
Total bilirubin is negatively related to diabetes mellitus in Chinese elderly: a community study
Introduction
Disease spectrum has significantly changed in the past 100 years, and noncommunicable diseases (NCD) including diabetes mellitus (DM), cancer and cardiovascular diseases have become the major cause of death worldwide. DM has been one of the most important NCD and threatens the human health worldwide. The statistics from International Diabetes Federation (IDF) show there were 370 million DM cases worldwide in 2011, and there will be 550 million DM cases in 2030. Oxidative stress plays important roles in the occurrence and development of DM. A variety of studies have shown that glucose overload may induce oxidative stress, causing damage to cells (1-3). However, the clinical intervention with vitamin E, a widely accepted anti-oxidant, fails to achieve favorable efficacy in DM patients (4).
Bilirubin is an end product in the metabolism of heme and has been confirmed to possess potential anti-oxidative activity (5) and be negatively related to oxidative stress (6,7). Especially, in the hydrophobic cell membrane, bilirubin is better to preserve the stability of proteins in cell membrane as compared to glutathione. In addition, both bound and unbound bilirubin has anti-oxidative activity (8). Although bilirubin at a high level is toxic to nervous system, a large number of studies have revealed that bilirubin at appropriate elevated level is beneficial. Japanese studies have indicated that bilirubin is negatively associated with peptide C, glycated hemoglobin and type 2 DM (T2DM) in middle-aged and old people (9). There is also evidence indicating that elevated bilirubin is able to reduce the incidence of DM and metabolic syndrome (10).
The incidence of DM increases over age, and the prevalence of DM increases by 68% with an increment of 10 years after adjusting for other factors (11). However, the age-span is larger than 20 years (12) or middle-aged/old people are recruited (9) in available studies on the relationship between bilirubin and DM. In addition, some subjects in these studies have some risk factors for vascular diseases or other comorbidities (such as Gilbert syndrome and chronic kidney diseases) (13-17). Thus, this cross-sectional study was undertaken to investigate the predictive value of serum total bilirubin (TB) and to explore the relationship between serum TB and DM in people older than 65 years of East China.
Methods
Subjects
This cross-sectional study was conducted in 11 communities of Shanghai Pudong New Area between January 2014 and March 2014. People who were 65 years or older and had been residents for at least 5 years were recruited. A total of 3,876 subjects were included in this study, and the medical history was recorded (birth date, time of physical activity, smoking and drinking). Smoker was defined as smoking every day or with an interval of several days and use of more than 100 cigarettes in life. Drinking was defined as use of 20–30 g of alcohol every day for men or 10–20 g of alcohol every day for women. Subjects with a history of diseases {clinically or laboratory-proven severe systemic diseases (cancer, renal failure and heart failure), goiter, liver dysfunction [aspartate aminotransferase (AST) or alanine aminotransferase (ALT) higher than three times upper normal limit such as 120 U/L or TB higher than 17.1 µmol/L], HIV infection}, bodybuilders, professional athlete and amateur athletes were excluded from this study. The past history was collected with a standardized questionnaire. History of DM was defined as the use of antidiabetic drugs or insulin. A history of coronary heart disease (CHD) was defined as 50% stenosis of coronary artery in coronary angiography or a history of acute myocardial infarction. Hypertension was defined as systolic blood pressure (SBP) of ≥140 mmHg, diastolic blood pressure (DBP) of ≥90 mmHg or a history of use of antihypertensive drugs. Informed consent was obtained from each subject before study.
Anthropometric parameters
Subjects were asked to wear light clothes and stock alone during the measurement of height and body weight. Subjects were asked to rest for 10 min, the blood pressure was measured twice and a mean was calculated. Abdominal circumference was measured at the middle point between the lower edge of ribs and the iliac crest. The neck circumference was measured at the upper Adam’s apple when the subject was asked to look straightly with the head horizontal. The body mass index (BMI) was calculated as body weight/height (kg/m2).
Measurement of biomarkers
Venous blood was collected from subjects after overnight fasting and processed for the measurement of fasting blood glucose, TG and TC, TB and ALT. Blood was stored at –80 °C.
Statistical analysis
Quantitative data with normal distribution are expressed as mean ± standard deviation, quantitative data with abnormal distribution as quartiles, qualitative data as rates. Comparisons among groups were done with analysis of variance, and qualitative data were compared with nonparametric tests. Subjects were divided into four groups with identical sample size according to the serum TB quartiles [Q1 (the lowest TB), Q2, Q3, Q4]. In every serum TB quartile [Q1, ≤8.70 (n=1,011); Q2, 8.70–10.80 (n=946); Q3, 10.80–13.30 (n=956); and Q4, 13.30–17.10 (n=963)], the prevalence of DM was calculated. Binary Logistic regression analysis was employed to explore the independent predictors of DM. A value of P<0.05 was considered statistically significant, and statistical analysis was performed with SPSS version 13.0 (SPSS, Chicago, IL, USA).
Results
Characteristics at baseline
A total of 3,876 subjects were recruited into this study. There were 1,685 males (43.5%) with the mean age of 71.14±6.06 years and 2,191 females with the mean age of 70.93±6.43. There were 558 DM patients. Demography, lifestyles and general clinical information of DM and non-DM patients are shown in Table 1. There was no difference in gender and smoking and drinking history between DM and non-DM patients. Average age, weight, and BMI were higher in DM patients than non-DM patients (P<0.005). Prevalence of CHD history and high blood pressure (HBP) history was higher in DM patients than non-DM patients (P<0.001). SBP, TC, and fasting plasma glucose (FPG) were higher in DM patients than non-DM patients (P<0.001), while TG was lower in DM patients than non-DM patients (P<0.001). There was no difference in ALT between DM patients and non-DM patients, while there was a significant difference in TB between DM patients and non-DM patients (P=0.001).
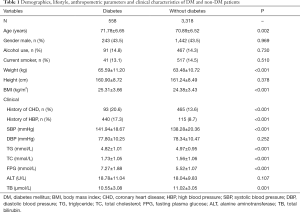
Full table
Relationship between TB and risk for DM
According to the TB quartiles, the prevalence of DM is shown in Table 2. Results showed the prevalence of DM in old people had a linear relationship with TB quartiles: the prevalence of DM reduced with the increase in serum TB (P=0.004).

Full table
Independent risk factors of DM with logistic regression analysis
Binary Logistic regression analysis showed age, TB, TG, BMI and history of hypertension were the independent risk factors of DM (Table 3): the prevalence of DM reduced by 18% with an increment of 1 µmol/L in TB [odds ratio (OR): 0.876, 95% confidence interval (CI): 0.807–0.951; P=0.002].
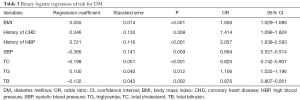
Full table
Discussion
In this cross-sectional study, 3,876 people aged ≥65 years were recruited from Chinese Eastern communities to investigate the relationship between physiological serum TB and DM. Our results showed physiological serum TB was an independent risk factor of DM in old people; the prevalence of DM in old people was linearly related to TB quartile; the prevalence of DM reduced with the increase in physiological serum TB.
Ko et al. for the first time reported the negative relationship between serum bilirubin and impaired glucose tolerance in 1996 (18). A variety of studies confirm that elevated bilirubin may reduce the risk for DM and improve the outcome of DM patients (12,19,20). In recent years, a large epidemiological study from Korea investigated 93,909 subjects and results showed high serum bilirubin level was closely related to low risk for DM (21). The NHANES study of USA also indicates that the incidence of DM in subjects with serum bilirubin higher than 10 micromole/liter is reduced by 20% as compared to those with serum bilirubin of <10 micromole/liter (12). However, both studies focused on the adolescents and old people. In this study, people older than 65 years were recruited, and results showed physiological serum bilirubin was negatively related to the prevalence of DM in them. This indicates that bilirubin plays a protective role in the occurrence and development of DM. Clinical and observational studies have revealed that the increased bilirubin may reduce the risk for DM by 26–31% (12,22). In the present study, the increased TB reduced the risk for DM by 18%. In our study, subjects with prior diagnosis of DM were included, and those with newly diagnosed DM were excluded. In addition, the serum bilirubin was in physiological range in our study, and subjects with comorbidities (such as Gilbert syndrome) were also excluded in the analysis of relationship between bilirubin and DM.
The protective role of bilirubin in DM is mainly ascribed to the anti-oxidative activity of bilirubin (23-26). Available studies have shown that TB in the physiological range may inhibit the damage of hyperglycemia-induced free radicals to cells (27). In addition, bilirubin may prevent vascular endothelial cells against oxidative stress (28,29). In animal experiments, biliverdin, the precursor of bilirubin, was found to prevent impaired glucose tolerance from deterioration (30). In adults with normal serum bilirubin, bilirubin accounts for about 10% of total anti-oxidative capacity and is negatively related to the serum markers of oxidative stress (31,32). These findings provide biological basis for the negative relationship between serum TB and DM. Bilirubin as an endogenous antioxidant (26,32,33) is negatively related to oxidative stress (7,34). Thus, the reduced prevalence of DM may be ascribed to the anti-oxidative activity of bilirubin.
Patients with T2DM usually have concomitant dyslipidemia (35). Some cross-sectional studies confirm that T2DM patients have a high incidence of dyslipidemia (36,37). Dyslipidemia may facilitate the development of atherosclerosis, which increases the risk of cardiovascular events in T2DM patients (38). Our findings were inconsistent with previously reported, which might be ascribed to the wide use of statins. Active lipid-lowering treatment is needed for DM patients, and serum lipid in physiological range is beneficial for DM patients.
There were still limitations in this study. First, this was a cross-sectional study which may not explain the causal relationship. Second, aminotransferase, γ-glutamate transferase and markers of viral hepatitis were not detected in this study, and thus we could not evaluate the influence of liver injury on our results. Third, the history of statins treatment was not recorded. Hemoglobin A1c (HbA1c) was not collected in DM patients. In addition, although the information about lifestyle (such as drinking and smoking) was collected, the information was incomplete and their reliability was questioned; the TB was measured once, and repeated measurement is needed in future studies.
Conclusions
Taken together, this large community study indicates that serum TB is an independent risk factor of DM in old people of Chinese eastern communities; the prevalence of DM in old people reduces with the increase in physiological serum TB.
Acknowledgments
Funding: This study was supported by Scientific Research Fund of Shanghai Science Committee (No. 19401935700 and 17411967700), Health and Family Planning Commission of Hongkou District (No. 1802-1), Shanghai Minhang district health and family planning commission (great discipline of Shanghai Minhang District No. 2017MWDXK02).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study has been approved by the Ethics Committee of Shanghai Traditional Chinese and Western Medicine Hospital, Shanghai University of Traditional Chinese Medicine (201909801).
References
- Brownlee M. Biochemistry and molecular cell biology of diabetic complications. Nature 2001;414:813-20. [Crossref] [PubMed]
- Ceriello A, Motz E. Is oxidative stress the pathogenic mechanism underlying insulin resistance, diabetes, and cardiovascular disease? The common soil hypothesis revisited. Arterioscler Thromb Vasc Biol 2004;24:816-23. [Crossref] [PubMed]
- Robertson RP. Chronic oxidative stress as a central mechanism for glucose toxicity in pancreatic islet beta cells in diabetes. J Biol Chem 2004;279:42351-4. [Crossref] [PubMed]
- Myung SK, Ju W, Cho B, et al. Efficacy of vitamin and antioxidant supplements in prevention of cardiovascular disease: systematic review and meta-analysis of randomised controlled trials. BMJ 2013;346:f10. [Crossref] [PubMed]
- Duman H, Özyurt S. Low serum bilirubin levels associated with subclinical atherosclerosis in patients with obstructive sleep apnea. Interv Med Appl Sci 2018;10:179-85. [Crossref] [PubMed]
- Hasanein P, Ghafari-Vahed M, Khodadadi I. Effects of isoquinoline alkaloid berberine on lipid peroxidation, antioxidant defense system, and liver damage induced by lead acetate in rats. Redox Rep 2017;22:42-50. [Crossref] [PubMed]
- Vítek L, Schwertner HA. The heme catabolic pathway and its protective effects on oxidative stress-mediated diseases. Adv Clin Chem 2007;43:1-57. [Crossref] [PubMed]
- Tomaro ML, Batlle AM. Bilirubin: its role in cytoprotection against oxidative stress. Int J Biochem Cell Biol 2002;34:216-20. [Crossref] [PubMed]
- Ohnaka K, Kono S, Inoguchi T, et al. Inverse associations of serum bilirubin with high sensitivity C-reactive protein, glycated hemoglobin, and prevalence of type 2 diabetes in middle-aged and elderly Japanese men and women. Diabetes Res Clin Pract 2010;88:103-10. [Crossref] [PubMed]
- Wu Y, Li M, Xu M, et al. Low serum total bilirubin concentrations are associated with increased prevalence of metabolic syndrome in Chinese. J Diabetes 2011;3:217-24. [Crossref] [PubMed]
- Diabetes Mellitus Branch of Chinese Medical Association. Guideline for the prevention and treatment of Type 2 diabetes mellitus in China (2013). Chin J Diabet 2014;22:2-42.
- Cheriyath P, Gorrepati VS, Peters I, et al. High total bilirubin as a protective factor for diabetes mellitus: an analysis of NHANES data from 1999-2006. J Clin Med Res 2010;2:201-6. [PubMed]
- Chan KH, O'Connell RL, Sullivan DR, et al. Plasma total bilirubin levels predict amputation events in type 2 diabetes mellitus: the Fenofibrate intervention and event lowering in diabetes (FIELD) study. Diabetologia 2013;56:724-36. [Crossref] [PubMed]
- Deetman PE, Bakker SJ, Dullaart RP. High sensitive C-reactive protein and serum amyloid A are inversely related to serum bilirubin: effect-modification by metabolic syndrome. Cardiovasc Diabetol 2013;12:166. [Crossref] [PubMed]
- Deetman PE, Bakker SJ, Kwakernaak AJ, et al. The relationship of the anti-oxidant bilirubin with free thyroxine is modified by insulin resistance in euthyroid subjects. PLoS One 2014;9:e90886. [Crossref] [PubMed]
- Fukui M, Tanaka M, Shiraishi E, et al. Relationship between serum bilirubin and albuminuria in patients with type 2 diabetes. Kidney Int 2008;74:1197-201. [Crossref] [PubMed]
- Schwertner HA, Vítek L. Gilbert syndrome, UGT1A1*28 allele, and cardiovascular disease risk: possible protective effects and therapeutic applications of bilirubin. Atherosclerosis 2008;198:1-11. [Crossref] [PubMed]
- Ko GT, Chan JC, Woo J, et al. Serum bilirubin and cardiovascular risk factors in a Chinese population. J Cardiovasc Risk 1996;3:459-63. [Crossref] [PubMed]
- Horsfall LJ, Nazareth I, Petersen I. Cardiovascular events as a function of serum bilirubin levels in a large, statin-treated cohort. Circulation 2012;126:2556-64. [Crossref] [PubMed]
- Lin JP, O'Donnell CJ, Schwaiger JP, et al. Association between the UGT1A1*28 allele, bilirubin levels, and coronary heart disease in the Framingham Heart Study. Circulation 2006;114:1476-81. [Crossref] [PubMed]
- Han SS, Na KY, Chae DW, et al. High serum bilirubin is associated with the reduced risk of diabetes mellitus and diabetic nephropathy. Tohoku J Exp Med 2010;221:133-40. [Crossref] [PubMed]
- Jung CH, Lee MJ, Kang YM, et al. Higher serum bilirubin level as a protective factor for the development of diabetes in healthy Korean men: a 4 year retrospective longitudinal study. Metabolism 2014;63:87-93. [Crossref] [PubMed]
- Abraham NG, Asija A, Drummond G, et al. Heme oxygenase-1 gene therapy: recent advances and therapeutic applications. Curr Gene Ther 2007;7:89-108. [Crossref] [PubMed]
- Baranano DE, Rao M, Ferris CD, et al. Biliverdin reductase: a major physiologic cytoprotectant. Proc Natl Acad Sci U S A 2002;99:16093-8. [Crossref] [PubMed]
- Duann P, Lianos EA. GEC-targeted HO-1 expression reduces proteinuria in glomerular immune injury. Am J Physiol Renal Physiol 2009;297:F629-38. [Crossref] [PubMed]
- Stocker R, Yamamoto Y, McDonagh AF, et al. Bilirubin is an antioxidant of possible physiological importance. Science 1987;235:1043-6. [Crossref] [PubMed]
- Chen YH, Chau LY, Chen JW, et al. Serum bilirubin and ferritin levels link heme oxygenase-1 gene promoter polymorphism and susceptibility to coronary artery disease in diabetic patients. Diabetes Care 2008;31:1615-20. [Crossref] [PubMed]
- Kawamura K, Ishikawa K, Wada Y, et al. Bilirubin from heme oxygenase-1 attenuates vascular endothelial activation and dysfunction. Arterioscler Thromb Vasc Biol 2005;25:155-60. [Crossref] [PubMed]
- Rodella L, Lamon BD, Rezzani R, et al. Carbon monoxide and biliverdin prevent endothelial cell sloughing in rats with type I diabetes. Free Radic Biol Med 2006;40:2198-205. [Crossref] [PubMed]
- Ikeda N, Inoguchi T, Sonoda N, et al. Biliverdin protects against the deterioration of glucose tolerance in db/db mice. Diabetologia 2011;54:2183-91. [Crossref] [PubMed]
- Kalousová M, Novotny L, Zima T, et al. Decreased levels of advanced glycation end-products in patients with Gilbert syndrome. Cell Mol Biol (Noisy-le-grand) 2005;51:387-92. [PubMed]
- Vitek L, Malikova I, Kvasnicka J, et al. Relationship between serum bilirubin and markers of inflammation and oxidative stress. J Gastroenterol Hepatol 2007;22:A235.
- Sedlak TW, Saleh M, Higginson DS, et al. Bilirubin and glutathione have complementary antioxidant and cytoprotective roles. Proc Natl Acad Sci U S A 2009;106:5171-6. [Crossref] [PubMed]
- Frei B, Stocker R, Ames BN. Antioxidant defenses and lipid peroxidation in human blood plasma. Proc Natl Acad Sci U S A 1988;85:9748-52. [Crossref] [PubMed]
- Haffner SM. American Diabetes Association. Dyslipidemia management in adults with diabetes. Diabetes Care 2004;27 Suppl 1:S68-71. [Crossref] [PubMed]
- Barrett-Connor E, Grundy SM, Holdbrook MJ. Plasma lipids and diabetes mellitus in an adult community. Am J Epidemiol 1982;115:657-63. [Crossref] [PubMed]
- Seyoum B, Abdulkadir J, Berhanu P, et al. Analysis of serum lipids and lipoproteins in Ethiopian diabetic patients. Ethiop Med J 2003;41:1-8. [PubMed]
- Colwell JA, Nesto RW. The platelet in diabetes: focus on prevention of ischemic events. Diabetes Care 2003;26:2181-8. [Crossref] [PubMed]


