
Proposed antithrombotic strategy for acute ischemic stroke with large-artery atherosclerosis: focus on patients with high-risk transient ischemic attack and mild-to-moderate stroke
Introduction
Acute ischemic stroke (AIS) is the most common type of stroke. Intravenous thrombolysis and endovascular therapy are considered to be effective treatments for AIS. Intravenous thrombolysis is recommended as the first choice (1), and endovascular therapy is usually used to treat large-vessel occlusions. However, only a few patients received intravenous thrombolysis or endovascular therapy due to strict time window, technology, and equipment limitations (2).
The latest guidelines recommend aspirin monotherapy for patients with AIS beyond the time window. Clopidogrel is recommended for patients with aspirin resistance (3,4). Antiplatelet therapy is still the main treatment for AIS with large-artery atherosclerosis (LAA) at home and abroad (5). Anticoagulant therapy is another treatment for AIS. Although anticoagulant therapy has been used for more than 50 years, its use is still controversial. A recent study showed that anticoagulant therapy could reduce stroke recurrence, pulmonary embolism, and deep vein thrombosis, but its efficacy was offset by a high incidence of symptomatic intracranial bleeding (6). Therefore, anticoagulant therapy is not recommended in the early stage of AIS. Defibrinogen therapy is recommended for patients with AIS who are not suitable for thrombolysis, especially those with high fibrinogen levels (3,4). However, clinical evidence for defibrinogen therapy is lacking.
As a common cause of AIS, LAA stroke shares similar pathogenesis with acute myocardial infarction (AMI). Importantly, LAA stroke is prone to aggravate, and once aggravated, it may cause disability and death. Recent studies confirmed the efficacy of dual antiplatelet therapy in treating high-risk transient ischemic attack (TIA) and minor stroke and further found that patients with LAA stroke might benefit more from dual antiplatelet therapy (7-9). Even if patients were given dual antiplatelet therapy, some of them still suffered from aggravation, disability, or even death. Preventing the aggravation in patients with AIS, especially those with LAA stroke, has become a hot issue in clinical research.
In theory, under the premise of controlling the risk of bleeding, the greater the intensity of antithrombotic therapy, the less the recurrence and aggravation of stroke. The present study proposed a new antithrombotic strategy for patients with TIA or mild stroke and LAA based on related clinical evidence, atherosclerotic thrombosis theory, antithrombotic treatment guidelines of AMI, and previous clinical studies.
Target population
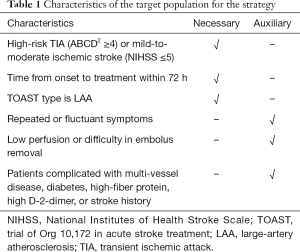
The characteristics of the target population for the strategy are shown in Table 1. The antithrombotic strategy proposed in this study is suitable for patients with high-risk TIA (ABCD2 ≥4) or mild stroke [National Institutes of Health Stroke Scale (NIHSS) ≤5]. Patients with NIHSS ≤5 are chosen as the target population due to two reasons. First, most of the minor strokes are defined as NIHSS ≤5. Second, patients with NIHSS ≤5 account for a large proportion of LAA stroke. Therefore, these patients could cover most patients in general (Table 1).
Full table
Proposed strategy
Early administration
In theory, the sooner the antithrombotic therapy is given, the sooner the therapy works to minimize the recurrence and aggravation of stroke. Patients have a high risk of recurrence and aggravation of stroke within 48 h from the onset. Hence, the diagnosis and treatment of stroke should be performed as soon as possible (10-12). Rothwell et al. (13) reported that among 2,416 patients with AIS, 23% had a TIA history, of which 17% occurred on the day of AIS onset, 9% on the previous day, and 43% within 7 days from the AIS onset. Large-sample studies showed that early treatment for patients with symptomatic TIA helped prevent stroke (14-16). Meanwhile, researchers indicated that compared with delayed treatment, early treatment did not increase the risk of intracranial hemorrhage or other organ hemorrhages (17). Therefore, early administration can help prevent or delay the occurrence of stroke in patients with TIA. Similarly, early administration can prevent the occurrence and aggravation of mild-to-moderate stroke.
The latest guidelines for ST-segment elevation myocardial infarction (STEMI) have recommended that patients with STEMI without aspirin contraindications should take aspirin as soon as possible (18,19). Providing antithrombotic therapy in the early stage to patients with STEMI can prevent the aggravation of STEMI and reduce the mortality of patients (20). Therefore, early administration as soon as possible should be recommended for LAA ischemic stroke as a crucial antithrombotic strategy.
Enhanced therapy
In clinical practice, a routine dose of antithrombotic drugs takes some time to achieve a relatively stable concentration. The drug achieves effective concentration rapidly at a loading dose to exert an antithrombotic effect as soon as possible, thus effectively reducing the recurrence and aggravation of stroke. A loading dose of 300 or 600 mg clopidogrel is usually used in clinical practice. Several studies have been performed to investigate the effect of dual antiplatelet therapy on ischemic stroke in recent years (21-23). The CHANCE trial showed that compared with aspirin monotherapy, clopidogrel plus aspirin treatment after a loading dose of clopidogrel could reduce the risk of recurrent stroke in patients with TIA or minor ischemic stroke (NIHSS 3) within 24 h of symptom onset (24), which was further demonstrated by POINTS trial (25). Besides, a loading dose has also been recommended in the guidelines for the treatment of STEMI (18,19). Overall, the loading dose strategy is suitable for preventing the recurrence and aggravation of TIA or mild stroke with LAA.
Combination therapy
Eroded or disrupted atherosclerotic plaques have a significant impact on the development of thrombosis. Vascular plaques often form in the regions with low and oscillatory shear forces, causing chronic minimal endothelial damage or dysfunction. Smooth muscle cells invade these early plaques, producing connective tissue fibrils that form a fibrous cap over the lipid center. The rupture of this cap is the main cause of thrombosis (26,27). The thrombus formed early is white in color, which is mainly formed by platelet aggregation. With the decrease in blood flow velocity and the increase in clotting factor, the blood gradually clots, and then the thrombus changes into red and mixed thrombi (28). Therefore, antiplatelet combined with anticoagulant therapy is an optimal antithrombotic strategy to prevent thrombus formation in patients with LAA. Antiplatelet therapy is used mainly for white thrombosis, and the anticoagulant therapy is used mainly for red thrombosis. In theory, the combination of antiplatelet and anticoagulant therapy achieves the best synergistic effect of antithrombotic therapy in LAA stroke.
Currently, the most commonly used anticoagulant drugs are warfarin and new oral anticoagulants such as rivaroxaban and dabigatran. The COMPASS trial reported that among patients with stable atherosclerotic vascular disease, those who received rivaroxaban combined with aspirin therapy had better cardiovascular outcomes compared with those who received aspirin therapy only (29). Warfarin combined with antiplatelet therapy is the standard therapy for patients with atrial fibrillation after a percutaneous coronary intervention (PCI), but this strategy might increase the risk of bleeding. Cannon et al. (30) demonstrated that among patients with atrial fibrillation who had undergone PCI, patients who received dual therapy with dabigatran had a lower risk of bleeding compared with those who received triple therapy with warfarin. A recent study found that compared with antiplatelet therapy alone, antiplatelet combined with anticoagulant therapy did not increase the risk of hemorrhage in acute mild stroke with LAA (unpublished data).
Short-term therapy
Although combination therapy can prevent thrombosis expansion and stroke aggravation, it increases the risk of bleeding. The risk of stroke aggravation within 1 week from stroke onset is the highest (24). Thus, short-term (3–5 days) combination therapy was proposed in this study, which could not only fully cover the high-risk period of stroke but also decrease the risk of bleeding due to combination antithrombotic treatment. The CHANCE study confirmed that the optimal time for dual antiplatelet therapy was about 14 days (31). In this study, antiplatelet combined with anticoagulant therapy was given for 3–5 days and then converted into dual antiplatelet therapy. Based on the SAMPRIS study, patients with LAA stroke should be given dual antiplatelet therapy for 3 months (32).
Sequential therapy
Sequential therapy refers to changing the same drug from intravenous injection to oral medication, or changing the drug while maintaining the same efficacy (33,34). Intravenous administration is more effective and suitable for patients who cannot take drugs orally. Changing intravenous to oral administration has some advantages, such as convenient application, low price, and fewer adverse reactions caused by an injection. Sequential therapy has been widely used in antibiotic therapy for several years (35-37). It is used for treating gastritis and pneumonia in recent years. However, sequential therapy is less mentioned for treating cerebrovascular diseases. It is proposed that sequential therapy should be used for patients with LAA stroke, which involves giving an intravenous injection at first and then changing it to oral medication, for example changing intravenous antiplatelet (such as tirofiban) or anticoagulant (such as argatroban) administration to oral medication (such as aspirin/clopidogrel).
Our clinical study
Our recent single-center study compared the efficacy and safety of dual antiplatelet therapy versus aspirin alone in treating AIS within 72 h of onset (38). A total of 690 patients aged ≥40 years were identified for enrollment. This study showed that compared with antiplatelet monotherapy, early dual antiplatelet therapy could reduce neurological deterioration in patients with AIS. The ongoing ATAMIS trial (NCT02869009) aims to evaluate the efficacy and safety of clopidogrel plus aspirin therapy versus aspirin monotherapy within 48 h of the symptom onset of mild-to-moderate ischemic stroke. The study is a randomized, open-label, multicenter, prospective trial with a target enrollment of 2,700 patients from 60 centers in Northeast China (39). Our recently completed study (NCT03552354) compared the efficacy and safety of short-term argatroban combined with antiplatelet (3–5 days) versus antiplatelet alone in treating LAA AIS within 72 h of onset. The results showed that compared with antiplatelet alone, short-term argatroban combined with antiplatelet did not increase the risk of intracranial hemorrhage or other organic hemorrhages, thus preventing stroke aggravation. Taken together, the clinical studies further supported the use of the proposed antithrombotic strategy for the given population.
In conclusion, this study proposed this “early administration, enhanced therapy, combination therapy, short-term therapy, and sequential therapy” antithrombotic strategy for patients with LAA stroke, especially high-risk TIA and mild-to-moderate AIS patients. It is believed that the proposed therapy is an effective and safe antithrombotic strategy to prevent the recurrence and aggravation of stroke, thus reducing disability and death in the said population. Multicenter randomized trials should be conducted to confirm the use of antithrombotic strategy.
Acknowledgments
The authors would like to thank Lin Tao, Yu Cui, and Xiaofu Tian for their support in this study.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Wardlaw JM, del Zoppo G, Yamaguchi T. Thrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev 2000.CD000213. [PubMed]
- Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med 2008;359:1317-29. [Crossref] [PubMed]
- Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2018;49:e46-e110. [Crossref] [PubMed]
- Neurology branch of Chinese Medical Association. Guidelines for the diagnosis and treatment of acute ischemic stroke in China 2014. Chin J Neurol 2015;48:246-57.
- Sandercock P, Gubitz G, Foley P, et al. Antiplatelet therapy for acute ischaemic stroke. Cochrane Database Syst Rev 2003.CD000029. [PubMed]
- Sandercock PA, Counsell C, Kane EJ. Anticoagulants for acute ischaemic stroke. Cochrane Database Syst Rev 2015.CD000024. [PubMed]
- Wang C, Yi X, Zhang B, et al. Clopidogrel plus aspirin prevents early neurologic deterioration and improves 6-month outcome in patients with acute large artery atherosclerosis stroke. Clin Appl Thromb Hemost 2015;21:453-61. [Crossref] [PubMed]
- Yi X, Lin J, Wang C, et al. A comparative study of dual versus monoantiplatelet therapy in patients with acute large-arteryatherosclerosis stroke. J Stroke Cerebrovasc Dis 2014;23:1975-81. [Crossref] [PubMed]
- Kim D, Park JM, Kang K, et al. Dual versus mono antiplatelet therapy in large atherosclerotic stroke. Stroke 2019;50:1184-92. [Crossref] [PubMed]
- Howard VJ, McClure LA, Meschia JF, et al. High prevalence of stroke symptoms among persons without a diagnosis of stroke or transient ischemic attack in a general population: the REasons for Geographic And Racial Differences in Stroke (REGARDS) study. Arch Intern Med 2006;166:1952-8. [Crossref] [PubMed]
- Toole JF, Lefkowitz DS, Chambless LE, et al. Self-reported transient ischemic attack and stroke symptoms: methods and baseline prevalence. The ARIC Study, 1987-1989. Am J Epidemiol 1996;144:849-56. [Crossref] [PubMed]
- Howard G, Safford MM, Meschia JF, et al. Stroke symptoms in individuals reporting no prior stroke or transient ischemic attack are associated with a decrease in indices of mental and physical functioning. Stroke 2007;38:2446-52. [Crossref] [PubMed]
- Rothwell PM, Warlow CP. Timing of TIAs preceding stroke: time window for prevention is very short. Neurology 2005;64:817-20. [Crossref] [PubMed]
- Hart CL, Hole DJ, Smith GD. The relation between questions indicating transient ischaemic attack and stroke in 20 years of follow up in men and women in the Renfrew/Paisley Study. J Epidemiol Community Health 2001;55:653-6. [Crossref] [PubMed]
- Rothwell PM, Algra A, Chen Z, et al. Effects of aspirin on risk and severity of early recurrent stroke after transient ischaemic attack and ischaemic stroke: time-course analysis of randomised trials. Lancet 2016;388:365-75. [Crossref] [PubMed]
- Lavallée PC, Meseguer E, Abboud H, et al. A transient ischaemic attack clinic with round-the-clock access (SOS-TIA): feasibility and effects. Lancet Neurol 2007;6:953-60. [Crossref] [PubMed]
- Rothwell PM, Giles MF, Chandratheva A, et al. Effect of urgent treatment of transient ischaemic attack and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet 2007;370:1432-42. [Crossref] [PubMed]
- Cardiology branch of Chinese Medical Association. Guidelines for the diagnosis and treatment of ST-segment elevation myocardial infarction. Chin J Cardiol 2015;43:380-93.
- O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2013;127:e362-425. [PubMed]
- Théroux P. Antithrombotic treatment of acute coronary syndromes. Can J Cardiol 1998;14 Suppl E:6E-10E.
- Ge F, Lin H, Liu Y, et al. Dual antiplatelet therapy after stroke or transient ischaemic attack - how long to treat? The duration of aspirin plus clopidogrel in stroke or transient ischaemic attack: a systematic review and meta-analysis. Eur J Neurol 2016;23:1051-7. [Crossref] [PubMed]
- Wang Z, Xu C, Wang P, et al. Combined clopidogrel-aspirin treatment for high risk TIA or minor stroke does not increase cerebral microbleeds. Neurol Res 2015;37:993-7. [Crossref] [PubMed]
- Li Z, Wang Y, Zhao X, et al. Treatment effect of clopidogrel plus aspirin within 12 hours of acute minor stroke or transient ischemic attack. J Am Heart Assoc 2016;5:e003038. [Crossref] [PubMed]
- Wang Y, Wang Y, Zhao X, et al. Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med 2013;369:11-9. [Crossref] [PubMed]
- Johnston SC, Easton JD, Farrant M, et al. Clopidogrel and aspirin in acute ischemic stroke and high-risk TIA. N Engl J Med 2018;379:215-25. [Crossref] [PubMed]
- Fuster V, Badimon JJ, Chesebro JH. Atherothrombosis: mechanisms and clinical therapeutic approaches. Vasc Med 1998;3:231-9. [Crossref] [PubMed]
- Rauch U, Osende JI, Fuster V, et al. Thrombus formation on atherosclerotic plaques: pathogenesis and clinical consequences. Ann Intern Med 2001;134:224-38. [Crossref] [PubMed]
- Kirchhof K, Welzel T, Mecke C, et al. Differentiation of white, mixed, and red thrombi: value of CT in estimation of the prognosis of thrombolysis phantom study. Radiology 2003;228:126-30. [Crossref] [PubMed]
- Eikelboom JW, Connolly SJ, Bosch J, et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med 2017;377:1319-30. [Crossref] [PubMed]
- Cannon CP, Bhatt DL, Oldgren J, et al. Dual antithrombotic therapy with dabigatran after PCI in atrial fibrillation. N Engl J Med 2018;378:485-6. [PubMed]
- Pan Y, Jing J, Chen W, et al. Risks and benefits of clopidogrel-aspirin in minor stroke or TIA: Time course analysis of CHANCE. Neurology 2017;88:1906-11. [Crossref] [PubMed]
- Chimowitz MI, Lynn MJ, Turan TN, et al. Design of the stenting and aggressive medical management for preventing recurrent stroke in intracranial stenosis trial. J Stroke Cerebrovasc Dis 2011;20:357-68. [Crossref] [PubMed]
- Quintiliani R, Cooper BW, Briceland LL, et al. Economic impact of streamlining antibiotic administration. Am J Med 1987;82:391-4. [PubMed]
- Barlow GD, Nathwani D. Sequential antibiotic therapy. Curr Opin Infect Dis 2000;13:599-607. [Crossref] [PubMed]
- Omidvari K, de Boisblanc BP, Karam G, et al. Early transition to oral antibiotic therapy for community-acquired pneumonia: duration of therapy, clinical outcomes, and cost analysis. Respir Med 1998;92:1032-9. [Crossref] [PubMed]
- Talan DA, Stamm WE, Hooton TM, et al. Comparison of ciprofloxacin (7 days) and trimethoprim-sulfamethoxazole (14 days) for acute uncomplicated pyelonephritis pyelonephritis in women: a randomized trial. JAMA 2000;283:1583-90. [Crossref] [PubMed]
- Karwowska A, Davies HD, Jadavji T. Epidemiology and outcome of osteomyelitis in the era of sequential intravenous-oral therapy. Pediatr Infect Dis J 1998;17:1021-6. [Crossref] [PubMed]
- He F, Xia C, Zhang JH, et al. Clopidogrel plus aspirin versus aspirin alone for preventing early neurological deterioration in patients with acute ischemic stroke. J Clin Neurosci 2015;22:83-6. [Crossref] [PubMed]
- Hou X, Li X, Wang X, et al. Antiplatelet Therapy in Acute Mild-Moderate Ischemic Stroke (ATAMIS): a parallel, randomised, open-label, multicentre, prospective study. Stroke Vasc Neurol 2018;3:263-7. [Crossref] [PubMed]


