
Obesity and its effect on outcomes in same-day bilateral total knee arthroplasty
Introduction
Obesity has a negative impact on the body in a multitude of ways, including a six-fold increase in risk for knee osteoarthritis (1). As such, many patients with increased body mass indices (BMI) will present to providers with bilateral disease, with some necessitating total knee arthroplasties (TKA) (2). To avoid the morbidity of multiple operations, same-day bilateral total knee arthroplasty (sd-BTKA) may be an option for these patients, as some find appeal in a single surgery and hospitalization (3,4). Moreover, physicians may acquiesce to the procedure as investigations report decreased cumulative hospital stays and rehabilitation time (5-10). Despite the purported benefits of this procedure, studies have revealed increased risk for negative outcomes with the bilateral operation (9-13). As a consequence of the conflicting body of literature, the utility of sd-BTKA continues to generate debate amongst arthroplasty surgeons (14-16).
Over time, the debate regarding sd-BTKA intensified to a level that warranted consensus recommendations in 2013 (4). Among several proposals, the presence of certain comorbidities, such as morbid obesity, were felt to warrant exclusion of individuals from consideration for the operation. This notion is predicated off studies identifying higher BMI patients as having an increased risk for complications when undergoing unilateral TKA (17-23), though several studies have demonstrated a lack of association between poor outcomes and high BMI (24-28). Ultimately, whether high BMI patients should be subjected to the cumulative risk of two unilateral TKAs or the single operation of sd-BTKA remains inconclusive, as no studies have investigated the prospect.
To date, there is a shortage of studies that have quantified the role of high BMI in patients undergoing sd-BTKA. Specifically, no study has evaluated the effect elevated BMI has on the outcomes of this procedure when compared to non-obese patients. Therefore, this study will compare (I) incidence, (II) demographics, and (III) outcomes of non-obese, obese, and morbidly obese sd-TKA patients in the United States from 2009 to 2016. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/atm-20-806).
Methods
Database
The National Inpatient Sample (NIS) database was queried for all individuals who underwent sd-BTKA from 2009 to 2016. The NIS is a large, publicly available database gathered by the Agency for Healthcare Research and Quality (AHRQ) for the Healthcare Cost and Utilization Project (HCUP), which was created with the goal of improving health care delivery. The unweighted NIS database contains seven million hospital stays each year. When weighted, it represents approximately 35 million hospitalizations nationally (29).
Patient selection
Using International Classification of Diseases, Ninth and Tenth Editions (ICD-9 and -10) procedural codes (ICD-9: ‘81.54’; ICD-10: ‘0SRC069’, ‘0SRC06A’, ‘0SRC06Z’, ‘0SRC0J9’, ‘0SRC0JA’, ‘0SRC0JZ’, ‘0SRC0KZ’, ‘0SRD069’, ‘0SRD06A’, ‘0SRD06Z’, ‘0SRD0J9’, ‘0SRD0JA’, ‘0SRD0JZ’, ‘0SRD0KZ’), an initial query was made to the NIS for those undergoing sd-BTKA. This was achieved by tallying patients who presented more than one TKA code (n=245,139). We then stratified patients into non-obese, obese (BMI >30 kg/m2; ICD-9: ‘278.00’, ‘278.03’; ICD-10: ‘E66.09’, ‘E66.1’, ‘E66.8’, ‘E66.9’) and morbidly obese (BMI >40 kg/m2; ICD-9: ‘278.01’; ICD-10: ‘E66.01’, ‘E66.2’) cohorts utilizing their respective diagnosis codes. As this study was retrospective and utilized a deidentified database, it was deemed exempt from Institutional Review Board approval.
Variables
Patient variables included mean age, mean length of stay (LOS), sex, race, primary payer, age-adjusted Charlson Comorbidity Index (ACCI) score, and discharge disposition. Length of stay was defined as the stay from admission until discharge. Race was categorized into Caucasian, African American, Hispanic, Asian, Native American, and other. Primary payer included Medicare, Medicaid, private insurance, self-pay, no charge, and others. The ACCI is a prognostic tool employed to estimate 10-year mortality based on 19 comorbid conditions and is categorized in accordance with the number of present comorbidities, namely 0, 1, 2, or 3+ (30). Discharge disposition was categorized into routine, short-term hospital, skilled nursing facility, home with home health care, against medical advice, and deceased.
The analyzed outcomes included charges, costs, and complications. Charges represented the monetary amount the hospital billed to the payer, while costs represented the monetary amount the hospital facility incurred for the inpatient stay. The charges associated with hospitals are an element recorded within the NIS database; although costs are not. In order to obtain costs, the yearly “Cost-to-Charge Ratio” supplemental files provided by HCUP were utilized (29). All costs and charges were adjusted using the January 1, 2019 consumer price index. Complications included myocardial infarctions (MI), cardiac arrests, pulmonary emboli (PE), deep vein thromboses (DVT), cerebrovascular complications, sepsis, periprosthetic joint infections (PJI), hematomas/seromas, mechanical complications, respiratory failures, pneumoniae, urinary tract infections (UTI), and blood transfusions. Cerebrovascular complications consisted of thromboses, emboli, or occlusions with or without cerebral infarction and/or hemorrhage. Mechanical complications represented intraoperative or perioperative fractures, mechanical breakdown, loosening, or dislocation of implants.
Statistical analysis
Chi-square analyses were used to analyze race, ACCI, primary payer, median household income, discharge destination, and complications. Student’s t-tests were performed to compare age, LOS, costs, and charges. Odds ratios for complications were determined by employing multinomial regression analyses. To reduce the chance of committing type I (alpha) error and more precisely identify statistical significance, post-hoc Bonferroni corrections were utilized. All analyses were conducted using the Statistical Package for the Social Sciences (SPSS®; IBM Corporation; Armonk, New York) version 25. A P value of 0.05 was considered the threshold for significance for all variables.
Results
Incidence
Non-obese patients [n=184,844 (75.4%)] comprised the highest percentage of sd-BTKA procedures over the course of the study, which was followed by obese [n=39,901 (16.3%)] and then morbidly obese [n=20,397 (8.3%)] patients (Table 1).

Full table
Patient demographics
Age decreased, mean LOS increased, and proportion of females increased as BMI increased (P<0.001 for all). Caucasians were the most common race undergoing sd-BTKA, although the proportion of African Americans increased as BMI increased (P<0.001). The number of individuals with an ACCI of 3+ decreased as obesity status increased, while those with ACCI statuses of 1 and 2 increased as BMI increased (P<0.001). The most common payer was private insurance, which increased in proportion as BMI increased (P<0.001). Median household income quartiles 3 and 4 significantly decreased among morbidly obese individuals (P<0.001). Proportion of discharges to skilled nursing facilities increased as BMI increased (P<0.001).
Outcomes
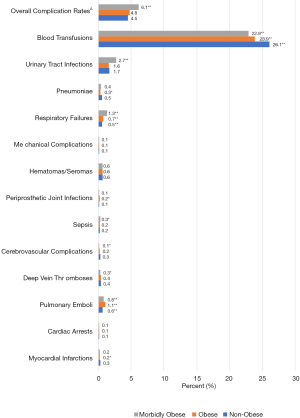
Hospital costs and charges increased as BMI increased (P<0.001 for both) (Table 2). In comparison with the non-obese patients, obese patients demonstrated significantly lower proportions of MIs (P=0.028), pneumoniae (P<0.001), and blood transfusions (P<0.001), while demonstrating significantly higher proportions of PE (P<0.001), respiratory failures (P<0.001), and PJIs (P=0.028) (Figure 1). For morbidly obese patients, significantly lower proportions were observed in DVTs (P=0.022), cerebrovascular complications (P=0.002), and blood transfusions (P<0.001), while significantly higher proportions were observed regarding PE (P<0.001), sepsis (P<0.001), respiratory failures (P<0.001), and UTIs (P<0.001). Only morbidly obese patients demonstrated a significantly increased overall complication rate compared to non-obese patients (P<0.001).
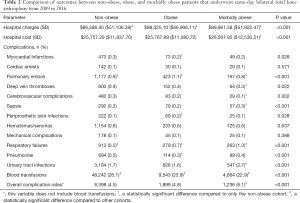
Full table
Multinomial regression analysis
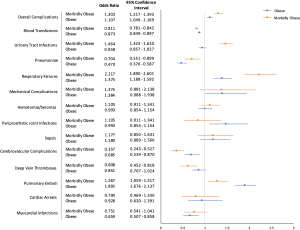
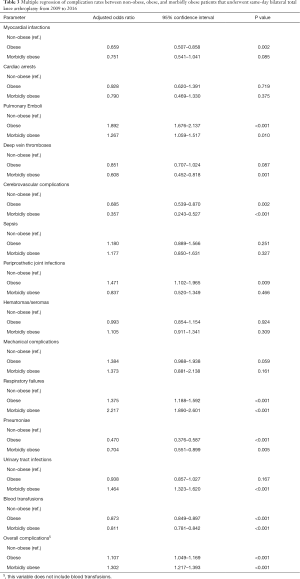
When compared to non-obese patients, obese patients had a significantly reduced risk for MIs [odds ratio (OR): 0.659], cerebrovascular complications (OR: 0.685), pneumoniae (OR: 0.470), and blood transfusions (OR: 0.873) (P<0.003 for all) (Figure 2; Table 3). Conversely, obese patients were at increased risk for PE (OR: 1.892), PJIs (OR: 1.471), and respiratory failures (OR: 1.375) (P<0.011 for all). Obese patients also demonstrated a slight, yet significant, overall increase in complication risk (OR: 1.107) when compared to non-obese patients (P<0.001).
Full table
When morbidly obese patients were compared to non-obese patients, they had a significantly reduced risk for cerebrovascular complications (OR: 0.357), pneumoniae (OR: 0.704), and blood transfusions (OR: 0.811) (P<0.006 for all). However, morbidly obese patients were at increased risk for PE (OR: 1.267), respiratory failures (OR: 2.217), and UTIs (OR: 1.464) (P<0.011 for all). Moreover, morbidly obese patients had a significantly increased overall complication risk (OR: 1.302) when compared to non-obese patients (P<0.001).
Discussion
Morbidity and mortality are the largest concerns surrounding sd-BTKA, and conflicting studies have generated debate regarding the appropriateness of this procedure. The present study utilized the NIS database to examine and identify outcomes of sd-BTKA patients with varying BMI levels, in an effort to characterize the degree of risk higher BMI patients sustain when undergoing this procedure, as no studies have done so previously. Predictably, LOS, hospital costs and charges, and overall inpatient complication rates increased as BMI increased. Specifically, obese individuals demonstrated increased risk for PE, PJI, and respiratory failures, while morbidly obese individuals demonstrated increased risk for PE, sepsis, respiratory failures, and UTIs. Similar to unilateral TKA, the presence of obesity or morbid obesity appears to confer a higher level of overall risk for complications in patients undergoing sd-BTKA.
This study does possess limitations. As the present study was performed retrospectively, the authors were confined to the data presented within the NIS database. Second, the transition period from ICD-9 to ICD-10 medical coding systems occurred during our study. The new coding system may have caused providers to miscode sd-BTKAs, producing inconsistencies in our obtained incidence numbers. However, any data entry errors that occurred were likely diminished due to the considerable sizes of our analyzed cohorts. Moreover, querying the NIS in the method we chose did not delineate between simultaneous or sequential BTKA, which is why we opted for the term ‘same-day’. Nonetheless, both procedures are performed under the same anesthetic and may incur similar perioperative risk, as several studies have compared both approaches to staged BTKA or unilateral TKA (31-34). Third, the NIS database only captures the inpatient stay. Therefore, we were unable to measure readmissions and post-discharge complications. Although, this study provides a thorough analysis regarding the morbidity and mortality of patients with varying BMI statuses throughout the inpatient stay, which is arguably when the patient is subjected to the highest amount of risk. Although limitations exist in this study, the breadth of our analysis is comprehensive and provides valuable information pertaining to the role of BMI in the highly debated procedure of sd-BTKA.
In the present study, a significant difference was observed between BMI and hospital LOS. As BMI increased, the LOS also increased, with non-obese individuals staying an average of 3.6 days and morbidly obese individuals staying 4.0 days. An increased LOS can have large implications on the postoperative outcomes TKA patients. Otero et al. (35) examined the association between LOS and complications in TKA patients from 2011 to 2013, finding patients staying four or more days experienced complication rates that were three times higher than those staying 3 days (3.41% vs. 11.15%). Moreover, the cohort staying 4 days or longer had a higher average American Society of Anesthesiologists (ASA) scores, were older, and more likely to be female. Although LOS in itself was likely not the sole reason patients experienced higher complication rates, it appears to be an important factor that should be reduced, though this may not be readily possible when performing sd-BTKA. Thus, selecting patients with favorable characteristics, namely lower ASA or younger age, may be the next best option to optimize postoperative courses. Davidson et al. (36) did just that and assessed outcomes in sd-BTKA patients who were selected via their institutionally developed appropriateness of care criteria (AOCC) versus those who were not. Patients were considered ‘ideal’ candidates by the AOCC if they were younger than 70, did not have cardiac disease, diabetes, or lower extremity deformities, and were non-obese. With the AOCC stratification tool, the ideal cohort was younger (61 vs. 65 years), had fewer comorbidities, required a shorter LOS (3.6 vs. 3.9 days), and were discharged home more frequently (26% vs. 13%). While this study used obesity as an exclusion criterion, providers may observe good outcomes in higher BMI patients if they appropriately satisfy other criteria. Obese and morbidly obese individuals who underwent sd-BTKA in the present study appeared to be ‘healthier’ despite the presence of obesity, as evidenced by the reduced average ACCI and age. Performing sd-BTKA on high BMI individuals is possible, and risk stratifying patients in a manner similar to the AOCC may increase the likelihood of achieving favorable outcomes.
Both obese and morbidly obese cohorts demonstrated increased odds for experiencing complications, but morbidly obese patients demonstrated a statistically significant increase in overall complications. Unfortunately, only a select few have examined the role of obesity in sd-BTKA. In a retrospective study performed by Taylor et al. (37), the authors compared 1-year morbidity and mortality rates in obese patients undergoing either sd-BTKA (n=151) or unilateral TKA (n=148), concluding both major (MI, PE, cerebrovascular accident, etc.) and minor (UTI, superficial infection, ileus, etc.) complication rates in sd-BTKA to be similar to unilateral TKA. Thus, obese individuals undergoing the procedure of sd-BTKA may not be at increased risk compared to their unilateral TKA counterparts. Madsen et al. (3) investigated morbidly obese patients receiving sd-BTKA by performing a ten-year analysis of outcomes in non-obese (n=79) and morbidly obese patients (n=42). The authors found similar complication rates between the two cohorts, with both experiencing four major complication events. The obese cohort experienced one PE, one extensor mechanism disruption, and two DVTs, while the morbidly obese cohort experienced one MI, one extensor mechanism disruption, and two DVTs. Although the authors provided a long-term analysis of sd-BTKA patients, the number of patients examined in each cohort was insufficient to make appropriate conclusions regarding the procedure. Predicated off the limited literature assessing BMI status and sd-BTKA, the benefit of this procedure remains inconclusive, though it may be appropriate for higher BMI individuals with desirable comorbidity profiles. Moreover, opting to perform sd-BTKA may benefit select higher BMI patients considering staged BTKA. In a study performed by Grace et al. (38), the authors examined the risk for recurrent complications (MI and other cardiac-related complications, ischemic stroke, respiratory complications, digestive complications, urinary complications, and hematomas) in staged BTKA patients after they experienced a complication following their initial unilateral TKA. The authors noted significantly increased odds ratios (OR) for all analyzed complications, with MIs [OR: 56.63; 95% confidence interval (CI): 18.04–155.44; P<0.001] and stroke (OR: 41.38; 95% CI: 1.98–275.82; P=0.03) presenting the greatest risk. As higher BMI individuals already experience increased probabilities for complications with unilateral TKA compared to non-obese patients, providers may want to consider the prospect of sd-BTKA to mitigate the cumulative risk staged BTKA bestows upon these patients.
Conclusions
The United States continues to experience an increase in obesity, and arthroplasty surgeons will be faced with the decision of operating on these patients. The present study determined that high BMI patients undergo meticulous selection for sd-BTKA, as evidenced by decreasing age and ACCI. However, these patients are still experiencing longer LOS, heightened chances for discharge to nursing facilities, and increased complication rates compared to their non-obese counterparts. Despite these differences, obese and morbidly patients may be optimized to a level where they experience similar risk to those with comparable BMIs undergoing unilateral TKA. More research is necessary to understand the risk patients accrue when undergoing sd-BTKA compared to those undergoing staged BTKA.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/atm-20-806
Peer Review File: Available at http://dx.doi.org/10.21037/atm-20-806
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-806). JN reports other from Journal of Arthroplasty, from Journal of the American Osteopathic Medicine Association, from Orthopedic Knowledge Online, from Journal of Knee Surgery, other from Stryker, outside the submitted work. RED reports other from Baltimore City Medical Society, other from Orthofix, Inc, other from Stryker, other from United Orthopedics, other from Flexion Therapeutics, other from TissueGene, outside the submitted work. RED serves as an unpaid editorial board member of Annals of Translational Medicine from Jul 2018 to Jun 2020. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Davis MA, Ettinger WH, Neuhaus JM, et al. The association of knee injury and obesity with unilateral and bilateral osteoarthritis of the knee. Am J Epidemiol 1989;130:278-88. [Crossref] [PubMed]
- Parvizi J, Rasouli MR. Simultaneous-bilateral TKA: double trouble - affirms. J Bone Joint Surg Br 2012;94:90-2. [Crossref] [PubMed]
- Madsen AA, Taylor BC, Dimitris C, et al. Safety of Bilateral Total Knee Arthroplasty in Morbidly Obese Patients. Orthopedics 2014;37:e252-9. [Crossref] [PubMed]
- Memtsoudis SG, Hargett M, Russell LA, et al. Consensus statement from the consensus conference on bilateral total knee arthroplasty group knee. Clin Orthop Relat Res 2013;471:2649-57. [Crossref] [PubMed]
- Odum SM, Troyer JL, Kelly MP, et al. A cost-utility analysis comparing the cost-effectiveness of simultaneous and staged bilateral total knee arthroplasty. J Bone Joint Surg Am 2013;95:1441-9. [Crossref] [PubMed]
- March LM, Cross M, Tribe KL, et al. Two knees or not two knees? Patient costs and outcomes following bilateral and unilateral total knee joint replacement surgery for OA. Osteoarthr Cartil 2004;12:400-8. [Crossref] [PubMed]
- Fick D, Crane T, Shakespeare D. A comparison of bilateral vs. unilateral total knee arthroplasty mobilised using a flexion regime. Knee 2002;9:285-9. [Crossref] [PubMed]
- Powell RS, Pulido P, Tuason MS, et al. Bilateral vs Unilateral Total Knee Arthroplasty: A Patient-Based Comparison of Pain Levels and Recovery of Ambulatory Skills. J Arthroplasty 2006;21:642-9. [Crossref] [PubMed]
- Fu D, Li G, Chen K, et al. Comparison of clinical outcome between simultaneous-bilateral and staged-bilateral total knee arthroplasty: A systematic review of retrospective studies. J Arthroplasty 2013;28:1141-7. [Crossref] [PubMed]
- Lindberg-Larsen M, Pitter FT, Husted H, et al. Simultaneous vs staged bilateral total knee arthroplasty: a propensity-matched case–control study from nine fast-track centres. Arch Orthop Trauma Surg 2019;139:709-16. [Crossref] [PubMed]
- Hart A, Antoniou J, Brin YS, et al. Simultaneous Bilateral Versus Unilateral Total Knee Arthroplasty: A Comparison of 30-Day Readmission Rates and Major Complications. J Arthroplasty 2016;31:31-5. [Crossref] [PubMed]
- Hu J, Liu Y, Lv Z, et al. Mortality and morbidity associated with simultaneous bilateral or staged bilateral total knee arthroplasty: A meta-analysis. Arch Orthop Trauma Surg 2011;131:1291-8. [Crossref] [PubMed]
- Stefánsdóttir A, Lidgren L, Robertsson O. Higher early mortality with simultaneous rather than staged bilateral TKAs: Results from the Swedish knee arthroplasty register. Clin Orthop Relat Res 2008;466:3066-70. [Crossref] [PubMed]
- Memtsoudis SG, González Della Valle A, Besculides MC, et al. In-hospital complications and mortality of unilateral, bilateral, and revision TKA: Based on an estimate of 4,159,661 discharges. Clin Orthop Relat Res 2008;466:2617-27. [Crossref] [PubMed]
- Poultsides L, Memtsoudis S, Gonzalez Della Valle A, et al. Perioperative morbidity and mortality of same-day bilateral TKAs: Incidence and risk factors knee. Clin Orthop Relat Res 2014;472:111-20. [Crossref] [PubMed]
- Meehan JP, Blumenfeld TJ, White RH, et al. Risks and benefits of simultaneous bilateral total knee arthroplasty. JBJS Rev 2015;3:01874474-201503020-00002.
- Fournier MN, Hallock J, Mihalko WM. Preoperative Optimization of Total Joint Arthroplasty Surgical Risk: Obesity. J Arthroplasty 2016;31:1620-4. [Crossref] [PubMed]
- Yeung E, Jackson M, Sexton S, et al. The effect of obesity on the outcome of hip and knee arthroplasty. Int Orthop 2011;35:929-34. [Crossref] [PubMed]
- Vasarhelyi EM, MacDonald SJ. The influence of obesity on total joint arthroplasty. J Bone Joint Surg Br 2012;94:100-2. [Crossref] [PubMed]
- Namba RS, Paxton L, Fithian DC, et al. Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J Arthroplasty 2005;20:46-50. [Crossref] [PubMed]
- Gandhi R, Wasserstein D, Razak F, et al. BMI independently predicts younger age at hip and knee replacement. Obesity (Silver Spring) 2010;18:2362-6. [Crossref] [PubMed]
- Wagner ER, Kamath AF, Fruth K, et al. Effect of Body Mass Index on Reoperation and Complications After Total Knee Arthroplasty. J Bone Joint Surg Am 2016;98:2052-60. [Crossref] [PubMed]
- George J, Piuzzi NS, Ng M, et al. Association Between Body Mass Index and Thirty-Day Complications After Total Knee Arthroplasty. J Arthroplasty 2018;33:865-71. [Crossref] [PubMed]
- Bordini B, Stea S, Cremonini S, et al. Relationship between obesity and early failure of total knee prostheses. BMC Musculoskelet Disord 2009;10:29. [Crossref] [PubMed]
- Hamoui N, Kantor S, Vince K, et al. Long-term outcome of total knee replacement: does obesity matter? Obes Surg 2006;16:35-8. [Crossref] [PubMed]
- Suleiman LI, Ortega G, Ong’Uti SK, et al. Does BMI affect perioperative complications following total knee and hip arthroplasty? J Surg Res 2012;174:7-11. [Crossref] [PubMed]
- Dewan A, Bertolusso R, Karastinos A, et al. Implant durability and knee function after total knee arthroplasty in the morbidly obese patient. J Arthroplasty 2009;24:89-94, 94.e1-3.
- Daniilidis K, Yao D, Gosheger G, et al. Does BMI influence clinical outcomes after total knee arthroplasty? Technol Health Care 2016;24:367-75. [Crossref] [PubMed]
- Overview of the National (Nationwide) Inpatient Sample (NIS). 2019. Available online: https://www.hcup-us.ahrq.gov/nisoverview.jsp
- Charlson M, Szatrowski TP, Peterson J, et al. Validation of a combined comorbidity index. J Clin Epidemiol 1994;47:1245-51. [Crossref] [PubMed]
- Kim YH, Choi YW, Kim JS. Simultaneous bilateral sequential total knee replacement is as safe as unilateral total knee replacement. J Bone Joint Surg Br 2009;91:64-8. [Crossref] [PubMed]
- Bini SA, Khatod M, Inacio MCS, et al. Same-Day Versus Staged Bilateral Total Knee Arthroplasty Poses No Increase in Complications in 6672 Primary Procedures. J Arthroplasty 2014;29:694-7. [Crossref] [PubMed]
- Zeni JA, Snyder-Mackler L. Clinical outcomes after simultaneous bilateral total knee arthroplasty. Comparison to unilateral total knee arthroplasty and healthy controls. J Arthroplasty 2010;25:541-6. [Crossref] [PubMed]
- Bohm ER, Molodianovitsh K, Dragan A, et al. Outcomes of unilateral and bilateral total knee arthroplasty in 238,373 patients. Acta Orthop 2016;87 Suppl 1:24-30. [Crossref] [PubMed]
- Otero JE, Gholson JJ, Pugely AJ, et al. Length of Hospitalization After Joint Arthroplasty: Does Early Discharge Affect Complications and Readmission Rates? J Arthroplasty 2016;31:2714-25. [Crossref] [PubMed]
- Davidson IU, Brigati DP, Faour M, et al. Same-Day Bilateral Total Knee Arthroplasty Candidacy Criteria Decrease Length of Stay and Facility Discharge. Orthopedics 2018;41:293-8. [Crossref] [PubMed]
- Taylor BC, Dimitris C, Mowbray JG, et al. Perioperative safety of two-team simultaneous bilateral total knee arthroplasty in the obese patient. J Orthop Surg Res 2010;5:38. [Crossref] [PubMed]
- Grace TR, Tsay EL, Roberts HJ, et al. Staged Bilateral Total Knee Arthroplasty: Increased Risk of Recurring Complications. J Bone Joint Surg Am 2020;102:292-7. [Crossref] [PubMed]


