Ultrasound features and the diagnostic strategy of subhepatic appendicitis
Introduction
EAES and WSES guidelines recommended to make a combination of “ultrasound” and “comprehensive clinical indicators” to form a clinical-imaging score could significantly improve the sensitivity and specificity of appendicitis diagnosis, and reduce the need for CT examinations in the diagnosis of acute appendicitis. Although the clinical-imaging score could significantly improve the accuracy and specificity of appendicitis diagnosis, the diagnosis of appendicitis remained to be a challenge and the clinical management of appendicitis was also in dispute (1). After review of the appendicitis surgery data in our hospital from January 2014 to January 2018, we found that the main reason for the missed diagnosis of appendicitis was the abnormal location of the appendix (the appendix located far away from the McBurney point). Subhepatic appendicitis is a common type of variation in the position of the appendix, with low morbidity and a high rate of missed diagnosis (2). The common type of abnormal appendicitis was subhepatic appendicitis. In this review and analysis, the diagnostic accuracy of subhepatic appendicitis in our hospital was only 11.1%. Due to the overhigh rate of missed diagnosis, we focused on the ultrasound diagnosis in subhepatic appendicitis. For open appendectomy (OA), the accurate diagnosis of subhepatic appendicitis by ultrasound and body surface positioning could help the surgeon find the best surgical incision in the upper right abdomen. For LA and SLA, the ultrasound could help the surgeon select a more easy-to-operate “hole”. This was a retrospective cohort study on the ultrasound features of subhepatic appendicitis. Combining the “20/80 rule” and “the Pareto principle”, this study made logical judgments on the combination of direct ultrasonic images with indirect ultrasonic images of subhepatic appendicitis and explored the diagnostic strategy of subhepatic appendicitis (3-5). The effective combination of statistical method and logical judgment method was an exploration of a whole new diagnostic mode in clinical study. The improvement of accuracy in the diagnostic of subhepatic appendicitis by ultrasound provided a basis for selection of surgical timing and surgical methods.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/atm-20-5265).
Methods
Patients
All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). This study was reviewed and approved by the Ethics Committee of Jizhong Energy Fengfeng Group Hospital and informed consent was taken from all the patients. Totally 1,591 patients with appendicitis who were treated at Jizhong Energy Fengfeng Group Hospital between January 2014 and January 2018 were analyzed, and 20 patients with subhepatic appendicitis, confirmed through an open appendectomy, or laparoscopic appendectomy, was selected as the population. Eighteen of the patients had complete clinical data and preoperative US data.
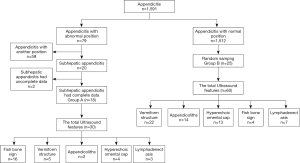
Inclusion criteria: for the group of patients with subhepatic appendicitis (Group A), cases with complete clinical data and ultrasound data were screened. For the group of patients with appendicitis with normal position (Group B). Appendicitis cases with complete data were numbered and entered in the SPSS 21.0 software, and then 25 cases were randomly selected (Figure 1).
Exclusion criteria for the study were: (I) patients without undergoing ultrasound examination before surgery; (II) patients with incomplete clinical data; (III) cases without having been confirmed through surgery; (IV) patients who are complicated by periappendiceal abscess and not fit for phase I surgical treatment; (V) Crohn’s disease; (VI) right-sided diverticulitis; (VII) right-sided segmental omental infarction; (VIII) appendiceal lesions with appendiceal mucocele.
Classification: the ultrasound-positive findings in Group A and Group B were sorted and classified on the screening results and clinical experience.
Equipment
Philips IU Elite Ultrasound System with L5–12 linear array probes and C1–5 sector probes, Philips HD15 Ultrasound System with L3–12 linear array probes and C1–5 sector probes, and HITACHI EUB-8500 Ultrasound System with 13-6 linear array probes and 5-2 sector probes were used.
Ultrasound techniques
During the ultrasound examination, the patients were instructed to lie in a supine position, with the abdomen exposed and a suitable amount of ultrasound gel applied. An abdominal ultrasound examination starts with the right lower abdomen. All the radiologists were trained on the standard operating procedure for acute abdominal ultrasound diagnosis.
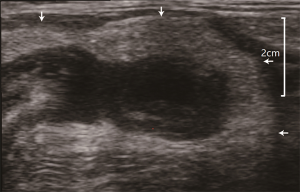
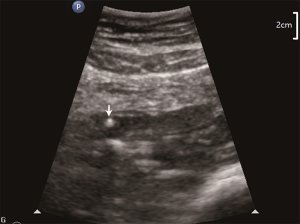
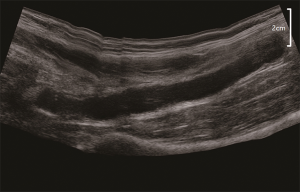
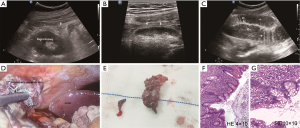
Variables for observation: (I) the fishbone sign: When the jejunum dilates in the lower abdomen, the small intestinal mucosa can be recognized, and jejunal villi can be recognized, presenting with fishbone-like ultrasound findings; (II) enlarged appendix: a vermiform structure in the right lower or upper abdomen, with a lumen diameter >6 mm and a wall thickness >2 mm (6,7); (III) the presence of lymphadenectasis in the abdominal cavity, with the ratio of the long axis-short axis <2 and the short axis >5 mm (8); (IV) appendicoliths: calcified fecal deposits that are known as appendicoliths, manifested as strong cloddy echoes with sound shadows behind on the ultrasound imaging (9-13); (V) hyperechoic omental cap: thickened oedematous omentum surrounding the appendix (Figures 2-5).
General clinical data
General clinical data include patient age, sex, body mass index (BMI), white blood cell (WBC), neutrophil percentage, body temperature, with or without the irritative symptoms of peritonitis, with or without signs of metastatic lower abdominal pain, and course of the disease.
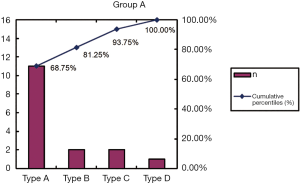
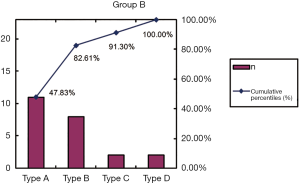
Pareto chart and the Pareto principle
The Pareto principle: factors with a cumulative distribution of 0% to 80% were primary, factors with a cumulative distribution of 80% to 90% secondary, and factors with a cumulative distribution of 90% to 100% general (14).
Pareto chart: a bar chart was drawn with the ultrasound findings of appendicitis as the X-coordinate and the number of patients with distinct types of appendicitis on the ultrasound imaging as the Y-coordinate. A broken line chart was drawn with the ultrasound findings of appendicitis as the X-coordinate and the cumulative percentage as the Y-coordinate. Afterward, the bar chart and the broken line chart were integrated with the Y-coordinate as the benchmark to form a Pareto chart.
Pathological classification of appendicitis
Pathological classification: (I) acute simple appendicitis; (II) acute phlegmonous appendicitis; (III) acute gangrenous appendicitis; and (IV) periappendiceal abscess (15,16). As patients with periappendiceal abscess are not fit for phase I surgical treatment, this type of patient is not included in this study.
Statistical methods
SPSS21.0 software was used for statistical analysis. Measurement variables were expressed in
Results
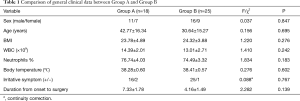
Comparison of general clinical data
Group A: sex (male/female): 11/7; age (42.77±16.34); BMI (23.78±4.89), WBC (14.39±2.01)×109; neutrophils % (76.74±4.03); body temperature (8.28±0.60) °C; irritative symptoms of peritonitis (+/−): 16/2; and duration from onset to surgery (7.33±1.78) days. The total of 30 accumulated ultrasound manifestations.
Group B: sex (male/female): 16/9; age (30.64±15.27); BMI (24.32±3.88); WBC (13.01±2.71)×109; neutrophils % (74.49±3.32); body temperature (38.41±0.57) °C; irritative symptoms of peritonitis (+/−): 25/1; and duration from onset to surgery (4.16±1.49) days. The total of 60 accumulated ultrasound manifestations.
P was greater than 0.05 for comparison between the two groups, showing that there were no statistically significant differences in the clinical data of the patients between the two groups (Table 1).
Full table
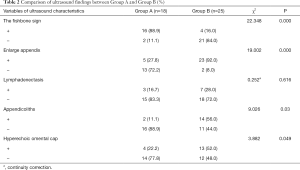
Comparison of ultrasound findings between Group A and Group B
Comparisons between the two groups showed an χ2=28.135 with a P value <0.05 for the fishbone sign of dilated ileum in the right lower abdomen, an χ2=16.245 with a P<0.05 for vermiform structure, an χ2=9.026 with a P<0.05 for appendicoliths, and an χ2=3.882 with a P<0.05 for hyperechoic omental cap, with statistical significance observed with differences in frequencies of the samples between the two groups. For whether there was a presence of lymphadenectasis, the comparison showed an χ2=0.753 with a P value of 0.386 greater than 0.05, indicating the difference in the frequency between the two groups was not statistically significant (Table 2).
Full table
The observed variables of statistical significance are screened out and ranked by the positive rate from highest to lowest as follows:
In Group A: the fishbone sign in the right lower abdomen (88.9%) > vermiform structure (27.8%) in the right upper abdomen > hyperechoic omental cap (22.2%) > appendicoliths (11.1%).
In Group B: vermiform structure in the right lower abdomen (92.0%) > appendicoliths (56.0%) > hyperechoic omental cap (52.0%) > dilated intestine in the right lower abdomen (16.0%).
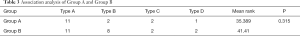
Appendicitis with normal position and subhepatic appendicitis is divided into A, B, C and D types for the two groups on the sequences of abnormal positive findings screened out using Chi-square test and on clinical experience
In Group A: Type A: the fishbone sign in the right lower abdomen; Type B: the fishbone sign in the right lower abdomen + vermiform structure in the right upper abdomen; Type C: the fishbone sign in the right lower abdomen + vermiform structure in the right upper abdomen + hyperechoic omental cap; and Type D: the fishbone sign in the right lower abdomen + vermiform structure in the right upper abdomen + hyperechoic omental cap + appendicoliths.
In Group B: Type A: vermiform structure in the right lower abdomen; Type B: vermiform structure in the right lower abdomen + appendicoliths; Type C: vermiform structure in the right lower abdomen + appendicoliths + hyperechoic omental cap; and Type D: vermiform structure in the right lower abdomen + appendicoliths + hyperechoic omental cap + the fishbone sign in the right lower abdomen.
Analysis using the contingency table for the ultrasonic classification: the mean rank was 41.41 for Group B and 35.389 for Group A, with a P value of 0.315, supporting the original hypothesis that the classification using the diagnostic strategy for Group A was consistent to that for Group B (Table 3).
Full table
Analysis of correlation between ultrasonic classification and pathological classification: in Group B, ultrasonic classification is positively correlated with pathological classification, with a Spearman’s correlation coefficient of 0.716. In Group A, ultrasonic classification is positively correlated with pathological classification, with a Spearman’s correlation coefficient of 0.747 (Table 4).

Full table
Pareto chart and the Pareto principle
Group A: Type A and Type B were the main ultrasound findings, with a cumulative percentage of 81.25%. Type A: the fishbone sign of the dilated small intestine in the right lower abdomen; Type B: the fishbone of the dilated small intestine in the right lower abdomen + vermiform structure in the right upper abdomen (Table 5; Figure 6).
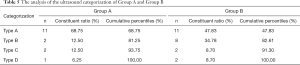
Full table
Group B: Type A and Type B were the main ultrasound findings, with a cumulative percentage of 82.61%. Type A: vermiform structure in the right lower abdomen; Type B: vermiform structure + appendicoliths (Table 5; Figure 7).
Discussion
Appendicitis is the most common surgical abdominal emergency in the developed world and developing world (17-21). Although anatomic variations are less common, most of the surprises encountered during an appendectomy are usually due to the various positions of the appendix. It is of great significance for surgeons and ultrasonographers to gain a full understanding of the appendix with an abnormal position (22-24).
Subhepatic appendicitis, also called appendicitis with a high position, refers to the inflamed appendix above the navel and is the most common type of appendicitis with the abnormal position (25-27) (Figure 2D). The development of the appendix is closely related to the development of the midgut. The primitive gut begins to develop at four weeks of gestation and can be divided into the foregut, midgut, and hindgut by the end of the fifth week. The first structures of the caecum and appendix become visible as bud of the caecum The appendix becomes visible in the eighth week of gestation. Colon stretching and elongation results in the descent of the caecum and vermiform appendix, pushing the appendix ahead of the caecum. In the postpartum period, the appendix and the caecum descend to the normal position. Subhepatic appendicitis primarily results from midgut malrotation, non-descent of the caecum, or is a result of free caecum (28-30).
Dilated jejunum is due to the widening of the jejunum and deposition of intestinal contents, with the intestinal mucosa displayed clearly against the background of the intestinal contents. It is primarily manifested as the fishbone sign on the ultrasound imaging (Figure 2C). It has a low display rate of only 8% in appendicitis with the normal position, but a display rate of up to 88.9% in subhepatic appendicitis. These results could be attributed to the following: (I) variation in the anatomic position: in subhepatic appendicitis, the colon moves up, and the jejunum rotates and aggregates in the right lower abdomen. The display rate of the ileum is high; (II) inflammatory stimulation: the inflammatory exudates of subhepatic appendicitis flow in the direction of gravity into the right lower abdomen, and paralysis is caused to the ileum due to inflammatory stimulation from the exudates, consequently resulting in reduced peristalsis and deposition of intestinal contents; (III) display of the small intestinal mucosa: the dilated small intestine can be displayed on the ultrasound imaging. The above factors lead to a high positive rate of the fishbone sign in the right lower abdomen in subhepatic appendicitis. The fishbone sign is also the main lead in the ultrasonic diagnosis of subhepatic appendicitis.
The vermiform structure is direct evidence for a diagnosis of appendicitis (Figure 5). When performed by ultrasonographers properly trained on acute abdominal ultrasound, appendicitis with the standard position was displayed by up to 90%. This figure shows the advantage of ultrasound in the diagnosis of appendicitis in a normal position. While in Group A, the display rate was only 27.8%. This difference could be attributed to the following: (I) the physician performing the examination was not familiar with subhepatic appendicitis, resulting in a decreased detection rate of subhepatic appendicitis; (II) significant anatomic variation exists with an appendix with a high position, for it can appear at any position in the abdominal cavity. The uncertainty of the anatomic position has increased the difficulty in locating the appendix; (III) the appendix with the high position is mostly located in posterior colon/jejunum, and gas present in the colon interferes with the display of the appendix.
Appendicoliths is the leading cause responsible for the acute onset of appendicitis (31-35) (Figure 4). In appendicitis with normal position (Group B), the display rate of appendicoliths could be up to 56% due to a fixed position of the appendix. While in subhepatic appendicitis (Group A), the display rate of appendicoliths was low due to the different anatomic position and impact of surrounding tissues. It was only 11.1%.
Hyperechoic omental cap is a manifestation of extra-intestinal fat inflammation. Accumulation of purulence in the appendiceal cavity increases pressure in the cavity, and the involvement of fats surrounding the appendix by inflammation leads to lipedema, with fats encapsulating around the appendix. The occurrence of a hyperechoic omental cap indicates the worsening of appendicitis. The display rate of the hyperechoic omental cap was 52.0% in Group B, and 22.2% in Group A. Hyperechoic omental cap helps localize inflammation. Subhepatic appendicitis is often complicated by an abnormal distribution of fats around the appendix, with incomplete fat encapsulation (Figure 3).
After a statistical comparison, the observed variable lymphadenectasis in the abdominal cavity was not included as a subject of this study, and it fulfills the diagnostic thinking. Appendiceal inflammation is not an independent correlation factor for lymphadenectasis. (I) Age is a confounding factor for the display of lymphadenectasis, which has a varying rate of display in different age groups, with a higher rate in the infants than in the adults. (II) Multiple abdominal disorders can lead to lymphadenectasis, including inflammatory bowel disease, gastrointestinal tumor, mesenteric lymphadenitis. The Pareto principle is also known as the 80/20 rule, the law of the vital few, or the principle of factor sparsity (36,37). The Pareto chart is a bar chart of frequencies sorted by frequency. The most commonly used incarnation of the chart puts the highest bars on the left and includes a line showing the scores produced by adding the heights in order from left to right. This chart is used widely in quality control settings to find critical factors leading to failure or defects in a process. The Pareto chart principle is widely applied in the management, and applying this principle can show the leading factors of the problem efficiently and objectively. We applied this principle in finding the leading factors for ultrasonic findings of subhepatic appendicitis in this study, which was a combination of statistics and management. This principle was used to summarize the diagnosis of subhepatic appendicitis: only 20% of ultrasound-positive features were presented in 80% of the patients with subhepatic appendicitis (38-42).
In subhepatic appendicitis (Group A), the main types of ultrasound findings are (I) dilated ileum in the right lower abdomen, and (II) dilated ileum in the right lower abdomen + vermiform structure in the right upper abdomen. Dilated ileum in the right lower abdomen is the main, leading to the diagnosis of subhepatic appendicitis. In the case of clinical data of suspicious appendicitis, the surgeon and the ultrasonographer should consider the possibility of subhepatic appendicitis and perform a careful scan examining whether there are echoes of vermiform structure in the right upper abdomen when dilated ileum is seen in the right lower abdomen, to avoid a missed diagnosis of subhepatic appendicitis.
In appendicitis with normal position (Group B), the main types of ultrasound findings are as follows: (I) vermiform structure in the right lower abdomen; and (II) vermiform structure in the right lower abdomen + appendicoliths observed in the vermiform structure. Dilated ileum in the right lower abdomen was a general factor in appendicitis with a normal position. In other words, the possibility of dilated ileum occurring in appendicitis with the normal position is low. It may only exist in cases of serious exudation from the appendix causing small intestinal paralysis.
Currently, laparoscopic appendectomy (LA) was the main treatment for acute appendicitis. Mini-incision open appendectomy (MOA), single port laparoscopic appendectomy (sLA) and (Natural orifice transluminal endoscopic surgery (NOTES) via various methods were also the treatments. The treatments for normal appendicitis and subhepatic appendicitis were basically in consistency, for which the surgical excision was recommended. However, the positions of surgical incisions between the two were different. For normal appendicitis, generally appendectomy was conducted at the McBurney point in the right lower abdomen. For subhepatic appendicitis, the best surgical approach needed to be in the near location after positioning of body surface by ultrasound. When selecting LA, for subhepatic appendicitis, the body surface projection was needed to be labelled under the guidance of ultrasound. The surgeon selected the best position of the puncture hole for the laparoscope according to the projection position of body surface. The diagnosis of subhepatic appendicitis could improve the cure rate, select the most suitable surgical approach, shorten the operation time, and ensure patient’s safety to the greatest extent.
When it is suspected to be subhepatic appendicitis through “comprehensive clinical indicators”, each ultrasound feature is of great significance to the diagnosis of subhepatic appendicitis. The more cumulative positive ultrasound features, the higher the diagnostic accuracy. Combined with the 20/80 rule, when comprehensive clinical indicators support appendicitis with fishbone sign been found by ultrasound scan of the right lower abdomen, the ultrasound physician shall consider whether it is subhepatic appendicitis. At this time, the upper right abdomen needs to be carefully scanned for evidence of subhepatic appendicitis by the examiner. The purpose of study on ultrasound features of subhepatic appendicitis is to improve the diagnosis accuracy of subhepatic appendicitis and allow patients with subhepatic appendicitis to receive timely treatment.
Conclusions
This study has summarized the ultrasonic diagnostic procedure for subhepatic appendicitis. This procedure can achieve a similar diagnostic effect as the procedure for appendicitis with a normal position. The presence of an abnormally dilated ileum in the right lower abdomen − the fishbone sign, is the first lead to the diagnosis of subhepatic appendicitis.
A specialized diagnostic strategy for subhepatic appendicitis for patients with clinically suspicious appendicitis when a vermiform structure is not scanned in the right lower abdomen and only dilated ileum (the fishbone sign) should be utilized. A scan focusing on determining whether there is a presence of vermiform structure in the right upper abdomen should be performed, and the possibility of subhepatic appendicitis should not be ruled out even if the presence of the appendix with the high position is discovered.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-5265
Data Sharing Statement: Available at http://dx.doi.org/10.21037/atm-20-5265
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-5265). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). This study was reviewed and approved by the Ethics Committee of Jizhong Energy Fengfeng Group Hospital and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gorter RR, Eker HH, Gorter-Stam MA, et al. Diagnosis and management of acute appendicitis. EAES consensus development conference 2015. Surg Endosc 2016;30:4668-90. [Crossref] [PubMed]
- Friday JH. Update on appendicitis: diagnosis and presurgical management. Curr Opin Pediatr 2006;18:234-8. [Crossref] [PubMed]
- Thompson GC, Schuh S, Gravel J, et al. Variation in the Diagnosis and Management of Appendicitis at Canadian Pediatric Hospitals. Acad Emerg Med 2015;22:811-22. [Crossref] [PubMed]
- Craner DR, Wexler JI, Nalugo M, et al. Bringing Surgeons Together Across the World: Diagnosis and Management of Acute Appendicitis. J Laparoendosc Adv Surg Tech A 2015;25:261-5. [Crossref] [PubMed]
- Rice-Townsend S, Barnes JN, Hall M, et al. Variation in Practice and Resource Utilization Associated With the Diagnosis and Management of Appendicitis at Freestanding Children's Hospitals: Implications for Value-Based Comparative Analysis. Ann Surg 2014;259:1228-34. [Crossref] [PubMed]
- Alter SM, Walsh B, Lenehan PJ, et al. Ultrasound for Diagnosis of Appendicitis in a Community Hospital Emergency Department has a High Rate of Nondiagnostic Studies. J Emerg Med 2017;52:833-8. [Crossref] [PubMed]
- Franca Neto AH, Amorim MM, Nóbrega BM. Acute appendicitis in pregnancy: literature review. Rev Assoc Med Bras (1992) 2015;61:170-7. [Crossref] [PubMed]
- Sonawane R, Jatkar G, Chaudhari M. Correlation of ultrasonography findings of acute appendicitis with pathological acute appendicitis. Int Surg J 2016;3:1447-50. [Crossref]
- Dehghan A, Moaddab AH, Mozafarpour S. An unusual localization of trichobezoar in the appendix. Turk J Gastroenterol 2011;22:357-8. [Crossref] [PubMed]
- Robb AL, Ali S, Poonai N, et al. Pain management of acute appendicitis in Canadian pediatric emergency departments. CJEM 2017;19:417-23. [Crossref] [PubMed]
- Horn CB, Tian D, Bochicchio GV, et al. Incidence, demographics, and outcomes of nonoperative management of appendicitis in the United States. J Surg Res 2018;223:251-8. [Crossref] [PubMed]
- GlobalSurg Collaborative. Laparoscopy in management of appendicitis in high-, middle-, and low-income countries: a multicenter, prospective, cohort study. Surg Endosc 2018;32:3450-66. [Crossref] [PubMed]
- Jacob R, Krauss B, Twito G, et al. Emergency department pain management in children with appendicitis in a Biethnic population. Clin J Pain 2017;33:1014-8. [Crossref] [PubMed]
- Qu Z, Dalton C, Blough J, et al. Validation of Pareto Principle ("20/80 Rule") in Surgical Pathology to Gain Insight Into Specimen-Diagnosis Profile. Am J Clin Pathol 2015;144:A176. [Crossref]
- Cho J, Lee D, Sung K, et al. Clinical implication of discrepancies between surgical and pathologic diagnoses of acute appendicitis. Ann Surg Treat Res 2017;93:43-9. [Crossref] [PubMed]
- Carr NJ. The pathology of acute appendicitis. Ann Diagn Pathol 2000;4:46-58. [Crossref] [PubMed]
- Aydin D, Turan C, Yurtseven A, et al. Integration of radiology and clinical score in pediatric appendicitis. Pediatr Int 2018;60:173-8. [Crossref] [PubMed]
- Mikaere H, Zeng I, Lauti M, et al. Derivation and validation of the APPEND score: an acute appendicitis clinical prediction rule. ANZ J Surg 2018;88:E303-E307. [Crossref] [PubMed]
- Aceti V, Boscarelli A. Burying the appendiceal stump during appendicectomy: state of art. Transl Pediatr 2018;7:73-4. [Crossref] [PubMed]
- Pacharn P, Ying J, Linam LE, et al. Sonography in the evaluation of acute appendicitis: are negative sonographic findings good enough? J Ultrasound Med 2010;29:1749-55. [Crossref] [PubMed]
- Ahn SE, Moon SK, Lee DH, et al. Sonography of Gastrointestinal Tract Diseases: Correlation with Computed Tomographic Findings and Endoscopy. J Ultrasound Med 2016;35:1543-71. [Crossref] [PubMed]
- Sanchez TR, Corwin MT, Davoodian A, et al. Sonography of Abdominal Pain in Children: Appendicitis and Its Common Mimics. J Ultrasound Med 2016;35:627-35. [Crossref] [PubMed]
- Xu Y, Jeffrey RB, Chang ST, et al. Sonographic Differentiation of Complicated From Uncomplicated Appendicitis: Implications for Antibiotics-First Therapy. J Ultrasound Med 2017;36:269-77. [Crossref] [PubMed]
- Xu Y, Jeffrey RB, Shin LK, et al. Color Doppler Imaging of the Appendix: Criteria to Improve Specificity for Appendicitis in the Borderline-Size Appendix. J Ultrasound Med 2016;35:2129-38. [Crossref] [PubMed]
- Chiapponi C, Jannascha O, Petersena M, et al. A rare case of perforated "sub-hepatic appendicitis" - a challenging differential diagnosis of acute abdomen based on the combination of appendicitis and maldescent of the caecum. Pathol Res Pract 2017;213:75-8. [Crossref] [PubMed]
- Singh R. Subhepatic appendicitis: diagnostic dilemma: a case report. Int Surg J 2016;3:422-4. [Crossref]
- Sinha A, Cukkemane A, Saini V. Study of different positions of appendix in operated cases of appendicitis in rural hospital and its clinical correlation. Journal of Evidence Based Medicine and Healthcare 2017;4:1420-4. [Crossref]
- Ahmed I, Asgeirsson KS, Beckingham IJ, et al. The position of the vermiform appendix at laparoscopy. Surg Radiol Anat 2007;29:165-8. [Crossref] [PubMed]
- Chauhan S, Anand S. Intracecal appendix: an extremely rare anatomical variation. A case report and review of literature. Surg Radiol Anat 2018;40:111-4. [Crossref] [PubMed]
- Nayak BS. Why the tip of vermiform appendix has variable position? Med Hypotheses 2010;75:682-3. [Crossref] [PubMed]
- Resanovic V, Resanovic A, Krstic S, et al. Acute Appendicitis: Still a Surgical Disease? Results from a Propensity Score-Based Outcome Analysis of Conservative Versus Surgical Management from a Prospective Database. World J Surg 2018;42:903-4. [Crossref] [PubMed]
- Lipsett SC, Bachur RG. Current Approach to the Diagnosis and Emergency Department Management of Appendicitis in Children. Pediatr Emerg Care 2017;33:198-203. [Crossref] [PubMed]
- Rothrock SG, Pagane J. Acute appendicitis in children: emergency department diagnosis and management. Ann Emerg Med 2000;36:39-51. [Crossref] [PubMed]
- Simillis C, Symeonides P, Shorthouse AJ, et al. A meta-analysis comparing conservative treatment versus acute appendectomy for complicated appendicitis (abscess or phlegmon). Surgery 2010;147:818-29. [Crossref] [PubMed]
- Slotta JE, Kopsch U, Ghadimi M, et al. Management of acute appendicitis: evidence for prompt surgical treatment? Chirurg 2017;88:503-11. [Crossref] [PubMed]
- Warner CJ, Walsh DB, Horvath AJ, et al. Lean principles optimize on-time vascular surgery operating room starts and decrease resident work hours. J Vasc Surg 2013;58:1417-22. [Crossref] [PubMed]
- Davies P. Time to acknowledge the workings of the 80/20 principle? Br J Gen Pract 2005;55:55-6. [PubMed]
- Delibegović S, Mehmedovic Z. The influence of the different forms of appendix base closure on patient outcome in laparoscopic appendectomy: a randomized trial. Surg Endosc 2018;32:2295-9. [Crossref] [PubMed]
- Lee M, Kim SC. Appendiceal foreign body in an infant. Medicine (Baltimore) 2017;96:e6717. [Crossref] [PubMed]
- Müller F, Dormann H, Pfistermeister B, et al. Application of the Pareto principle to identify and address drug-therapy safety issues. Eur J Clin Pharmacol 2014;70:727-36. [Crossref] [PubMed]
- Greenwood TJ, Lopez-Costa RI, Rhoades PD, et al. CT Dose Optimization in Pediatric Radiology: A Multiyear Effort to Preserve the Benefits of Imaging While Reducing the Risks. Radiographics 2015;35:1539-54. [Crossref] [PubMed]
- Cruz-Ramírez M, Hervás-Martínez C, Fernández J, et al. Predicting patient survival after liver transplantation using evolutionary multi-objective artificial neural networks. Artif Intell Med 2013;58:37-49. [Crossref] [PubMed]
(English Language Editor: J. Chapnick)