
Avoiding desaturation during endotracheal intubation: is high-flow nasal cannula the answer?
Tracheal intubation in critically ill patients is a common procedure in the intensive care unit (ICU), and often is realized in an emergency scenario. Hypoxemia, hypotension, arrhythmia and cardiac arrest are described as severe adverse events related to the procedure, with an incidence around 28% (1,2). Among these intubation-related adverse events, life-threatening hypoxemia and profound desaturation (SpO2 below 80%) are the most frequent ones (3).
For several years, desaturation during intubation and the consequent need of preoxygenation has been discussed (4). Preoxygenation before intubation is used as standard of care in the majority of the ICUs, and the goal is to prolong the time until desaturation during apnea, earning time to safely perform the procedure, and avoiding hypoxemia. In healthy patients, preoxygenation can result in several minutes of apnea without desaturation, however, critically ill patients frequently have a decreased functional residual capacity (FRC), low hemoglobin levels, and decreased alveolar ventilation and cardiac output, leading to faster desaturation during apnea (3).
The effectiveness of preoxygenation can be defined by its efficacy and efficiency. The efficiency is the rate of decrease in oxyhemoglobin desaturation during apnea, while efficacy is the capacity of increase the alveolar fraction of oxygen and decrease the alveolar fraction of nitrogen (5,6). The rate of oxyhemoglobin desaturation is highly sensitive to the initial alveolar fraction oxygen and, therefore, adequate efficacy is better assessed measuring end-tidal oxygen concentration (EtO2) (7,8).
Peripheral oxygen saturation (SpO2) can be a misleading guide for preoxygenation, since a SpO2 of 100% can occur before the lungs are properly denitrogenated. Also, SpO2 starts to decrease only after the oxygen reserve is already depleted, thus, EtO2 monitoring during intubation is considered standard of care in the operating room (6,9). Nevertheless, measurements of the EtO2 must be performed with a sealed system and non-occlusive devices, such as high-flow nasal cannula (HFNC), are not adequate for it (10).
To improve safety during intubation, current guidelines suggest preoxygenation using oxygen through facemask, continuous positive airway pressure (CPAP), noninvasive ventilation (NIV) or nasal catheters with 10 to 15 liters of oxygen per min (L/min). In addition, the concentration of oxygen should be 100% for 3 minutes before laryngoscopy, aiming at an EtO2 higher than 90%. The best choice between the devices is not clear, but it is suggested that CPAP should be selected when oxygenation is impaired, and that HFNC or NIV should be kept during the procedure when already in use before it (2). Moreover, a systematic review of clinical trials suggests a possible benefit of pre-oxygenation with NIV and/or HFNC over oxygen alone in ICU patients (11).
HFNC is a popular device due its worldwide use in neonatal setting and is a relatively new method for respiratory support in adult patients. The device gained popularity in the ICU due to its ability to improve oxygenation, increase FRC, and offer a high inspiratory flow with higher and accurate measurement of the inspired fraction of oxygen (FiO2). In addition, HFNC induces a modest positive end-expiratory pressure effect when the mouth is closed, and is well tolerated by the patients, resulting in good comfort even with flows up to 60 L/min (12,13).
During intubation, HFNC may improve safety because it can offer not only adequate preoxygenation, but also apneic oxygenation during the procedure. Nasal prongs can be left in place during the entire intubation, offering oxygen at the pharyngeal level, while standard bag-valve mask (SMO) must be removed during laryngoscopy (3). In previous studies, apneic oxygenation was associated with increased peri-intubation SpO2, decreased rates of hypoxemia, and increased first-pass intubation (14-16).
In this context, Guitton et al., designed a randomized clinical trial to evaluate the benefits of HFNC in the preoxygenation of non-severely hypoxemic patients undergoing endotracheal intubation. The study, known as the PROTRACH trial, was a multicenter, randomized and open-label clinical trial. In the intervention arm, HFNC was maintained throughout the whole intubation procedure, while in the control group SMO was used during the preoxygenation but removed during laryngoscopy, as usual. The primary outcome was the lowest SpO2 during the procedure. Secondary outcomes were the incidence of desaturation (defined according to different cut-offs of SpO2), rate of difficult intubation, intubation difficulty scale score, need to proceed to face mask ventilation to correct desaturation, intubation-related adverse events [classified as severe (death, cardiac arrest, SpO2 <80% and/or severe hypotension)] or moderate [arrhythmia requiring intervention, esophageal intubation, aspiration of gastric content and/or dental injury)], organ failure during the first 5 days, time on ventilator, ICU length of stay, occurrence of ventilator-associated pneumonia, and 28-day mortality (17).
Patients were randomized from April 2016 to June 2017 in 7 French ICUs and followed for 28 days after randomization. Non-severe hypoxemia, defined as a PaO2/FiO2 <200 up to 4 hours before inclusion in the study was used as a key inclusion criterion, and the patients randomized were mainly in comatose state and intubated because of neurologic reasons. In the intention-to-treat analysis, the median lowest SpO2 was similar in both groups (100% in the HFNC vs. 99% in the SMO group; P=0.300), while mild desaturation (SpO2 <95%) was less frequent in the HFNC group [12% vs. 23%; relative risk (RR) 0.51, 95% confidence interval (CI): 0.26–0.99; P=0.045]. During intubation, the incidence of at least one intubation-related adverse event was lower in the HFNC group (6% vs. 19%; RR 0.31, 95% CI: 0.13–0.76; P=0.007), as was the incidence of severe complications (6% vs. 16%; RR 0.38, 95% CI: 0.15–0.95; P=0.030). Multivariable analysis showed that HFNC was associated with less desaturation, less intubation-related adverse events, and there was a trend towards reduced incidence of a SpO2 <80%. The authors concluded that during intubation of non-severely hypoxemic patients in the ICU, HFNC did not improved the median lowest SpO2 compared to SMO, however, HFNC was as associated with increased safety, leading to a reduction in intubation-related adverse events (17).
In line with these findings, Miguel-Montanes et al., conducted a single center before-after study, including non-hypoxemic patients mainly requiring intubation because of shock or coma, and found that HFNC significantly improved preoxygenation and reduced the prevalence of severe hypoxemia compared with SMO (18). In hypoxemic patients, Baillard et al., found that preoxygenation using NIV is more effective at decreasing the incidence of desaturation than SMO and, since then, NIV has been considered a useful approach for intubation of hypoxemic patients in the ICU (11). In 2015, the PREOXYFLOW trial evaluated the impact of HFNC compared to SMO for preoxygenation in severely hypoxemic patients (median PaO2/FiO2 of 120 mmHg), and no significant differences between the devices were found (19). Moreover, in 2016, the OPTINIV study showed that in severely hypoxemic patients, the preoxygenation with NIV combined with HFNC increased the lowest SpO2 during intubation compared to NIV alone (20). Finally, recently the FLORALI-2 study compared the use of NIV versus HFNC for the preoxygenation of patients with acute hypoxemic respiratory failure and found no difference between the devices in the risk of severe hypoxemia. However, in patients with PaO2/FiO2 ≤200, severe hypoxemia occurred in 24% of the patients in the NIV group and 35% of the patients in the HFNC group (absolute difference estimate −11.3%, 95% CI: −22.3 to 0.3; P=0.055), suggesting a possible benefit of NIV among this group of patients (21).
It is important to emphasize that these studies evaluated different populations. As shown in Table 1, the studies comparing HFNC to SMO in non-hypoxemic patients found better results in patients undergoing HFNC, while the trials evaluating severely hypoxemic patients did not find this association (17-19). Furthermore, for hypoxemic patients, the OPTINIV and the FLORALI-2 trials found better results for preoxygenation with NIV or combining NIV and HFNC compared to the devices alone. Hence, it is possible to infer from the data that HFNC provides better oxygenation during intubation of non-hypoxemic patients but, in severely hypoxemic patients, it might not be enough to prevent desaturation. This hypothesis can be supported by the physiological fact that hypoxemic patients usually have a higher amount of alveoli collapsed, and HFNC may not provide sufficient pressure to recruit these alveoli and prevent further collapse.
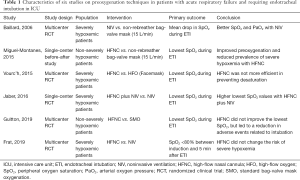
Full table
A recent trial comparing preoxygenation with HFNC vs. SMO in patients undergoing general anesthesia for surgery, found that HFNC is not a reliable method of preoxygenation before the induction of anesthesia. In this study, only 4% of the patients in the HFNC group achieved an EtO2 equal or greater than 90% after 3 minutes, while 54% of the patients in the face mask group reached the expected EtO2. The measurements of EtO2 were performed by exchanging the HFNC for a face mask while the subject held their breath at end inspiration and the EtO2 was assessed after a deep expiration and, due to the possibility of leaks during this exchange, the values of EtO2 could have been inaccurate. According to the authors, the reasons for the difference in oxygenation among the devices are the occurrence of air leaks through the mouth and a high inter-individual variability in the EtO2 values measured in the HFNC group (22).
The PROTRACH study has some limitations. First, the preoxygenation device was unblinded what may have interfered in the findings. Although difficult to be performed in a large sample of patients, the blinding is feasible and has been done previously (20). Second, the study did not compare HFNC to NIV, and NIV may have beneficial effects even in non-hypoxemic patients, although the risk of gastric aspiration and the significant number of patients with contraindications to NIV, such as those with neurological impairment should be considered. Third, the outcomes were based on the SpO2 and it may not reflect effectiveness of preoxygenation as discussed previously. Nevertheless, measuring EtO2 is not easy in patients undergoing HFNC and exchanging devices is not feasible in an emergency intubation.
In conclusion, the PROTRACH trial provides the best evidence until the moment comparing SMO and HFNC for preoxygenation of non-severely hypoxemic patients. Despite neutral for its primary outcome, the study demonstrated a potential benefit with the use of HFNC regarding the prevention of intubation-related adverse events. Given the small number of adverse events, these findings must be confirmed in well powered studies. Meanwhile, HFNC can be considered instead of SMO for the preoxygenation of non-severely hypoxemic patients, especially in intubations performed due to neurologic impairment, when NIV is commonly contraindicated.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Jaber S, Amraoui J, Lefrant JY, et al. Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Crit Care Med 2006;34:2355-61. [Crossref] [PubMed]
- Higgs A, McGrath BA, Goddard C, et al. Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth 2018;120:323-52. [Crossref] [PubMed]
- Ricard JD. Hazards of intubation in the ICU: role of nasal high flow oxygen therapy for preoxygenation and apneic oxygenation to prevent desaturation. Minerva Anestesiol 2016;82:1098-106. [PubMed]
- Weitzner SW, King BD, Ikezono E. The rate of arterial oxygen desaturation during apnea in humans. Anesthesiology 1959;20:624-7. [Crossref] [PubMed]
- Benumof JL. Preoxygenation: best method for both efficacy and efficiency. Anesthesiology 1999;91:603-5. [Crossref] [PubMed]
- Nimmagadda U, Salem MR, Crystal GJ. Preoxygenation: Physiologic Basis, Benefits, and Potential Risks. Anesth Analg 2017;124:507-17. [Crossref] [PubMed]
- Farmery AD, Roe PG. A model to describe the rate of oxyhaemoglobin desaturation during apnoea. Br J Anaesth 1996;76:284-91. [Crossref] [PubMed]
- Hanouz JL, Gerard JL, Fischer MO. Nasal high-flow preoxygenation for endotracheal intubation in the critically ill patient? Con. Intensive Care Med 2019;45:526-8. [Crossref] [PubMed]
- Langeron O, Bourgain JL, Francon D, et al. Difficult intubation and extubation in adult anaesthesia. Anaesth Crit Care Pain Med 2018;37:639-51. [Crossref] [PubMed]
- Benumof JL, Herway ST. High End-Tidal Oxygen Concentration Can Be a Misleading Sole Indicator of the Completeness of Preoxygenation. Anesth Analg 2017;124:2093. [Crossref] [PubMed]
- Cabrini L, Landoni G, Baiardo Radaelli M, et al. Tracheal intubation in critically ill patients: a comprehensive systematic review of randomized trials. Crit Care 2018;22:6. [Crossref] [PubMed]
- Papazian L, Corley A, Hess D, et al. Use of high-flow nasal cannula oxygenation in ICU adults: a narrative review. Intensive Care Med 2016;42:1336-49. [Crossref] [PubMed]
- Corley A, Rickard CM, Aitken LM, et al. High-flow nasal cannulae for respiratory support in adult intensive care patients. Cochrane Database Syst Rev 2017;5:CD010172. [PubMed]
- Binks MJ, Holyoak RS, Melhuish TM, et al. Apneic oxygenation during intubation in the emergency department and during retrieval: A systematic review and meta-analysis. Am J Emerg Med 2017;35:1542-6. [Crossref] [PubMed]
- Oliveira J E Silva L, Cabrera D, Barrionuevo P, et al. Effectiveness of Apneic Oxygenation During Intubation: A Systematic Review and Meta-Analysis. Ann Emerg Med 2017;70:483-94.e11. [Crossref] [PubMed]
- Pavlov I, Medrano S, Weingart S. Apneic oxygenation reduces the incidence of hypoxemia during emergency intubation: A systematic review and meta-analysis. Am J Emerg Med 2017;35:1184-9. [Crossref] [PubMed]
- Guitton C, Ehrmann S, Volteau C, et al. Nasal high-flow preoxygenation for endotracheal intubation in the critically ill patient: a randomized clinical trial. Intensive Care Med 2019;45:447-58. [Crossref] [PubMed]
- Miguel-Montanes R, Hajage D, Messika J, et al. Use of high-flow nasal cannula oxygen therapy to prevent desaturation during tracheal intubation of intensive care patients with mild-to-moderate hypoxemia. Crit Care Med 2015;43:574-83. [Crossref] [PubMed]
- Vourc'h M, Asfar P, Volteau C, et al. High-flow nasal cannula oxygen during endotracheal intubation in hypoxemic patients: a randomized controlled clinical trial. Intensive Care Med 2015;41:1538-48. [Crossref] [PubMed]
- Jaber S, Monnin M, Girard M, et al. Apnoeic oxygenation via high-flow nasal cannula oxygen combined with non-invasive ventilation preoxygenation for intubation in hypoxaemic patients in the intensive care unit: the single-centre, blinded, randomised controlled OPTINIV trial. Intensive Care Med 2016;42:1877-87. [Crossref] [PubMed]
- Frat JP, Ricard JD, Quenot JP, et al. Non-invasive ventilation versus high-flow nasal cannula oxygen therapy with apnoeic oxygenation for preoxygenation before intubation of patients with acute hypoxaemic respiratory failure: a randomised, multicentre, open-label trial. Lancet Respir Med 2019;7:303-12. [Crossref] [PubMed]
- Hanouz JL, Lhermitte D, Gerard JL, et al. Comparison of pre-oxygenation using spontaneous breathing through face mask and high-flow nasal oxygen: A randomised controlled crossover study in healthy volunteers. Eur J Anaesthesiol 2019;36:335-41. [PubMed]


