Quadriceps tendon autograft and platelet rich plasma injection to treat chronic Achilles tears—a minimum two-year follow-up
Introduction
Achilles tendon ruptures represent the most common acute tendon rupture in the human body (1), and frequently they are diagnosed solely based on clinical examination, but it is considered that up to 25% of them can be misdiagnosed by the first clinician who examines the patient (2). When they take more than 4–6 weeks to get correct diagnosis and treatment, they are referred to as chronic, neglected or delayed, and represent a challenging therapeutic problem due to the retraction and scarring of the tendon stumps, that create a gap that could be several centimeters long (3). Although there is no consensus regarding the specific time in which an acute tear becomes a chronic rupture, 4 weeks seems to be the most widely accepted interval (4). Regardless of the lack of a precise chronological definition, neglected ruptures are characterized by the difficulty of achieving an end-to-end apposition of the tendon ends with plantar flexion of the foot during surgical reconstruction.
In the past, several authors recommended the use of an inverted superficial turn-down flap of the gastrocnemius fascia to cover the defect (5-7). Many other authors have used different tissues to bridge the tendon gap, from local tendons, such as flexor hallucis longus (FHL) or peroneus brevis tendon (8,9), to distant tendons, such as the semitendinosus or gracilis tendons (10,11). Although the use of the quadriceps tendon for the treatment of chronic Achilles tendon ruptures was first published in 1995 (12), there are scarce further references to such technique (13), except to treat distal Achilles tendinosis and in fact, the technique used in our study was published in English literature in 2016 (14). One of the amplest revisions of the history of graft options for neglected Achilles tendon ruptures, published in 2008 did not even consider quadriceps tendon graft as an option for the treatment of tissue deficits in chronic Achilles tendon tears (15).
Some authors have published good results adding platelet rich plasma (PRP) to the operative procedure for the treatment of acute Achilles tendon ruptures (16), but our literature search could not find any publications on its use for the treatment of chronic Achilles tendon ruptures, and, to our knowledge, this is the first report on the results obtained combining the use of an autograft and PRP in this difficult condition.
There are no published reports on the results of the treatment of chronic Achilles tendon ruptures using bone-quadriceps tendon autografts, but it would be important for clinicians to know if it is a useful technique to treat such debilitating problem. We present the revision, after a minimum 2 years follow-up, of a case series of 8 patients who presented with a chronic Achilles tendon tears that were treated successfully with autologous bone-quadriceps tendon grafts enhanced with PRP.
Methods
This is a retrospective review of a prospectively designed database of a cohort of eight patients who presented chronic neglected ruptures of the Achilles tendon. All were active patients. Surgical treatment was done by means of an ipsilateral quadriceps autograft supplemented with PRP.
Inclusion criteria: chronic (more than 6 months) and symptomatic Achilles tendon rupture or re-rupture, patients previously active in sports. Exclusion criteria were active infection, non-athletes, ruptures located more than 7 cm from the calcaneus insertion of the tendon, or patients unwilling to enter the study protocol.
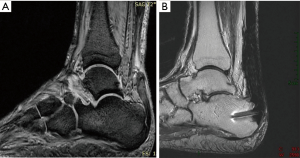
The technique has been used in 8 cases of chronic subcutaneous Achilles tendon ruptures. There were 6 men and 2 women, with a median age of 55 years (range, 43–72 years). Two patients played football (soccer), four were runners, and two were mountain-hikers before the injury; all of them were unable to practice sport when seen at the clinic before treatment. All patients had a noticeable weakness of active plantar flexion of the affected ankle, and walked with a limp; in all of them, a palpable defect in the tendon body was evident (Figure 1). The time from rupture to surgery was more than 6 months in all cases (range, 6–13 months), and minimum follow-up was 24 months (range, 24–51 months). After discussion of the surgical and non-surgical options available, the patients gave their informed consent to the procedure, using the quadriceps tendon as graft source. The preparation of the Leukocyte-Poor Platelet-Rich Plasma was elaborated according to PRGF technology (16). Briefly, 34 cc of peripheral blood was collected into 9 cc tubes containing 3.8% (wt/vol) sodium citrate; tubes were centrifuged at 640 g for 8 min and the 2-cc plasma fraction located just above the buffy coat was aspirated and dispensed into an empty tube under vertical air flow conditions. Few minutes prior to the infiltration, calcium chloride was added at a final concentration of 22.8 mM. The activated liquid was injected before coagulation, both into the graft and the borders of the Achilles tendon stumps for a distance of approximately 15 mm in each direction.
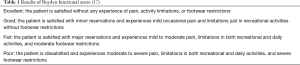
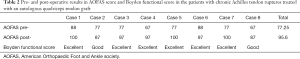
Results were evaluated using the American Orthopedic Foot and Ankle Society (AOFAS) score (11), and the 4-domain system described by Boyden et al. (17) evaluating pain, level of activity, footwear restrictions, and satisfaction, which had been previously validated and used by Maffulli et al. (18) (Table 1). Statistical analysis was done by the sign test for matched pairs and Wilcoxon signed-rank test. Alpha error was set at 0.05.
The study was approved by the Ethics Committee of the University of A Coruña with the number 22/2016.
Surgical technique
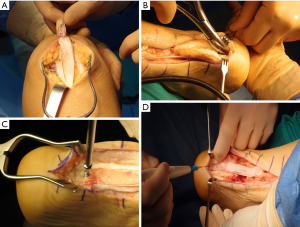
The surgical technique has been published previously (14). To avoid unnecessary movements during surgery, and to avoid the necessity of changing drapes, the patient is placed in a semi-lateral ventral decubitus on the uninjured side, tilted ventrally. The injured limb is prepped and draped free. Using external hip rotation, the ipsilateral knee can be positioned so that the patella is pointing to the ceiling, and the bone-tendon quadriceps graft can be harvested following the standard technique, to obtain the longest possible graft. We aimed to get a graft at least 10 mm in width, including a 12 mm long bone plug and 80–90 mm of tendon length (Figure 2). When knee incision is closed the patient can be rotated to full ventral decubitus, without requiring the change of drapes. Then, through a standard longitudinal incision, both the Achilles tendon and the calcaneal tuberosity are exposed. After necrotic and scarred tissue is debrided, a trough is created in the posterior aspect of the calcaneus (Figure 2B), where the bone plug from the patella is press-fitted and fixed with a 3.5 mm cancellous screw (Figure 2C). The quadriceps tendon graft is used to bridge the Achilles tendon gap (Figure 2D) and sutured to the proximal stump with enough tension to keep the foot in slight equinus position, and the longitudinally opened proximal and distal Achilles tendon stumps are sutured latero-laterally to the graft. Leukocyte-Poor Platelet-Rich Plasma is injected into the graft and the Achilles tendon stumps, and the wound is closed in a routine fashion. After surgery, the limb is placed in a short leg plaster cast keeping the plantar-flexed ankle position for 4 weeks. After cast removal, an orthosis with range of motion control was used, allowing free plantar flexion but limiting dorsal movement to −20º for two more weeks while allowing partial weight bearing. The orthosis was retired for night rest and physiotherapy, avoiding dorsiflexion above neutral until the 8th postoperative week. After 8 weeks, patients were weaned from the use of the orthosis.
Results
Preoperatively, patients showed an average AOFAS score of 77.25 (range, 67–88) (19). Patients were followed for a minimum of 24 months after surgery (range, 24–51 months). At last visit, AOFAS score showed a marked improvement in all the cases (Table 2), with AOFAS scores almost normal in most of them: average 95.6 (range, 87–100). Six of the eight patients resumed their previous athletic activity.
Full table
Improvement in AOFAS score results was statistically significant, both for sign test for matched pairs (P=0.008) and for Wilcoxon signed-rank test (P=0.012). The Boyden functional activity results are shown in Table 1. All of the patients were satisfied with the results of the procedure and would undergo it again, although 2 of them had only a good result. As complications of the procedure, it was necessary to retire two of the calcaneal screws (under local anesthesia) due to persistent discomfort and skin irritation corresponding to the head of the screws. No wound healing complications were noted. All patients showed some degree of persistent triceps surae atrophy, with a median calf gird difference of 1.7 cm. MRI and US scans showed full healing with homogeneous signal in all cases (Figure 1B).
Discussion
The main finding of this study is that autologous quadriceps bone-tendon graft offers an excellent option for the repair of chronic Achilles tendon ruptures.
The incidence of Achilles tendon ruptures has apparently increased during the past years (some authors have reported a four-fold frequency), probably due to the increase in the general population activity and sports participation (20). Even with the improvement in the awareness and diagnosis of the pathology by the primary care physicians, still some Achilles tendon ruptures will go unnoticed and become chronic tears. No matter whether non-operative or surgical treatment is used for the acute Achilles tendon rupture, some percentage of the patients will suffer unwanted complications that can include re-ruptures (in 5.6% of cases). In the case of surgically treated Achilles tendon tears, complications include infections and tissue necrosis (in 2.2% of cases) that could require further surgical procedures to correct the residual defect in the tendon (21).
Most authors agree that (as there is no “gold standard” for surgical reconstruction of chronic Achilles tendon tears), in order to achieve the optimal functional outcome and regardless of the chosen technique, the ultimate goal of surgical treatment is to restore the length tension relationship such that sufficient plantar flexion power is obtained (15).
Although numerous operative procedures have been proposed for the reconstruction of a chronic Achilles tendon rupture, most publications present only case series with small number of patients. Thus, there is no clear evidence to help surgeons to choose one method over the others (15). Keeping this in mind, autologous quadriceps tendon graft seems an excellent option that has not received as much attention for the treatment of this pathology as it would seem logical, considering the bone-tendon configuration of the graft, that makes it suitable for the reinforcement and grafting of the Achilles tendon (12). It is well known that quadriceps tendon autograft represents a reliable option for the treatment of several sports injuries, including anterior cruciate ligament (ACL) tears, and its use has seen a renewed interest recently. Advantages of the quadriceps tendon autograft include its excellent mechanical properties, the solid fixation that can be obtained using its bone plug if harvested as a bone-tendon unit, and the low morbidity associated with this procedure (22,23).
The use of a quadriceps bone-tendon graft allows to restore the Achilles tendon structural continuity without sacrificing other neighbor structures. It has the advantage that creates an "anatomical" repair, as the patellar bone plug can be fixed in the tendon footprint at the posterior calcaneal tuberosity, to avoid changing the traction vector of the tendon. All the above confer to the use of quadriceps tendon autograft advantages over other techniques that are used for the surgical treatment of chronic Achilles tendon tears and that sacrifice functionally agonistic tendons as grafts, or that fix the tendons in positions that do not follow exactly the Achilles traction line.
After surgery, as the skin vascularization might be compromised, placing the foot in a discrete equinus position helps to favor skin vascularization, while reducing the tension in the sutures that fix the graft to the host Achilles tendon tissue (24). Using PRP injected along the quadriceps tendon graft and the host tissue borders was done to promote tissue healing. In that sense, some authors have published a shorter recovery time after PRP injection in cases of operative repair of acute Achilles tendon ruptures in athletes (16). We could not find any published reports concerning the use of PRP to improve the results of the surgical repair of chronic Achilles tendon tears. Even though, we decided to use the PRP injection into the graft and host tissue borders because the biologic environment is not different to the one found in other operative procedures where bone and soft tissue autografts have been used, such as the cases of ACL repairs with autologous graft tissue. In such procedures, some authors have shown that the use of intraoperative PRP can promote an early integration and maturation of the graft (25).
The main limitation of our study is the short number of patients and their relatively high age, which might make that our results could not extrapolate to other populations.
Limitations of this procedure lie basically in the distance of the torn tendon gap from the calcaneus. If the gap is located more than 5–6 cm away from the calcaneus, the quadriceps graft might not have enough length to bridge it. Nevertheless, its length (usually, 8.5 cm on average) is longer than the obtained when harvesting the FHL tendon, which nowadays is one of the most popular grafts for chronic Achilles tendon reconstruction, due to its proximity to the Achilles tendon (26). Average length of the FHL graft, when harvested through a posterior incision, is only 5.16 cm (26). If the quadriceps tendon length is not enough to bridge the gap, other different surgical procedures, as the ones recently described using a free semitendinosus tendon graft (27,28), a scar tissue repair and FHL augmentation (29), or a free gastrocnemius aponeurosis flap (30), should be used.
Conclusions
The use of autologous Quadriceps tendon graft (in bone-tendon configuration) gives a reliable result for patients with tissue defects in the Achilles tendon. Due to its availability and low morbidity, it could be considered as a first choice of treatment in cases of chronic or neglected Achilles tendon ruptures. Autologous Quadriceps tendon graft could also be used to solve some of the surgical complications of Achilles tendon surgery (as deep infections or Achilles tendon necrosis or re-ruptures), without sacrificing other neighbor structures nor shortening the myotendinous triceps surae unit. It allows performing an "anatomical" repair, which might, in turn, allow a better force transmission.
Acknowledgments
The authors gratefully acknowledge the funding from the Catedra HM de Traumatología del Deporte y el Grupo de Investigación INCIDE de la Universidade da Coruña for the publication of this manuscript.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Ethics Committee of the University of A Coruña with the number 22/2016. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Inglis AE, Sculco TP. Surgical repair of ruptures of the tendo Achillis. Clin Orthop Relat Res 1981.160-9. [PubMed]
- Maffulli N. Rupture of the Achilles tendon. J Bone Joint Surg Am. 1999;81:1019-36. [Crossref] [PubMed]
- Leppilahti J, Orava S. Total Achilles tendon rupture. A review. Sports Med 1998;25:79-100. [Crossref] [PubMed]
- Porter DA, Mannarino FP, Snead D, et al. Primary repair without augmentation for early neglected Achilles tendon ruptures in the recreational athlete. Foot Ankle Int 1997;18:557-64. [Crossref] [PubMed]
- Abraham E, Pankovich AM. Neglected rupture of the Achilles tendon. Treatment by V-Y tendinous flap. J Bone Joint Surg Am 1975;57:253-5. [Crossref] [PubMed]
- Bosworth DM. Repair of defects in the tendo achillis. J Bone Joint Surg 1956;38-A:111-4. [Crossref] [PubMed]
- Christensen I. Rupture of the Achilles tendon; analysis of 57 cases. Acta Chir Scand 1953;106:50-60. [PubMed]
- Mann RA, Holmes GB, Seale KS, et al. Chronic rupture of the Achilles tendon: a new technique of repair. J Bone Joint Surg Am 1991;73:214-9. [Crossref] [PubMed]
- Pintore E, Barra V, Pintore R, et al. Peroneus brevis tendon transfer in neglected tears of the Achilles tendon. J Trauma 2001;50:71-8. [Crossref] [PubMed]
- Maffulli N, Leadbetter WB. Free gracilis tendon graft in chronic tears of the Achilles tendon. Clin J Sport Med 2005;15:56-61. [Crossref] [PubMed]
- Nilsson-Helander K, Sward L, Silbernagel KG, et al. A new surgical method to treat chronic ruptures and reruptures of the Achilles tendon. Knee Surg Sports Traumatol Arthrosc 2008;16:614-20. [Crossref] [PubMed]
- Besse JL, Lerat JL, Moyen B, et al. Distal reconstruction of the Achilles tendon with a bone-tendon graft from extensor system of the knee. Rev Chir Orthop Reparatrice Appar Mot 1995;81:453-7. [PubMed]
- Philippot R, Wegrzyn J, Grosclaude S, et al. Repair of insertional achilles tendinosis with a bone-quadriceps tendon graft. Foot Ankle Int 2010;31:802-6. [Crossref] [PubMed]
- Arriaza R, Gayoso R, López-Vidriero E, et al. Quadriceps autograft to treat Achilles Chronic tendon tears: a simple surgical technique. BMC Musculoskelet Disord 2016;17:116. [Crossref] [PubMed]
- Gove JR, Hardy MA. Autograft, Allograft and Xenograft Options in the Treatment of Neglected Achilles Tendon Ruptures: A Historical Review with Illustration of Surgical Repair. Foot Ankle J 2008;1:1-10.
- Sánchez M, Anitua E, Azofra J, et al. Comparison of surgically repaired Achilles tendon tears using platelet-rich fibrin matrices. Am J Sports Med 2007;35:245-51. [Crossref] [PubMed]
- Boyden EM, Kitaoka HB, Cahalan TD, et al. Late versus early repair of Achilles tendon rupture: clinical and biomechanical evaluation. Clin Orthop Relat Res 1995.150-8. [PubMed]
- Maffulli N, Loppini M, Longo UG, et al. Minimally Invasive Reconstruction of Chronic Achilles Tendon Ruptures Using the Ipsilateral Free Semitendinosus Tendon Graft and Interference Screw Fixation. Am J Sports Med 2013;41:1100-7. [Crossref] [PubMed]
- Kitaoka HB, Alexander IJ, Adelaar RS, et al. Clinical Rating Systems for the Ankle-Hindfoot, Midfoot, Hallux and Lesser Toes. Foot & Ankle Int 1994;15:349-53. [Crossref] [PubMed]
- Pajala A, Kangas J, Ohtonen P, et al. Rerupture and Deep Infection Following Treatment of Total Achilles Tendon Rupture. J Bone Joint Surg Am 2002;84:2016-21. [Crossref] [PubMed]
- Bergkvist D, Åström I, Josefsson PO, et al. Acute Achilles tendon rupture: a questionnaire follow-up of 487 patients. J Bone Joint Surg Am 2012;94:1229-33. [Crossref] [PubMed]
- DeAngelis JP, Fulkerson JP. Quadriceps tendon–a reliable alternative for reconstruction of the anterior cruciate ligament. Clin Sports Med 2007;26:587-96. [Crossref] [PubMed]
- Sheean AJ, Musahl V, Slone HS, et al. Quadriceps tendon autograft for arthroscopic knee ligament reconstruction: use it now, use it often. Br J Sports Med 2018;52:698-701. [Crossref] [PubMed]
- Poynton AR, O’Rourke K. An analysis of skin perfusion over the Achilles tendon in varying degrees of plantarflexion. Foot Ankle Int 2001;22:572-4. [Crossref] [PubMed]
- Vogrin M, Rupreht M, Dinevski D, et al. Effects of a platelet gel on early graft revascularization after anterior cruciate ligament reconstruction: a prospective, randomized, double-blind, clinical trial. Eur Surg Res 2010;45:77-85. [Crossref] [PubMed]
- Tashjian RZ, Hur J, Sullivan RF, et al. Flexor hallucis longus transfer for repair of chronic Achilles tendinopathy. Foot Ankle Int 2003;24:673-6. [Crossref] [PubMed]
- Maffulli N, Del Buono A, Spiezia F, et al. Less-Invasive Semitendinosus Tendon Graft Augmentation for the Reconstruction of Chronic Tears of the Achilles Tendon. Am J Sports Med 2013;41:865-71. [Crossref] [PubMed]
- Sarzaeem MM, Lemraski MMB, Safdari F. Chronic Achilles tendon rupture reconstruction using a free semitendinosus tendon graft transfer. Knee Surg Sports Traumatol Arthrosc 2012;20:1386-91. [Crossref] [PubMed]
- Lee KB, Park YH, Yoon TR, et al. Reconstruction of neglected Achilles tendon rupture using the flexor hallucis tendon. Knee Surg Sports Traumatol Arthrosc 2009;17:316-20. [Crossref] [PubMed]
- Richardson DR, Willers J, Cohen BE, et al. Evaluation of the hallux morbidity of single-incision flexor hallucis longus tendon transfer. Foot Ankle Int 2009;30:627-30. [Crossref] [PubMed]