
Impact of cerebral ischemic lesions on the outcome of carotid endarterectomy
Introduction
Patients with hemodynamically significant carotid artery stenosis (CAS) are commonly stratified according to the presence of previous neurological events. However, a dichotomy between symptomatic and asymptomatic patients is not accurate enough to precisely identify the risk of new symptoms or recurrences or to define the perioperative risk in patients submitted to carotid revascularization. As a matter of fact, the stratification of symptomatic patients according to the type of symptoms is important to identify those at higher risk of stroke and also to evaluate the risk of a revascularization procedure (1), since it is well known that patients with stroke in evolution or transient ischemic attack (TIA) in crescendo are more prone to perioperative complications compared with patients with a single stable TIA (2-4). Other than the clinical status, the presence and extension of cerebral ischemic lesions (CIL) is increasingly used as a stratification tool of these patients (5). Specifically, CIL are constantly considered in the evaluation of patients with CAS, since their presence can identify patients with “silent symptoms” who are at higher risk for further cerebral ischemic events, even if they are apparently asymptomatic (6). Moreover, CIL can be an adjunctive element to assess the perioperative risk of patients scheduled for carotid revascularization, being in some instances an important factor in defining the appropriate intervention time (7).
In the European Society of Vascular and Endovascular Surgery guidelines (1), the presence of CIL in an asymptomatic CAS patient is considered an element of increased stroke risk, suggesting carotid revascularization. In symptomatic patients, with a severe stroke and a CIL extension of more than 1/3 of the medium cerebral artery territory, the intervention should be delayed (1).
The present review focus on the influence of CIL on patients with CAS, analysing their impact in both asymptomatic and symptomatic patients.
Silent CILs in patients with asymptomatic carotid stenosis and risk of new events
The presence of CIL in asymptomatic patients is commonly defined as “silent” CIL. The identification of such lesions, ipsilateral to CAS, can be considered the effect of a previous embolic event from the carotid plaque; the apparent absence of symptoms can be due to either the involvement of a mute brain area or to a an unrecognized event, i.e., occurring during sleep or of a minimal clinical magnitude. A silent CIL can be identified in about 10–20% of patients with CAS (8,9).
The stroke risk of patients with asymptomatic CAS is commonly considered 1% for every year, but patients with CIL have a significantly higher annual risk of cerebral events (4.5–5%) (8,10). Specifically, in the ACSRS (11) analysis, patients with CAS had 2.4% of TIA/stroke risk per year, that increased to 4.6% in patients with asymptomatic CIL; moreover, the stroke rate increased from 1% to 3.6%. Similar results were reported in the ACST (12): patients with silent CIL had an absolute stroke risk increase of 5.8% at 10-year follow-up, as confirmed by the multivariate analysis, with a hazard ratio 1.5. In the Rotterdam study, including 1,077 patients, the presence of asymptomatic CIL at magnetic resonance imaging (MRI), was found to be an independent risk factor for stroke, with a 3-fold increase during a 4-year follow-up (13).
Jayasooriya et al. (14) confirmed those data, with non-lacunar CIL identified as a specific risk factor for future stroke in patients with CAS, with an odd ratio of 4.6. CIL in asymptomatic CAS are associated with ipoechogenicity of the carotid plaque at the grey scale measurement, plaque ulceration and very severe stenosis (15,16). However, independently from the intima media thickness, the presence of a CIL is an independent risk factor for future stroke (17).
There are different hypotheses to justify such an increased risk. The CIL can damage the cerebrovascular reactivity, reducing the cerebrovascular reserve of the brain, consequently leading to a greater sensibility of the cerebral parenchyma to the ischemic events; also the CIL can be a manifestation of an embolizing CAS, as demonstrated by the association between CIL and microembolic signals at TCD (18-20). The identification of asymptomatic microembolic signals at the transcranial Doppler was identified as an adjunctive factor supporting the indication to CEA in asymptomatic patients (Class IIa level B, evidence) (1,21-24).
Silent CIL and carotid revascularization outcome
According with the concepts detailed above, asymptomatic patients with silent CIL are comparable to symptomatic patients. Based on that assumption, some authors evaluated the risk of carotid revascularization in these instances, in order to ascertain if the results were similar to those of symptomatic patients. Although Cao et al. (25) concluded that silent CIL do not influence CEA results significantly, the study of Fürst et al. (26), by analysing the results of 297 asymptomatic CEAs, showed that silent CIL increased the postoperative stroke risk up to 7%; the authors concluded that SCI can affect the cerebral vascular reserve, with an alteration of the collateral pathway determining a higher sensitivity to ischemic lesion. In the paper of Pini et al. (6), patients with silent CIL had a significantly higher 30-day post-CEA stroke of 3.1% vs. 0.2% of patients without CIL (Table 1). The slight increase of the risk of CEA complications in asymptomatic patients with CIL led to question the real benefit obtainable in this particular group of patients. Data from ACST (12) confirm the efficacy of CEA in the reduction of stroke in patients submitted to carotid endarterectomy with silent CIL. At 5-year of follow-up, the stroke rate in patients in the delayed CEA group was 10%, compared with 7% in patients submitted to early CEA, with a relative risk reduction of 30% (absolute 3%) in the latter group. The benefit was more pronounced at 10 years of follow-up, with 12.8% stroke rate in the early CEA group, compared with 18.6% in the deferred group, with a relative stroke risk reduction of 50% (absolute 6%).

Full table
The ACST (12) data underline the necessity to consider asymptomatic patients with silent CIL a separate entity, different from both asymptomatic and symptomatic patients, with a high risk of cerebral events the carotid lesion is left untreated, and a high benefit from the intervention.
CIL in symptomatic CAS
Carotid revascularization outcome according to the presence of CIL
Symptomatic carotid artery stenoses need prompt revascularization to reduce the recurrence of cerebral ischemic events; the highest benefit is reached if the intervention is performed within two weeks from the index event (1). In the panorama of the symptomatic status, the presence and characteristics of CIL can be considered important elements to better stratify these patients.
However, different data are reported in the literature. Cao et al. (27), in their analysis of 503 symptomatic patients, identified CIL in 54% of patients with stroke and 33% of those with TIA. CIL influenced the outcome of CEA in their series: stroke and death were significantly higher in patients with CIL (OR: 6.37; 95% CI, 5.12–7.63). Similarly, Blohmé et al. (28), in a retrospective analysis of 273 symptomatic patients, showed that the presence of an ipsilateral CIL was associated with a higher risk of stroke/death, compared with patients without CIL (10% vs. 3%; P=0.01).
Differently, data from 1,604 symptomatic patients submitted to CEA in the ECST (29) showed a stroke/death rate after CEA similar in patients with and without CIL (7.5% vs. 6.7%; P=0.45).
Influence of CIL volume on the carotid revascularization outcome
A possible explanation of the different outcome associated with CIL in the literature data can be due to the effect of the CIL volume, that has been scarcely evaluated in many reports (30). In a paper from Pini et al. (5), the presence of a CIL was not identified as a possible risk factor for carotid revascularization in 489 symptomatic patients: 4.8% vs. 3.5%, P=0.46. However, the CIL volume of patients who suffered a post-operative stroke was significantly higher compared with that of patients with favourable outcome: 5,100 mm3 (IQR, 31,000 mm3) vs. 1,000 mm3 (IQR, 7,000 mm3) P=0.01. In the evaluation of CIL volumes, the authors identified in 4,000 mm3 a threshold for a higher risk of stroke/death after carotid revascularization. A CIL volume >4,000 mm3 was identified as an independent risk factor for postoperative stroke, which was as high as 9.3%, compared with 1.9% of patients with a CIL volume <4,000 mm3.
Patients with large volume CIL should have a carotid revascularization delayed for more than 2 weeks, according to the guidelines of ESVES (1), without a more specific definition of the timing for the intervention. For those patients, some authors suggest awaiting at least 4-week from symptoms, reporting better results in the late revascularization group (11.9% vs. 1.7%, P=0.03) (31).
Asymptomatic CIL after carotid endarterectomy
Other than evaluating the effect of preoperative CIL on CEA outcome, many authors focused their researches on the identification of new asymptomatic CIL after carotid revascularization, as a surrogate marker of possible cerebral events after carotid revascularization. The common method adopted to identify new asymptomatic CIL is the diffusion weight magnetic resonance, which can identify new asymptomatic CIL after carotid revascularization. Different studies have evaluated the presence of new CIL after CEA, founding that their presence is relatively uncommon ranging from 4% to 9%. Different anatomical and technical characteristics were identified as possible risk factors for new asymptomatic CIL at DWI-MR, such as the presence of concomitant ipsilateral vertebral artery stenosis or the intraoperative use of shunt (32,33).
Conclusions
Patients with CAS are commonly divided in symptomatic and asymptomatic, however it is necessary to better stratify these patients, as shown by a growing evidence in the literature. Asymptomatic CAS patients can be divided in those without CIL, who are at low risk for future neurologic events, and in those with CIL, who are at higher risk for future strokes. Moreover, symptomatic patients can be stratified in patients without CIL (more often with TIA and amaurosis fugax) or small (<4,000 mm3) CIL; in both cases the carotid revascularization can be performed in the early period after symptoms, with a low rate of post-operative events. Differently, patients with a CIL volume >4,000 mm3 are associated with a poorer outcome, therefore some experiences suggest delaying the carotid revascularization of at least 4 weeks, in order to reduce the postoperative complication rate (34) (Table 2).
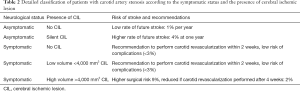
Full table
In summary, CIL are a key factor to ascertain indication to, and benefit of, carotid revascularization.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Dr. Kosmas I. Paraskevas) for the series “Carotid Artery Stenosis and Stroke: Prevention and Treatment Part I” published in Annals of Translational Medicine. The article was sent for external peer review organized by the Guest Editor and the editorial office.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/atm-20-1098). The series “Carotid Artery Stenosis and Stroke: Prevention and Treatment Part I” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Naylor AR, Ricco JB, de Borst GJ, et al. Editor's Choice - Management of Atherosclerotic Carotid and Vertebral Artery Disease: 2017 Clinical Practice Guidelines of the European Society for Vascular Surgery (ESVS). Eur J Vasc Endovasc Surg 2018;55:3-81. [Crossref] [PubMed]
- Pini R, Faggioli G, Gargiulo M, et al. The different scenarios of urgent carotid revascularization for crescendo and single transient ischemic attack. Vascular 2019;27:51-9. [Crossref] [PubMed]
- Pini R, Faggioli G, Longhi M, et al. Impact of postoperative transient ischemic attack on survival after carotid revascularization. J Vasc Surg 2014;59:1570-6. [Crossref] [PubMed]
- Nordanstig A, Rosengren L, Strömberg S, et al. Editor's Choice - Very Urgent Carotid Endarterectomy is Associated with an Increased Procedural Risk: The Carotid Alarm Study. Eur J Vasc Endovasc Surg 2017;54:278-86. [Crossref] [PubMed]
- Pini R, Faggioli G, Longhi M, et al. Impact of acute cerebral ischemic lesions and their volume on the revascularization outcome of symptomatic carotid stenosis. J Vasc Surg 2017;65:390-7. [Crossref] [PubMed]
- Pini R, Faggioli G, Longhi M, et al. The detrimental impact of silent cerebral infarcts on asymptomatic carotid endarterectomy outcome. J Vasc Surg 2016;64:15-24. [Crossref] [PubMed]
- Jean-Baptiste E, Perini P, Suissa L, et al. Prognostic value of preoperative border-zone (watershed) infarcts on the early postoperative outcomes of carotid endarterectomy after acute ischemic stroke. Eur J Vasc Endovasc Surg 2013;45:210-7. [Crossref] [PubMed]
- Naylor AR, Schroeder TV, Sillesen H. Clinical and imaging features associated with an increased risk of late stroke in patients with asymptomatic carotid disease. Eur J Vasc Endovasc Surg 2014;48:633-40. [Crossref] [PubMed]
- Bernick C, Kuller L, Dulberg C, et al. Cardiovascular Health Study Collaborative Research Group. Silent MRI infarcts and the risk of future stroke: the cardiovascular health study. Neurology 2001;57:1222-9. [Crossref] [PubMed]
- Pini R, Faggioli G, Vacirca A, et al. The fate of asymptomatic severe carotid stenosis in the era of best medical therapy. Brain Inj 2017;31:1711-7. [Crossref] [PubMed]
- Kakkos SK, Sabetai M, Tegos T, et al. Asymptomatic Carotid Stenosis and Risk of Stroke (ACSRS) Study Group. Silent embolic infarcts on computed tomography brain scans and risk of ipsilateral hemispheric events in patients with asymptomatic internal carotid artery stenosis. J Vasc Surg 2009;49:902-9. [Crossref] [PubMed]
- Streifler JY, den Hartog AG, Pan S, et al. ACST-1 trial collaborators. Ten-year risk of stroke in patients with previous cerebral infarction and the impact of carotid surgery in the Asymptomatic Carotid Surgery Trial. Int J Stroke 2016;11:1020-7. [Crossref] [PubMed]
- Vermeer SE, Hollander M, van Dijk EJ, et al. Silent brain infarcts and white matter lesions increase stroke risk in the general population: the Rotterdam Scan Study. Stroke 2003;34:1126-9. [Crossref] [PubMed]
- Jayasooriya G, Thapar A, Shalhoub J, et al. Silent cerebral events in asymptomatic carotid stenosis. J Vasc Surg 2011;54:227-36. [Crossref] [PubMed]
- Sabetai MM, Tegos TJ, Clifford C, et al. Carotid plaque echogenicity and types of silent CT-brain infarcts. Is there an association in patients with asymptomatic carotid stenosis? Int Angiol 2001;20:51-7. [PubMed]
- Hougaku H, Matsumoto M, Handa N, et al. Asymptomatic carotid lesions and silent cerebral infarction. Stroke 1994;25:566-70. [Crossref] [PubMed]
- Miwa K, Hoshi T, Hougaku H, et al. Silent cerebral infarction is associated with incident stroke and TIA independent of carotid intima-media thickness. Intern Med 2010;49:817-22. [Crossref] [PubMed]
- Orlický M, Vachata P, Barto R, et al. A selective carotid artery shunting for carotid endarterectomy: prospective MR DWI monitoring of embolization in a group of 754 patients. J Neurol Surg A Cent Eur Neurosurg 2015;76:89-92. [PubMed]
- Purkayastha S, Fadar O, Mehregan A, et al. Impaired cerebrovascular hemodynamics are associated with cerebral white matter damage. J Cereb Blood Flow Metab 2014;34:228-34. [Crossref] [PubMed]
- Paraskevas KI, Spence JD, Veith FJ, et al. Identifying which patients with asymptomatic carotid stenosis could benefit from intervention. Stroke 2014;45:3720-4. [Crossref] [PubMed]
- Spence JD, Coates V, Li H, et al. Effects of intensive medical therapy on microemboli and cardiovascular risk in asymptomatic carotid stenosis. Arch Neurol 2010;67:180-6. [Crossref] [PubMed]
- Spence JD, Tamayo A, Lownie SP, et al. Absence of microemboli on transcranial Doppler identifies low-risk patients with asymptomatic carotid stenosis. Stroke 2005;36:2373-8. [Crossref] [PubMed]
- Spence JD. Transcranial Doppler monitoring for microemboli: a marker of a high-risk carotid plaque. Semin Vasc Surg 2017;30:62-6. [Crossref] [PubMed]
- Topakian R, King A, Kwon SU, et al. Ultrasonic plaque echolucency and emboli signals predict stroke in asymptomatic carotid stenosis. Neurology 2011;77:751-8. [Crossref] [PubMed]
- Cao P, Zannetti S, Giordano G, et al. Cerebral tomographic findings in patients undergoing carotid endarterectomy for asymptomatic carotid stenosis: short-term and long-term implications. J Vasc Surg 1999;29:995-1005. [Crossref] [PubMed]
- Fürst H, Hartl WH, Haberl R, et al. Silent cerebral infarction: risk factor for stroke complicating carotid endarterectomy. World J Surg 2001;25:969-74. [Crossref] [PubMed]
- Cao P, Giordano G, De Rango P, et al. Computerised tomography findings as a risk factor in carotid endarterectomy: early and late results. Eur J Vasc Endovasc Surg 1996;12:37-45. [Crossref] [PubMed]
- Blohmé L, Sandström V, Hellström G, et al. Complications in carotid endarterectomy are predicted by qualifying symptoms and preoperative CT findings. Eur J Vasc Endovasc Surg 1999;17:213-8. [Crossref] [PubMed]
- Bond R, Narayan SK, Rothwell PM, et al. European Carotid Surgery Trialists' Collaborative Group. Clinical and radiographic risk factors for operative stroke and death in the European carotid surgery trial. Eur J Vasc Endovasc Surg 2002;23:108-16. [Crossref] [PubMed]
- Faggioli G, Pini R, Mauro R, et al. Perioperative outcome of carotid endarterectomy according to type and timing of neurologic symptoms and computed tomography findings. Ann Vasc Surg 2013;27:874-82. [Crossref] [PubMed]
- Pini R, Faggioli G, Vacirca A, et al. Is size of infarct or clinical picture that should delay urgent carotid endarterectomy? A meta-analysis. J Cardiovasc Surg (Torino) 2020. [Epub ahead of print]. [Crossref] [PubMed]
- Pascot R, Parat B, Le Teurnier Y, et al. Predictive Factors of Silent Brain Infarcts after Asymptomatic Carotid Endarterectomy. Ann Vasc Surg 2018;51:225-33. [Crossref] [PubMed]
- Roh HG, Byun HS, Ryoo JW, et al. Prospective analysis of cerebral infarction after carotid endarterectomy and carotid artery stent placement by using diffusion-weighted imaging. AJNR Am J Neuroradiol 2005;26:376-84. [PubMed]
- Pini R, Faggioli G, Vacirca A, et al. The benefit of deferred carotid revascularization in patients with moderate-severe disabling cerebral ischemic stroke. J Vasc Surg 2020. [Epub ahead of print]. [Crossref] [PubMed]


