procedure, and 1 patient suffered from traumatic arthritis and hardware irritation. During follow-up, none o of the patients experienced severe complications such as comminuted osteoporotic fracture, implant failure, secondary loss of reduction, severe numbness of the dorsal malleolus, delayed union or non-union, skin necrosis, or wound infection. See Tables 1 and 2 for details.
Full table
Full table
Discussion
Purely lateral malleolus fractures comprise 50.8% of ankle fractures, and the incidence is rising annually (4). The bone defect of purely lateral malleolus fractures involves only the fibula, while the position of the talus (under the tibia) remains correct. Because the fibula plays an important role in maintaining the stability of the ankle joint, recovering the correct length, axis, and rotation of the distal fibula is crucial (18). Additionally, malpositioned fragments may impair blood vessels, which can lead to pseudoarthrosis. Therefore, except for cases in which no joint subluxation on radiographs or instability is found during stress examination, both of which have a low risk of displacement and can be safely treated by traditional conservative methods (19), operative treatments are now recommended for the majority of ankle fractures, including minimally displaced lateral malleolus fractures (6). In clinical practice, various operative treatments can be used to recover the anatomical structure of the fibular, though the most frequently used technique is ORIF (20).
Traditional ORIF, which is based largely by the Arbeitsgemeinschaft für Osteosynthesefragen (AO) concept, requires rigid compression plating and results in stiffness at the fracture site (21). ORIF aims to obtain reduction of the displaced fractures, to maintain anatomical alignment of the ankle joint, and to allow patients to start functional exercise as soon as possible, which is helpful for bone union. In most cases, ORIF is performed using compression screws and neutralization plates to meet the AO principle (20). Zahn introduced pre-contoured locking plates, which improved fixation in an osteoporotic bone model (22). Despite the accumulation of clinical experience, however, the management of lateral malleolus fractures is still challenging. Besides the long operation time, mechanical failure of traditional ORIF occurs in up to 14% of cases (23,24). The hardware removal rate is approximately 33% for traditional ORIF treatment, which increases the total cost of treatment per patient (25) and increases the rate of complications to 30% (20).
These complications occur for the following reasons. First, compression produced by traditional internal fixation is discontinuous, static, and passive. The mechanical compression produced by rigid implanted plates has the consequences of weak bone, which might be associated with non-union (21). Second, lateral malleolus fractures cause local swelling because of the thinner overlying skin and lack of skeletal muscle surrounding the fibula. Extensive soft tissue dissection is needed during the traditional operation to obtain precise fracture reduction and compression (26), which can lead to damage in the limited space and the rigid traditional implants have a high risk of complications such as wound dehiscence and infection, hardware prominence, neurovascular damage, and incision disunion (27,28). Furthermore, incorrect timing of the operation and application of standard large fragment plates have been associated with treatment failure because of steel plate exposure, joint pain or malformation, and even sepsis (25,29,30). All of these reports indicate that even if traditional ORIFis performed correctly, a high risk of wound complications requiring further surgical procedures still exists.
In response to these observations, the BO principle was put forward. In contrast to the original AO concept, the BO principle implies close reduction and elastic fixation to strike a balance between fracture stability and the integrity of soft tissue (8,9). Subsequently, many surgeons began to produce and evaluate plates with reduced stiffness and minimal invasiveness to accelerate the healing process. The minimally invasive treatment concept was developed as an alternative to the direct, open treatment method, avoiding major soft tissue complications such as neurovascular injuries and skin necrosis (18). The mini locking plate introduced in this study meets the BO principle, as does the minimally invasive treatment concept, which has been reported in many cases, such as clavicular and femoral fractures (31,32). With its flexibility and ingenious construction, the mini-locking plate can maximally preserve vascularization of intermediate fragments and provides minimal invasiveness for surgical intervention. In this study, the mini locking plate not only acted as an internal fixator, but also protected the surrounding soft tissues, needing only one nterolateral incision of 6 cm.
In addition to the mini-locking plate, an arched internal fixation device made of Ni-Ti shape-memory alloy was invented for compression broken ends of bones. With the biocompatibility and corrosion resistance superiority of the Ni-Ti shape-memory alloy, the ASC has been widely used in orthopedics and has beneficially improved both intraoperative and postoperative outcomes of fracture repair (15,33). Due to its characteristic of transforming its shape with temperature changes, the force produced by two arms of the ASC sufficiently stabilizes the fracture without any further management after implantation. Moreover, the ASC has high strength and low modulus, which effectively avoids the “stress shielding effect” (34). The results of follow-ups in the present study showed that this minimally invasive operation resulted in union in 100% of cases, post-operative complications in 11.3% of cases, and satisfactory AOFAS scores. These results are comparable to those in the literature (5).
Compared with conventional techniques, this new treatment has the following advantages. The mini plating system with its simple structure occupies less space and can thus only causes only minimal skin irritation and pain when the ankle joint begins early movement. Also, neurovascular injuries are reduced, further improving fracture union and decreasing removal rates. Compression obtained with an ASC is an evenly distributed, continuous, and dynamic force that can be transmitted across the fracture terminus, contributing to healing. Additionally, this technique only requires bone holding forceps for temporary fixation and an electric drill for drilling holes, which contributes to the simplicity of the procedure and results in a small amount of damage, a short operation time, and a low risk of vascular injury and blood loss. Thus, not only are the postoperative complications reduced but there is also a decreased need for secondary operations, especially metal removal, and increased patient satisfaction.
There are some limitations to this study. First, the diagnosis of lateral malleolus fracture was mainly dependent on X-ray imaging rather than computed tomography, which made misdiagnosis of lateral malleolus fracture more likely. Second, the ASC is a novel implant and relevant biomechanical testing and evaluation are still lacking. Finally, although the ASC showed good efficacy in this preliminary study, the sample size was small and the study design was retrospective. To better validate the efficacy of this surgical approach, a rigorous prospective study with a large sample size should be performed in the future.
Conclusions
Although our study is limited by the lack of a control group, the results suggested helpful treatment outcomes for the combination of mini locking plates and ASC fixation to treat purely lateral malleolus fractures. Based on the BO concept, mini locking plates are minimally invasive and strike a balance between fracture stability and soft tissue integrity. The ASC is not only an effective rigid device for multi-fragmented and comminuted fractures with rare hardware irritation but it also provides continuous concentrated compression to accelerate osseous healing. Therefore, this new treatment aids restoration, permitting early rehabilitation with a low incidence of postoperative complications.
Acknowledgments
Funding: We acknowledge the support of the National Science Foundation for Young Scientists of China (No. 81601910), the Shanghai Rising-Star Program (No. 18QA1405400), the Military Medical Research Foundation from the Naval Military Medical University (No. 2017JS15), and the China Postdoctoral Science Foundation Grant (No. 2016M592936).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-4055
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-20-4055
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-4055). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Ethics of Biomedicine Research of Second Military Medical University (No.: 112012098) and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Salai M, Dudkiewicz I, Novikov I, et al. The epidemic of ankle fractures in the elderly--is surgical treatment warranted? Arch Orthop Trauma Surg 2000;120:511-3. [Crossref] [PubMed]
- Pott P. Some few general remarks on fractures and dislocations. 1758. Clin Orthop Relat Res 2007.40-1. [Crossref] [PubMed]
- Goost H, Wimmer MD, Barg A, et al. Fractures of the ankle joint: investigation and treatment options. Dtsch Arztebl Int 2014;111:377-88. [PubMed]
- Koval KJ, Zhou W, Sparks MJ, et al. Complications after ankle fracture in elderly patients. Foot Ankle Int 2007;28:1249-55. [Crossref] [PubMed]
- Asloum Y, Bedin B, Roger T, et al. Internal fixation of the fibula in ankle fractures: a prospective, randomized and comparative study: plating versus nailing. Orthop Traumatol Surg Res 2014;100:S255-9. [Crossref] [PubMed]
- Palmanovich E, Brin YS, Laver L, et al. The effect of minimally displaced posterior malleolar fractures on decision making in minimally displaced lateral malleolus fractures. Int Orthop 2014;38:1051-6. [Crossref] [PubMed]
- Sanders DW, Tieszer C, Corbett B. Operative versus nonoperative treatment of unstable lateral malleolar fractures: a randomized multicenter trial. J Orthop Trauma 2012;26:129-34. [Crossref] [PubMed]
- Palmer RH. Biological osteosynthesis. Vet Clin North Am Small Anim Pract 1999;29:1171-85. vii. [Crossref] [PubMed]
- Sakhvadze S. Biological osteosynthesis as the treatment mode for multifragmental extra-articular fractures of lower limb long bones. Georgian Med News 2009.15-20. [PubMed]
- Zhang Y, Wang P, Xia Y, et al. Application of a Shape-Memory Alloy Concentrator in Displaced Patella Fractures: Technique and Long-Term Results. J Knee Surg 2017;30:166-73. [Crossref] [PubMed]
- Zhang Y, Zhao X, Tang Y, et al. Application of Ni-Ti alloy connector for the treatment of comminuted coronal plane supracondylar-condylar femoral fractures: a retrospective review of 21 patients. BMC Musculoskelet Disord 2013;14:355. [Crossref] [PubMed]
- Chen X, Liu P, Zhu X, et al. Design and application of nickel-titanium olecranon memory connector in treatment of olecranon fractures: a prospective randomized controlled trial. Int Orthop 2013;37:1099-105. [Crossref] [PubMed]
- Hoh DJ, Hoh BL, Amar AP, et al. Shape memory alloys: metallurgy, biocompatibility, and biomechanics for neurosurgical applications. Neurosurgery 2009;64:199-214; discussion 215. [PubMed]
- Levi DS, Kusnezov N, Carman GP. Smart materials applications for pediatric cardiovascular devices. Pediatr Res 2008;63:552-8. [Crossref] [PubMed]
- Vogt S, Tischer T, Blanke F. Biomaterials in orthopedics. Orthopade 2015;44:649-60. [Crossref] [PubMed]
- Sharma M, Sharma S. Comment on: shape memory Ni-Ti alloy swan-like bone connector for treatment of humeral shaft nonunion. Int Orthop 2010;34:1071. [Crossref] [PubMed]
- Kitaoka HB, Alexander IJ, Adelaar RS, et al. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 1994;15:349-53. [Crossref] [PubMed]
- Hess F, Sommer C. Minimally invasive plate osteosynthesis of the distal fibula with the locking compression plate: first experience of 20 cases. J Orthop Trauma 2011;25:110-5. [Crossref] [PubMed]
- McConnell T, Creevy W, Tornetta P 3rd. Stress examination of supination external rotation-type fibular fractures. J Bone Joint Surg Am 2004;86:2171-8. [Crossref] [PubMed]
- Jain S, Haughton BA, Brew C. Intramedullary fixation of distal fibular fractures: a systematic review of clinical and functional outcomes. J Orthop Traumatol 2014;15:245-54. [Crossref] [PubMed]
- Beltran MJ, Collinge CA, Gardner MJ. Stress Modulation of Fracture Fixation Implants. J Am Acad Orthop Surg 2016;24:711-9. [Crossref] [PubMed]
- Zahn RK, Jakubietz M, Frey S, et al. A locking contoured plate for distal fibular fractures: mechanical evaluation in an osteoporotic bone model using screws of different length. J Appl Biomech 2014;30:50-7. [Crossref] [PubMed]
- Beauchamp CG, Clay NR, Thexton PW. Displaced ankle fractures in patients over 50 years of age. J Bone Joint Surg Br 1983;65:329-32. [Crossref] [PubMed]
- White TO, Bugler KE, Appleton P, et al. A prospective randomised controlled trial of the fibular nail versus standard open reduction and internal fixation for fixation of ankle fractures in elderly patients. Bone Joint J 2016;98-B:1248-52. [Crossref] [PubMed]
- Lynde MJ, Sautter T, Hamilton GA, et al. Complications after open reduction and internal fixation of ankle fractures in the elderly. Foot Ankle Surg 2012;18:103-7. [Crossref] [PubMed]
- Litchfield JC. The treatment of unstable fractures of the ankle in the elderly. Injury 1987;18:128-32. [Crossref] [PubMed]
- Winkler B, Weber BG, Simpson LA. The dorsal antiglide plate in the treatment of Danis-Weber type-B fractures of the distal fibula. Clin Orthop Relat Res 1990.204-9. [PubMed]
- Lakhotia D, Sharma G, Khatri K, et al. Minimally invasive osteosynthesis of distal tibial fractures using anterolateral locking plate: Evaluation of results and complications. Chin J Traumatol 2016;19:39-44. [Crossref] [PubMed]
- Makwana NK, Bhowal B, Harper WM, et al. Conservative versus operative treatment for displaced ankle fractures in patients over 55 years of age. A prospective, randomised study. J Bone Joint Surg Br 2001;83:525-9. [Crossref] [PubMed]
- Vallier HA. Current Evidence: Plate Versus Intramedullary Nail for Fixation of Distal Tibia Fractures in 2016. J Orthop Trauma 2016;30 Suppl 4:S2-6. [Crossref] [PubMed]
- Ruchholtz S, El-Zayat B, Kreslo D, et al. Less invasive polyaxial locking plate fixation in periprosthetic and peri-implant fractures of the femur--a prospective study of 41 patients. Injury 2013;44:239-48. [Crossref] [PubMed]
- Zhang Y, Xu J, Zhang C, et al. Minimally invasive plate osteosynthesis for midshaft clavicular fractures using superior anatomic plating. J Shoulder Elbow Surg 2016;25:e7-12. [Crossref] [PubMed]
- Song K, Min T, Jung JY, et al. A superhydrophilic nitinol shape memory alloy with enhanced anti-biofouling and anti-corrosion properties. Biofouling 2016;32:535-45. [Crossref] [PubMed]
- Xin-wei L, Shuo-gui X, Chun-cai Z, et al. Biomechanical study of posterior wall acetabular fracture fixation using acetabular tridimensional memory alloy-fixation system. Clin Biomech (Bristol, Avon) 2010;25:312-7. [Crossref] [PubMed]


