
Psychological distress and health-related quality of life in patients with bone marrow edema syndrome
Introduction
Bone marrow edema syndrome (BMES) is a painful disease with pathological increase of the interstitial fluid in bone, usually affecting a joint (1). BMES occurs preferentially in the lower extremity in men (3:1) aged 20–40 years (2). Because BMES is often diagnosed late and attempts at treatment are frequently unsuccessful, 80% of patients develop osteonecrosis (ON) 3–18 months after onset. In some cases, this even necessitates joint replacement (3-8). ON is a global health-care burden. According to this, there are 15,000 to 20,000 new cases of ON each year in the USA alone and studies showed that the average prevalence was 28.91 per 100,000 populations in Korea (9). In 2004 the number of patients who sought medical care for ON in Japan was about 11,400 (10). Besides this, Bergman et al. showed that the incidence rate was 4.7 cases per 10,000 among patients 50 years and older in Sweden in 2005 (11). Additionally, in the United Kingdom the incidence of ON ranges from about 1.4 to 3.0/100,000 including data from approximately 3.4 million active patients (12). On top of this, Zhao et al. estimated that there are 8.12 million cases with ON of the femoral head among Chinese people aged 15 years and older (13). It is thought that 10–12% of all total hip replacements are due to ON (2,14-16).
Chen et al. recently determined that female patients with ON in the proximal femur are at a higher risk of anxiety and depression (17). Anxiety and depression limit the ability to work, worsen the health-related quality of life (HrQoL), and thus lead to socio-economic problems (18). It has not yet been established whether psychological distress (anxiety and depression) plays a part in the genesis of ON or is already present in the early stages of ON (i.e., BMES).
The primary aim of the present study was therefore to investigate psychological distress and self-reported HrQoL in patients with BMES. The hypothesis was that patients with BMES that has not yet progressed to ON are more likely to suffer anxiety or depression than the normal population and also have poorer HrQoL. A secondary goal was to find out whether HrQoL or psychological distress is affected by the stage or site of the disease.
Methods
Patients and study design
This retrospective study was conducted at the University Hospital Jena/Orthopaedic Department, Campus Eisenberg, Thuringia, Germany and included patients with the diagnosis of BMES of the proximal femur or the knee joint who were treated in our hospital in 2016 or 2017. Those whose treatment was less than 12 months ago were excluded. The selection criterion in screening the electronic medical records was diagnosis M87.* according to the International Statistical Classification of Diseases and Related Health Problems (ICD-10-GM, German Modification).
Patients with previous joint replacement surgery were excluded.
Standard treatment of patients with BMES
Following a standard treatment schemeJeny (3,19)), all patients were admitted to the hospital and received a 5-day course of intravenous Iloprost (Ilomedin, Bayer Schering, Germany). Patients with Association Research Circulation Osseous (ARCO) stage ≥2 were additionally treated with surgical decompression beforehand (4). In all patients only partial loading of the affected joint (max. 15 kg weight bearing using two forearm crutches) was permitted for 6 weeks after treatment.
Data acquisition
All patients were given a questionnaire for self-reporting of psychological distress and HrQoL. The Hospital Anxiety and Depression Scale (HADS) was used to document anxiety and depression and the five-level version of the EuroQol Group’s EQ-5D instrument (EQ-5D-5L) to assess HrQoL. The established cut-offs described in the literature were employed to categorize patients as suffering from anxiety or depression (≥11 for anxiety and ≥9 for depression) (20). The EQ-5D-5L index was used to evaluate the EQ-5D-5L results. A mean value of 0.91 (health status of the South Australian population) was taken as reference for the normal population and corresponds approximately to the health status of the local population (21). Moreover, the visual analog scale of the EQ-5D-5L (EQ-VAS) was used. Ratings on this scale of 0 to 100 mm represent a global evaluation of the self-perceived health status, where 0 stands for the worst imaginable and 100 for the best imaginable state of health (21-24).
The data published by Hinz et al. in 2011 (25) (for more than 4,400 persons) and McCaffrey et al. in 2016 (24) (more than 2,900 persons), also acquired by means of HADS und EQ-5D-5L (EQ-VAS), served as reference/control group for comparison.
Furthermore, we documented the following parameters: radiological stage of BMES according to ARCO, based on radiography and preinterventional magnetic resonance imaging (MRI) (26); site of edema (hip or knee); presence of vascular disease, hypertension, diabetes mellitus, or lipid metabolism disorders; nicotine or alcohol consumption (yes/no); sex (female/male); body mass index (BMI); age group (15–24, 25–34, 35–44, 45–54, 55–64, 65–74, 75+ years).
Data analysis
With regard to the primary hypothesis, psychological distress was evaluated by comparing the rates of anxiety and depression in the study group and the control cohort. Based on the parameters EQ-VAS and EQ-5D-5L index, the effect of the disease on HrQoL was compared by age group and sex between patients with BMES and the control group.
Secondarily, we analyzed the influence of disease stage and site of edema (hip or knee joint) on the results of HADS and EQ-5D-5L in the BMES group.
Statistical analysis
Statistical analysis was performed with GraphPad Prism V.5.0a (GraphPad Software Inc., San Diego, USA) and SPSS V.24 (IBM, Armonk, USA). Continuous parameters were tested with a two-sided, two-way ANOVA, or a two-sided unpaired t-test, categorical parameters with Fisher’s exact test. The level of significance was set to P=0.05.
Results
Demographic characteristics
Of the 104 patients with the diagnosis of BMES who were identified and contacted in writing, 56 (53.8%; 26 females, 30 males) completed and returned the questionnaires. Their mean age was 55.8 years (range, 15–84 years). Further demographic and patient-specific data can be found in Table 1.

Full table
Anxiety and depression
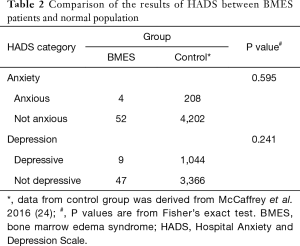
There was no significant difference between the study group and the control cohort in the rate of either anxiety (P=0.595) or depression (P=0.241; Table 2).
Full table
HrQoL
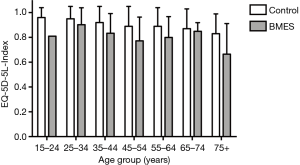
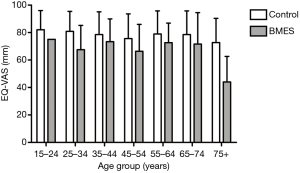
Compared with the healthy controls, the patients with BMES had significantly poorer HrQoL on both parameters (EQ-5D-5L index: PBMES <0.001; EQ-VAS: PBMES =0.001; Figures 1,2). The age group also had an effect on HrQoL (EQ-5D-5L index: Page =0.036; EQ-VAS: Page =0.040), but showed no interaction with that of the disease (EQ-5D-5L index: PBMES × age =0.816; EQ-VAS: PBMES × age =0.542). The patient’s sex exerted no influence on the results (EQ-5D-5L index: Pgender =0.755, PBMES × gender =0.162; EQ-VAS: Pgender =0.416, PBMES × gender =0.602).
Influence of site and stage of disease
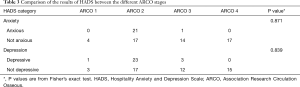
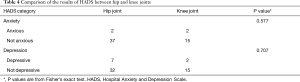
The influence of the site of edema and the ARCO stage on the HADS results is shown in Tables 3,4.
Full table
Full table
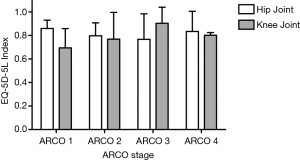
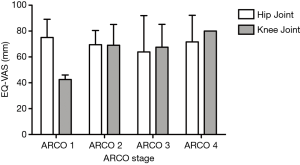
Neither the joint affected by edema nor the radiological disease stage had a significant effect on HrQoL in terms of EQ-5D-5L index (PARCO =0.900, Pjoint =0.738, PARCO × joint =0.592; Figure 3) or EQ-VAS (PARCO =0.501, Pjoint =0.483, PARCO × joint =0.383; Figure 4).
Discussion
The aim of the present study was to determine the psychological distress and the self-reported HrQoL in patients with BMES compared with the normal population. The secondary goal was to investigate the influence of disease stage and edema site on the outcome parameters. To the best of our knowledge we are the first to demonstrate the presence of a marked worsening of HrQoL, irrespective of age or sex, in BMES, the precursor of ON. In contrast to our hypothesis, however, the BMES patients did not show elevated rates of anxiety and depression. There was also no difference with regard to the joint involved or the radiological stage of BMES.
Earlier studies demonstrated that BMES causes pain and functional impairment (19). Our study confirms these findings in relation to the worsening of self-reported HrQoL owing to pain and functional impairment. Strikingly, the worsening of HrQoL was evident despite the elapse of at least 1 year since treatment. One explanation for this may be the fact that in many cases the detection and treatment of BMES took several weeks or even months. This can be associated with a degree of chronification of pain in the patients concerned. The International Association for the Study of Pain (IASP) defines chronic pain as “pain that has persisted beyond the normal tissue healing time (usually taken to be 3 months) (27). Thus, the typical evolution of BMES almost inevitably leads to chronic pain, which is then reflected in the HrQoL.
The prevalence of anxiety and depression in the patients with BMES was much lower than in the patients with ON described by Chen et al. (17). While the rates of anxiety (7.1%; 4/56 patients) and depression (16.1%; 9/56 patients) in BMES patients do not differ essentially from those of the normal population, the published prevalence in patients with ON seem to be much higher (anxiety: 20.4%, 44/216 patients; depression: 21.8%, 47/216 patients). It can be assumed that, due to the short duration of the disease, a chronic pain disorder has not yet developed and for this reason anxiety and/or depression have not yet progressed. It is well known from other diseases like low back pain that anxiety and depression are strongly linked to the chronicity of pain (27,28). Therefore, either anxiety or depression increase with the progression of the disease and the development of ON, or BMES is particularly likely to progress to ON in a subgroup of patients prone to anxiety and depression. Thus, one can conclude from the data that anxiety and depression are probably not causal factors for BMES, but it remains open whether anxiety, depression, and psychological distress caused by chronic pain, for example, can trigger progress to ON or whether they are a consequence of the disease. The results of a small-animal study by Henneicke et al. suggest the former. Using a mouse model, they found that chronic stress triggered an increase in serum glucocorticoid concentrations, which in turn led to increased osteoclast activity with elevation of bone resorption (29). In a recently published review, Harth and Nielson summarized data demonstrating how inflammatory joint diseases such as osteoarthritis are greatly intensified by the psychological distress resulting from chronic pain (30).
Although other risk factors such as elevated serum lipids or excessive biomechanical loading in obese patients seem to be primarily responsible for the pathogenesis of BMES (31), associations have nevertheless been demonstrated between the accepted risk factors, e.g., obesity, and psychological distress (32). However, it appears that this tends to play a relevant part in the progression to ON only with increasing duration of disease.
Our study is not without limitations. First, because the numbers of patients with anxiety or depression are relatively small, the power may be insufficient to document a corresponding difference, especially in the subgroups for ARCO stages or individual joints. Second, owing to the study design one can only speculate regarding the further progression of individual patients towards ON. Third, this was a retrospective study at an isolated point in time. No conclusions can be drawn concerning the course of the disease over time. Finally, the control cohort is from a different population (South Australia), so bias cannot be excluded with certainty. Nevertheless, the mean EQ-5D-5L index, for example, is almost identical in the two populations (South Australia vs. Germany) (21).
Conclusions
In conclusion, it can be stated that although patients with BMES already demonstrate with decreased HrQoL, this is not (yet) expressed in psychological distress (clinically significant anxiety and depression). Based on the knowledge of increased prevalence of anxiety and depression in patients with ON and the high likelihood of development of a chronic pain syndrome in BMES, patients with BMES, particularly those who score highly for anxiety and depression, should receive psychological counseling alongside their standard treatment.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the local ethics committee under rule number 5494-04/18/18.
References
- Geith T, Niethammer T, Milz S, et al. Transient Bone Marrow Edema Syndrome versus Osteonecrosis: Perfusion Patterns at Dynamic Contrast-enhanced MR Imaging with High Temporal Resolution Can Allow Differentiation. Radiology 2017;283:478-85. [Crossref] [PubMed]
- Pountos I, Giannoudis PV. The role of Iloprost on bone edema and osteonecrosis: Safety and clinical results. Expert Opin Drug Saf 2018;17:225-33. [Crossref] [PubMed]
- Röhner E, Zippelius T, Steindl D, et al. Effects of intravenous iloprost therapy in patients with bone marrow oedema of the foot and ankle. Eur J Orthop Surg Traumatol 2014;24:1609-16. [Crossref] [PubMed]
- Maus U, Roth A, Tingart M, et al. S3 Guideline. Part 3: Non-Traumatic Avascular Necrosis in Adults - Surgical Treatment of Atraumatic Avascular Femoral Head Necrosis in Adults. Z Orthop Unfall 2015;153:498-507. [PubMed]
- Vande Berg B, Lecouvet F, Koutaissoff S, et al. Bone marrow edema of the femoral head. JBR-BTR 2007;90:350-7. [PubMed]
- Elder GJ. From marrow oedema to osteonecrosis: common paths in the development of post-transplant bone pain. Nephrology (Carlton) 2006;11:560-7. [Crossref] [PubMed]
- Meizer R, Radda C, Stolz G, et al. MRI-controlled analysis of 104 patients with painful bone marrow edema in different joint localizations treated with the prostacyclin analogue iloprost. Wien Klin Wochenschr 2005;117:278-86. [Crossref] [PubMed]
- Symptomatic multifocal osteonecrosis. A multicenter study. Collaborative Osteonecrosis Group. Clin Orthop Relat Res 1999.312-26. [PubMed]
- Kang JS, Park S, Song JH, et al. Prevalence of osteonecrosis of the femoral head: a nationwide epidemiologic analysis in Korea. J Arthroplasty 2009;24:1178-83. [Crossref] [PubMed]
- Fukushima W, Fujioka M, Kubo T, et al. Nationwide epidemiologic survey of idiopathic osteonecrosis of the femoral head. Clin Orthop Relat Res 2010;468:2715-24. [Crossref] [PubMed]
- Bergman J, Nordström A, Nordström P. Epidemiology of osteonecrosis among older adults in Sweden. Osteoporos Int 2019;30:965-73. [Crossref] [PubMed]
- Cooper C, Steinbuch M, Stevenson R, et al. The epidemiology of osteonecrosis: findings from the GPRD and THIN databases in the UK. Osteoporos Int 2010;21:569-77. [Crossref] [PubMed]
- Zhao DW, Yu M, Hu K, et al. Prevalence of Nontraumatic Osteonecrosis of the Femoral Head and its Associated Risk Factors in the Chinese Population: Results from a Nationally Representative Survey. Chin Med J (Engl) 2015;128:2843-50. [Crossref] [PubMed]
- Lavernia CJ, Sierra RJ, Grieco FR. Osteonecrosis of the femoral head. J Am Acad Orthop Surg 1999;7:250-61. [Crossref] [PubMed]
- Steinberg ME, Hayken GD, Steinberg DR. A quantitative system for staging avascular necrosis. J Bone Joint Surg Br 1995;77:34-41. [Crossref] [PubMed]
- Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am 1995;77:459-74. [Crossref] [PubMed]
- Chen SB, Hu H, Gao YS, et al. Prevalence of clinical anxiety, clinical depression and associated risk factors in chinese young and middle-aged patients with osteonecrosis of the femoral head. PLoS One 2015;10:e0120234. [Crossref] [PubMed]
- Chisholm D, Sweeny K, Sheehan P, et al. Scaling-up treatment of depression and anxiety: a global return on investment analysis. Lancet Psychiatry 2016;3:415-24. [Crossref] [PubMed]
- Zippelius T, Perka C, Preininger B, et al. Long-term effects of intravenous iloprost therapy in patients with bone marrow oedema of the hip. Acta Orthop Belg 2018;84:172-8. [PubMed]
- Bjelland I, Dahl AA, Haug TT, et al. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res 2002;52:69-77. [Crossref] [PubMed]
- Hinz A, Kohlmann T, Stöbel-Richter Y, et al. The quality of life questionnaire EQ-5D-5L: psychometric properties and normative values for the general German population. Qual Life Res 2014;23:443-7. [Crossref] [PubMed]
- Janssen MF, Bonsel GJ, Luo N. Is EQ-5D-5L Better Than EQ-5D-3L? A Head-to-Head Comparison of Descriptive Systems and Value Sets from Seven Countries. Pharmacoeconomics 2018;36:675-97. [Crossref] [PubMed]
- Janssen MF, Szende A, Cabases J, et al. Population norms for the EQ-5D-3L: a cross-country analysis of population surveys for 20 countries. Eur J Health Econ 2019;20:205-16. [Crossref] [PubMed]
- McCaffrey N, Kaambwa B, Currow DC, et al. Health-related quality of life measured using the EQ-5D-5L: South Australian population norms. Health Qual Life Outcomes 2016;14:133. [Crossref] [PubMed]
- Hinz A, Brähler E. Normative values for the hospital anxiety and depression scale (HADS) in the general German population. J Psychosom Res 2011;71:74-8. [Crossref] [PubMed]
- Schmitt-Sody M, Kirchhoff C, Mayer W, et al. Avascular necrosis of the femoral head: inter- and intraobserver variations of Ficat and ARCO classifications. Int Orthop 2008;32:283-7. [Crossref] [PubMed]
- Classification of chronic pain. Descriptions of chronic pain syndromes and definitions of pain terms. Prepared by the International Association for the Study of Pain, Subcommittee on Taxonomy. Pain Suppl 1986;3:S1-226. [PubMed]
- Verhaak PF, Kerssens JJ, Dekker J, et al. Prevalence of chronic benign pain disorder among adults: a review of the literature. Pain 1998;77:231-9. [Crossref] [PubMed]
- Henneicke H, Li J, Kim S, et al. Chronic Mild Stress Causes Bone Loss via an Osteoblast-Specific Glucocorticoid-Dependent Mechanism. Endocrinology 2017;158:1939-50. [Crossref] [PubMed]
- Harth M, Nielson WR. Pain and affective distress in arthritis: relationship to immunity and inflammation. Expert Rev Clin Immunol 2019;15:541-52. [Crossref] [PubMed]
- Lim YZ, Wang Y, Wluka AE, et al. Association of obesity and systemic factors with bone marrow lesions at the knee: a systematic review. Semin Arthritis Rheum 2014;43:600-12. [Crossref] [PubMed]
- Sinha R, Jastreboff AM. Stress as a common risk factor for obesity and addiction. Biol Psychiatry 2013;73:827-35. [Crossref] [PubMed]


