
No free lunch—the price of double versus triple antithrombotic therapy in patients with atrial fibrillation after ACS or PCI
The optimal antithrombotic therapy after coronary stenting in patients with atrial fibrillation (AF) remains a clinical conundrum (1). Most patients with AF require life-long oral anticoagulation to reduce the risk of ischemic stroke and/or extracranial thromboembolism (2). Direct oral anticoagulants (DOACs) constitute today the best therapeutic option for preventing cardio-embolic events while reducing the risk of intracranial hemorrhage compared with vitamin K antagonists (VKAs) (2). Patients with acute coronary syndrome (ACS) or undergoing percutaneous coronary intervention (PCI) are all candidates to dual antiplatelet therapy consisting of aspirin and P2Y12 inhibitors to prevent the recurrence of platelet-mediated coronary events, especially those related to the stent (3,4). This therapeutic strategy prevents stent thrombosis by a greater extent (over 5-folds risk reduction) than aspirin alone or aspirin combined with oral anticoagulants (5,6). As many as 20% to 40% of patients with AF undergo PCI and, from the reverse perspective, 5% to 10% of patients candidate to PCI present with AF (1). The coexistence of the two conditions complicates the therapeutic approach because combining an oral anticoagulant with dual antiplatelet therapy into the so-called triple antithrombotic therapy increases the risk of fatal and nonfatal bleeding (7). As a potential alternative, a modified—double—antithrombotic regimen, combining oral anticoagulation with a single antiplatelet agent (usually a P2Y12 inhibitor), has been proposed to reduce the risk of bleeding while preventing ischemic events. In the contemporary setting of DOACs, four randomized-controlled trials investigated a triple versus double therapy in patients with AF receiving PCI: the PIONEER AF-PCI (8), the RE-DUAL PCI (9), the AUGUSTUS (10), and the ENTRUST AF-PCI (11).
In the AUGUSTUS trial (10), Lopes and colleagues randomly assigned—with a two-by-two factorial design—4,614 patients with AF after ACS or following PCI to receive (I) apixaban 5 mg bid or VKAs (open-label comparison), and (II) aspirin or matching placebo (blinded comparison). Patients were followed up for 6 months to evaluate for a primary (safety) endpoint of major or clinically relevant non-major bleeding according to the International Society on Thrombosis and Hemostasis criteria, and secondary (efficacy) endpoints including the composite of death, hospitalization or death, and ischemic events [myocardial infarction (MI), stroke, urgent revascularization, or stent thrombosis]. According to the design of the study, double antithrombotic regimen consisted of apixaban plus a P2Y12 inhibitor (93% clopidogrel, 6% ticagrelor, and 1% prasugrel) reached through an early drop of aspirin. At 6 months, the primary endpoint was significantly reduced by apixaban compared with VKAs [hazard ratio (HR) 0.69; 95% confidence interval (CI): 0.58–0.81; P<0.001], and increased by aspirin compared with placebo (HR 1.89; 95% CI: 1.59–2.24; P<0.001). Moreover, apixaban associated with a lower risk of death or hospitalization than VKAs (HR 0.83; 95% CI: 0.74–0.93; P=0.002), while no difference was noted by comparing aspirin versus placebo.
By means of its design and inclusion/exclusion criteria, the AUGUSTUS trial adds numerous insights into the findings of the other DOAC-based trials (10). By randomizing patients in a two-by-two factorial fashion, the trial specifically addressed the individual impact of DOACs and aspirin withdrawal, demonstrating that both aspects worth in terms of bleeding prevention. Contrarily, the PIONEER AF-PCI, RE-DUAL PCI, and ENTRUST AF-PCI trials only partly answered this clinical question as, according to the design of the studies, it was not possible to determine whether the safety benefit of a double strategy was due to the use of a DOAC-based strategy or early aspirin discontinuation. Besides, the AUGUSTUS also included a proportion of patients with medically managed ACS (about one-quarter of study participants), who are known to be at high risk for future events, expanding current knowledge in this particular setting. However, findings from the AUGUSTUS did not provide evidence that early omission of aspirin is safe in all patients, nor clearly indicated the optimal timing for the transition from triple to double therapy. First, an initial period of triple antithrombotic therapy before randomization was granted to all patients in all the trials, for a maximum of 14 days in the AUGUSTUS, 5 days in the RE-DUAL PCI and ENTRUST AF-PCI, and 3 days in the PIONEER AF-PCI. Thus, the effect of a very early (or peri-procedural) aspirin discontinuation remains actually unexplored and should not be pursued. Moreover, in the AUGUSTUS, while a reduction in the risk of bleeding was shown in patients on placebo compared with those on aspirin, a signal for an absolute increase in the risk of MI, definite/probable stent thrombosis, and urgent revascularization, and was detected. For stent thrombosis, this rate was almost doubled when aspirin was early discontinued (HR 0.58, 95% CI: 0.28–1.22), with the majority of events (80%) occurring within 30 days of PCI (12). Whether the extensive use of clopidogrel and its variable response and efficacy (particularly without aspirin) played a relevant role in this setting remains uncertain. The consistency of the trends toward more coronary events in the placebo than in the aspirin group strongly supports the biological plausibility of the finding and suggests that a significant difference would likely be detected if more patients had been enrolled. Indeed, the AUGUSTUS (as the other trials) was largely underpowered to reliably detect differences in this respect considering that, in contemporary practice, cardiac and cerebrovascular ischemic events are roughly ten-fold less prevalent than bleeding occurrences (adopted as the primary endpoint in all these studies).
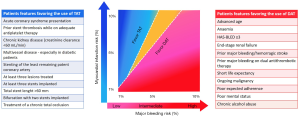
To tackle this relevant open-issue, a recent meta-analysis pooled aggregate data from the four DOAC-based trials (13). In a total population of 10,234 patients, double antithrombotic therapy, consisting of a DOAC and a P2Y12 inhibitor, significantly reduced bleeding events, including major and intracranial hemorrhages, while it increased the risk of MI and stent thrombosis with a statistical borderline and significant effect, respectively. These findings carry relevant clinical implications. First, given the totality and consistency of results, DAOCs should be prioritized in all patients with AF who have an ACS or receive PCI, as a superior safety over VKAs appears to be a class effect. Second, the increase in ischemic cardiac events with double therapy highlights (once again) the importance of a precise and fully individualized approach in deciding the duration of the initial course of triple therapy in these patients (14). Individual risk factors of bleeding and ischemic events continuously interact with each therapeutic intervention and should be comprehensively taken into account in the selection of the optimal antithrombotic regimen (14,15). The exercise to carefully assess clinical, laboratory, and procedural factors that are known to influence major bleeding and myocardial infarction remains essential to predict the net benefit/harm for each individual patient and guide decision-making (Figure 1). In patients deemed at low risk of cardiac ischemic events (i.e., those receiving elective PCI, without high-risk clinical or angiographic features) or at high risk of major bleeding, early discontinuation of aspirin and treatment with a DAOC combined with clopidogrel is warranted (3). Conversely, in patients presenting with ACS, high thrombotic burden, undergoing complex, high-risk, or multivessel PCI, continuing aspirin should be advised for at least several weeks or longer, and triple therapy duration tailored to patient’s bleeding risk (3) (Figure 1). Although treatment simplification is attractive, dropping aspirin very early is unlikely to benefit all patients. The still enduring belief that a one-size-fits-all approach is the way forward should also probably be “dropped” in practice and trials.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform (available at http://dx.doi.org/10.21037/atm.2020.01.26). Dr. Valgimigli reports grants and personal fees from Abbott, personal fees from Bayer, personal fees from Daiichi Sankyo, personal fees from Amgen, grants and personal fees from Terumo, personal fees from Alvimedica, grants from Medicure, grants and personal fees from Astrazeneca, personal fees from Idorsia, personal fees from Coreflow, personal fees from Vifor, personal fees from Bristol Myers Squib SA, personal fees from iVascular, outside the submitted work. Dr. Gragnano reports a research grant from the European Society of Cardiology (ESC).
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Capodanno D, Huber K, Mehran R, et al. Management of Antithrombotic Therapy in Atrial Fibrillation Patients Undergoing PCI. J Am Coll Cardiol 2019;74:83-99. [Crossref] [PubMed]
- Lip GYH, Freedman B, De Caterina R, et al. Stroke prevention in atrial fibrillation: Past, present and future. Thromb Haemost 2017;117:1230-9. [Crossref] [PubMed]
- Valgimigli M, Bueno H, Byrne RA, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS: The Task Force for dual antiplatelet therapy in coronary artery disease of the European Society of Cardiology (ESC) and of the European. Eur Heart J 2018;39:213-60. [Crossref] [PubMed]
- Calabrò P, Gragnano F, Di Maio M, et al. Epidemiology and Management of Patients With Acute Coronary Syndromes in Contemporary Real-World Practice: Evolving Trends From the EYESHOT Study to the START-ANTIPLATELET Registry. Angiology 2018;69:795-802. [Crossref] [PubMed]
- Leon MB, Baim DS, Popma JJ, et al. A Clinical Trial Comparing Three Antithrombotic-Drug Regimens after Coronary-Artery Stenting. N Engl J Med 1998;339:1665-71. [Crossref] [PubMed]
- Schömig A, Neumann FJ, Kastrati A, et al. A Randomized Comparison of Antiplatelet and Anticoagulant Therapy after the Placement of Coronary-Artery Stents. N Engl J Med 1996;334:1084-9. [Crossref] [PubMed]
- Hansen ML, Sørensen R, Clausen MT, et al. Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillation. Arch Intern Med 2010;170:1433-41. [Crossref] [PubMed]
- Gibson CM, Mehran R, Bode C, et al. Prevention of Bleeding in Patients with Atrial Fibrillation Undergoing PCI. N Engl J Med 2016;375:2423-34. [Crossref] [PubMed]
- Cannon CP, Bhatt DL, Oldgren J, et al. Dual Antithrombotic Therapy with Dabigatran after PCI in Atrial Fibrillation. N Engl J Med 2017;377:1513-24. [Crossref] [PubMed]
- Lopes RD, Heizer G, Aronson R, et al. Antithrombotic Therapy after Acute Coronary Syndrome or PCI in Atrial Fibrillation. N Engl J Med 2019;380:1509-24. [Crossref] [PubMed]
- Vranckx P, Valgimigli M, Eckardt L, et al. Edoxaban-based versus vitamin K antagonist-based antithrombotic regimen after successful coronary stenting in patients with atrial fibrillation (ENTRUST-AF PCI): a randomised, open-label, phase 3b trial. Lancet 2019;394:1335-43. [Crossref] [PubMed]
- Lopes RD, Leonardi S, Wojdyla DM, et al. Stent Thrombosis in Patients with Atrial Fibrillation Undergoing Coronary Stenting in the AUGUSTUS Trial. Circulation 2020;141:781-3. [PubMed]
- Gargiulo G, Goette A, Tijssen J, et al. Safety and efficacy outcomes of double vs. triple antithrombotic therapy in patients with atrial fibrillation following percutaneous coronary intervention: a systematic review and meta-analysis of non-vitamin K antagonist oral anticoagulant-based randomized clinical trials. Eur Heart J 2019;40:3757-67. [PubMed]
- Gragnano F, Calabrò P, Valgimigli M. Is triple antithrombotic therapy, or rather its duration and composition, the true culprit for the excess of bleeding events observed in patients with atrial fibrillation undergoing coronary intervention? Eur Heart J 2019;40:216-7. [Crossref] [PubMed]
- Gragnano F, Manavifar N, Valgimigli M. A call for action in bleeding prevention. Aging (Albany NY) 2019;11:287-8. [Crossref] [PubMed]


