Low awareness of stroke guidelines and preference for Chinese herbs in community physicians: a national survey in China
Introduction
Stroke patients are at high risk of recurrent stroke. It is important to comprehensively evaluate stroke etiology and give evidence-based secondary prevention therapies. To improve the quality of managements, the guidelines of stroke secondary prevention have been published and updated in many countries (1-5). Applying these guidelines in clinical practice significantly reduce the recurrence of stroke (6,7). The physicians’ adherence to the guidelines, therefore, is becoming a critical part of public stroke care system.
With 2.5 million new stroke cases each year, stroke has been the leading cause of mortality and disability in China (3). The recurrence of stroke in Chinese patients is 16-20% at 1 year after initial event, higher than the average rate of 11.1% worldwide (8,9). Given the diverse social economic status among different regions, China is facing great challenges to establish a cost-effective public stroke care system. In 2010, Chinese guidelines for the secondary prevention of ischemic stroke and transient ischemic attack was opened to the public (3). In this study, we performed a national survey to evaluate the awareness of current stroke guidelines in Chinese physicians.
Methods
Survey development and participants
This is an investigator-initiated, non-commercial, and no-incentive survey of the physicians who visit the sole Chinese government-authorized website (www.haoyisheng.com, HYS) for continuing medical education (CME). In China, CME is a mandatory requirement for each registered physician. To obtain the official admitted CME scores from HYS, the physicians need to register by providing their identities and working settings. When a visitor logged in HYS, a window with our survey popped out automatically. If the visitors declined the survey, they could continue their visits by closing the window. This study was performed from Oct 2010 to Jan 2012, and was approved by Peking Union Medical College Hospital ethic group.
Survey content
Survey respondents were asked to perform a self-examination of 13 questions regarding their current practice in stroke (Supplement). Physicians may select their preferred treatment strategies or prescriptions on cardiogenic stroke and large artery atherosclerotic stroke before checking the “standard answers”. The specialty and title of physicians, level of hospital, and expenses of stroke patient were also surveyed.
Data collection and procession
All data were automatically saved on line and could be transferred into an electronic Excel database (Microsoft Corp.) if required. The private information including name and identity number was kept secret by HYS, while the working hospitals, gender, age and log-in time were open to the investigators. Statistics analysis was performed using SAS Version 9.0.
Analysis
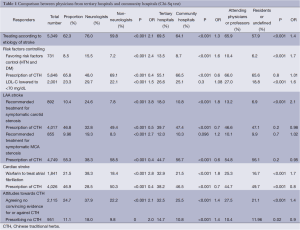
Our primary outcome measures were: (I) the percentage of physicians who selected the treatment strategies or prescriptions recommended by stroke guidelines; (II) the percentage of physicians who prescribed Chinese traditional herbs (CTH); (III) the stroke patients’ expense reported by physicians. We compared the provided answers from neurologists and non-neurologists; physicians from tertiary and community (primary and secondary) hospitals; experienced physicians (attending physicians and professors) and un-experienced physicians (residents and unrated physicians) using univariate analysis (Table 1) and logistic regression.
Full table
Results
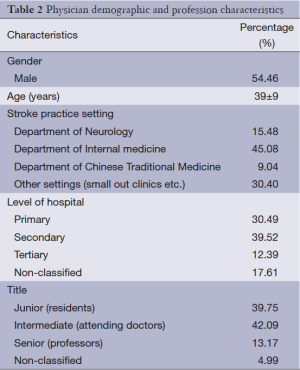
A total of 8,581 physicians from all 32 provinces and regions in China responded to the survey. Physicians demographic and profession characteristics are summarized in Table 2. In the responders, 70.1% were from community hospitals (39.52% from secondary and 30.49% from primary hospitals) and 12.39% from tertiary hospitals. Most respondents (81.84%) were junior (resident) or intermediate (attending doctor). Neurologists account for 15.48% of the respondents, while more respondents (45.08%) had their stroke practice in internal medicine department.
Full table
Concepts on stroke etiologies and risk factors control
A high percentage (62.34%, n=5,349) of doctors agreed to establish their treatment strategy based on the etiologies of stroke (stroke subtypes) whereas 24.39% (n=2,093) based on the severity of stroke, and 6.14% (n=527) based on the principle of “combining Chinese traditional medicine and Western medicine”. Doctors from community hospitals, non-neurologists and un-experienced physicians (junior) less likely concerned about the etiology of stroke (Figure 1A).
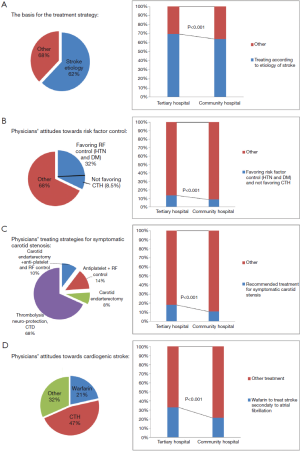
For a patient with a history of TIA or stroke, only 32.1% physicians believed well risk factor modification could reduce the risk of recurrent stroke. Of these physicians, 73.46% also agreed CTH for secondary prevention, which was not recommended by the guidelines. Physicians from community hospitals and non-neurologists were less likely to manage the risk factors, and more likely to give additional CTH treatment (Figure 1B).
Concepts of large artery atherosclerotic stroke managements
Regarding to the treatments of symptomatic carotid stenosis, only 10.4% physicians selected carotid endarterectomy and anti-platelet plus controlling stroke risk factors, which are recommended by the guidelines (1,3). For the treatments of symptomatic middle cerebral artery stenosis, only 9.96% physicians selected aspirin or clopidogrel (1), and 23.32% physicians selected the target of <70 mg/dL and lifelong statin use (1). In contrast, as high as 55.34% physicians preferred to prescribe CTH in their practice. Physicians from community hospital, non-neurologists, and un-experienced physicians were less likely to adhere to the guidelines. Physicians from community hospital and non-neurologists were more likely to prescribe CTH (Figure 1C).
Concepts of cardiogenic stroke managements
For a stroke patient with atrial fibrillation, only 21.45% physicians selected warfarin anticoagulation treatment, which is recommended by the guidelines (1). The remaining selected anti-platelet, CTH, cardiac surgery, or combination of them. A high percentage of physicians (46.92%) prescribed CTH in their practice. Physicians from community hospital, non-neurologists, and un-experienced physicians were less likely to follow the guidelines, and more prone to prescribe CTH (Figure 1D).
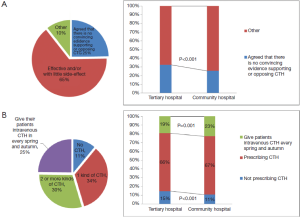
Physicians reports on CTH and patients expense
A high percentage (64.56%) of physicians had positive attitude towards CTH (effective and/or with little side-effect): 34.39% physicians prescribed one kind of CTH for their patients; 29.77% physicians prescribed two or more kinds of CTH; and 24.75% physicians preferred to give their patients intravenous CTH in every spring and autumn. Only 11.08% physicians did not prescribe CTH at all, and 24.65% physicians agreed that there is no convincing evidence supporting or opposing CTH. Physicians from community hospitals (P<0.001, OR =0.71), non-neurologists (P<0.001, OR =0.47), and un-experienced physicians (P<0.001, OR =0.70) were less likely aware of that CTH had no convincing evidence (Figure 2).
A total of 63.1% physicians reported their patients’ expenses for secondary stroke prevention were more than 200 RMB (about $34) per month. Those who prescribe one kind or more CTH for their patients reported more expenses (P<0.001, OR =1.78, 95% CI, 1.55-2.04).
Discussion
Several studies showed there was a gap between the guidelines and clinical practice. In the Reduction of Atherothrombosis for Continued Health (REACH) registry, a large investigation obtaining the data from 44 countries, 18% of the patients with a stroke history did not receive any antiplatelet therapy; and 43% did not receive any statin (10-12). Another survey of 3,489 Chinese neurologists from tertiary hospitals (with relatively high quality medical service in China) showed insufficient awareness of secondary stroke prevention guidelines. Less than 40% of Chinese neurologists are aware of the BP control goal in non-diabetic patients after an episode of ischemic stroke or TIA (13). In this survey, a wide gap was also seen between the responders’ concepts and stroke guidelines. Over all, less than one third responders considered risk factors control necessary for stroke, and less than 20% physicians gave treatments according to the guidelines. Most of the responders were community physicians and they were more likely unaware of the guidelines compared with those from tertiary hospitals. Therefore, the results suggest the stroke care in Chinese community hospitals is especially far away from the guidelines.
In this study, the physicians’ concepts of CTH were also surveyed. According to the theories of Chinese traditional medicine, “stasis of blood” is believed to be the main cause of ischemic stroke. The extracts of herbs such as Chuan Qiong, Erigeron Breviscapus, Radix Notoginseng, Radix Salviae Miltiorrhizae, Carthamus tinctorious, and Ginkgo, are believed to have an effect on “dissipating blood stasis”. In this survey, more than half of Chinese physicians had positive attitude towards CTH and preferred to prescribe CTH. The results suggested the concept of Chinese traditional medicine are more widely accepted and used in stroke patients than the guidelines. Given there is no convincing evidence of CTH in stroke (14), the prescriptions of CTH may highly increase the cost of stroke treatment with unknown effects. While more clinical trials with good quality are required to establish the efficacy and safety of CTH, the completed clinical trials of CTH should be systematically reviewed and a special guideline for CTH may be warranted.
Our study has several strengths. Current survey was the first survey of physicians from different level of hospitals with a large sample. It was designed according to local culture. Compared with the style of official non-interactive survey, the “self-examination” style with a small number of questions is more likely accepted by Chinese physicians. The non-commercial, no-incentive characteristics of the survey make the data more reliable. However, this study suffered from several limitations. The physicians who declined participating in the survey (closing the survey window) couldn’t be recorded technically in this study. The response rate was not calculated and reported. Potential bias, therefore, may exist. For example, only the physicians who are interested in stroke or who are enthusiastic about self-learning responded to this survey. Second, this survey was performed via internet media. Physicians without convenient internet access in some rural area of China may have no chances to respond to the survey.
Our results are meaningful for optimizing the public stroke care system. China is a representative of a developing country with a rapid economy growth. The health care system is undergoing huge changes. Currently, Chinese patients with “mild diseases” are encouraged to see the community physicians by the official authorities. A proportion of patients with minor stroke and transient ischemic attacks probably go to the community hospitals after the onset. In these patients, effective secondary stroke prevention managements must be given timely because a high rate of stroke recurrence happens (8). However, as reported in this study, the low awareness of guidelines in community physicians makes the stroke care system unlikely work in a cost-effective way. Therefore, it is important to establish a well-organized CME system for stroke guidelines training, which should be an essential complementary policy.
Conclusions
In conclusion, we found there is a wide gap between the secondary stroke prevention guidelines and Chinese community physicians practice. Our results suggest that a well-organized CME system for stroke should be established as an essential part in this largest developing country.
Acknowledgements
We are grateful to Xiaonan Huang, a member of working staff in HYS website who helped us to complete this survey.
Disclosure: The authors declare no conflict of interest.
References
- Furie KL, Kasner SE, Adams RJ, et al. Guidelines for the prevention of stroke in patients with stroke or transient ischemic attack: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke 2011;42:227-76. [PubMed]
- Lansberg MG, O’Donnell MJ, Khatri P, et al. Antithrombotic and thrombolytic therapy for ischemic stroke: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141:e601S-36S.
- Wang YJ, Zhang SM, Zhang L, et al. Chinese guidelines for the secondary prevention of ischemic stroke and transient ischemic attack 2010. CNS Neurosci Ther 2012;18:93-101. [PubMed]
- Bryer A, Connor MD, Haug P, et al. The South African guideline for the management of ischemic stroke and transient ischemic attack: recommendations for a resource-constrained health care setting. Int J Stroke 2011;6:349-54. [PubMed]
- Venketasubramanian N, Pwee KH, Chen CP. Singapore Ministry of health clinical practice guidelines on stroke and transient ischemic attacks. Int J Stroke 2011;6:251-8. [PubMed]
- Rothwell PM, Coull AJ, Giles MF, et al. Change in stroke incidence, mortality, case-fatality, severity, and risk factors in Oxfordshire, UK from 1981 to 2004 (Oxford Vascular Study). Lancet 2004;363:1925-33. [PubMed]
- Hong KS, Yegiaian S, Lee M, et al. Declining stroke and vascular event recurrence rates in secondary prevention trials over the past 50 years and consequences for current trial design. Circulation 2011;123:2111-9. [PubMed]
- Mohan KM, Wolfe CD, Rudd AG, et al. Risk and cumulative risk of stroke recurrence: a systematic review and meta-analysis. Stroke 2011;42:1489-94. [PubMed]
- Wang Z, Li J, Wang C, et al. Gender differences in 1-year clinical characteristics and outcomes after stroke: results from the China National Stroke Registry. PLoS One 2013;8:e56459. [PubMed]
- Bhatt DL, Steg PG, Ohman EM, et al. International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA 2006;295:180-9. [PubMed]
- Toso V, Carolei A, Gensini GF, et al. The Stroke in Italy and Related Impact on Outcome (SIRIO) study: design and baseline data. Neurol Sci 2006;27 Suppl 3:S263-7. [PubMed]
- Leoo T, Lindgren A, Petersson J, et al. Risk factors and treatment at recurrent stroke onset: results from the Recurrent Stroke Quality and Epidemiology (RESQUE) Study. Cerebrovasc Dis 2008;25:254-60. [PubMed]
- Wu J, Jia LF, Jia JP. Awareness of secondary stroke prevention guidelines among neurologists in China: a cross-sectional online survey. Chin Med J (Engl) 2012;125:1867-70. [PubMed]
- Wu B, Liu M, Liu H, et al. Meta-analysis of traditional Chinese patent medicine for ischemic stroke. Stroke 2007;38:1973-9.


