Non-operative treatment options for knee osteoarthritis
Introduction
Knee osteoarthritis (OA) is a chronic degenerative condition which leads to pain stiffness, and disability and affects almost one-fifth of the American population over the age of 45 years (1). Increased age and body mass index (BMI) are directly correlated with the prevalence of knee OA (2). Obesity is prevalent in approximately 66% of individuals with OA and many patients will report that joint pain prevents them from exercising and losing weight (3). Total knee arthroplasty (TKA) is indicated for advanced OA non-responsive to non-operative treatment, but not all patients are surgical candidates and some prefer not to have surgery. Furthermore, while TKA is a high-successful procedure, patients can still experience post-operative complications (4).
For mild to moderate OA, patients are managed conservatively with one or more non-operative treatment modalities for which there are a wide range of options with varying efficacy. The American Academy of Orthopedic Surgeons (AAOS) recommends strengthening exercises, low impact aerobic exercises, aquatic exercises, weight loss programs, and nonsteroidal anti-inflammatory agents (NSAIDs) (5). However, they did not reach a consensus determination regarding knee bracing, intra-articular corticosteroid injections, or hyaluronate injections due to varying results in the literature.
In order to best provide for our knee OA patients, it is essential for practitioners to understand the risks and benefits of the available treatments for successful management. Therefore, the purpose of this study was to review the non-operative management options for knee OA. Specifically, we evaluated: (I) NSAIDs; (II) weight loss; (III) intra-articular injections; (IV) physical therapy; and (V) bracing.
Methods
A comprehensive literature review was conducted using the electronic databases PubMed and EBSCO Host. All available studies between January 1, 1995 and December 31, 2018 were evaluated. Searches were performed using the following terms: total knee arthroplasty (title), cyclooxygenase-2 inhibitors (title), bracing (title), physical therapy (title), weight loss (title), knee osteoarthritis (title), intra-articular injection (title), hyaluronic acid (title), corticosteroid (title), and alternative (title). It is possible that some studies evaluating the above topics were not included for final analysis, however, for each field, a variety of the current literature is presented to provide at least an overview.
Reports were included if they evaluated clinical post-operative outcomes following TKA, had full-texts available, and were written in the English language. Exclusion criteria were the following: basic science studies, cadaveric studies, animal studies, conference abstracts, conference reviews, editorials, letters to the editor, surveys, case reports, and case series.
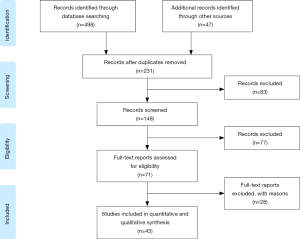
An initial literature search was performed by two authors (M DeRogatis, N Sodhi). Abstracts were screened in order to determine if identified articles met the inclusion and exclusion criteria. The full-text of selected articles was then further evaluated. The list of search results was screened for repeat reports by a third author (HK Anis). The references of all included studies were reviewed and determined for eligibility. The initial search yielded 7,882 reports. Through a Title and Abstract review, we identified relevant manuscripts, which were subsequently recovered in full and studied, yielding 545 reports that satisfied the search criteria. After full-text analysis, 43 studies were included in this review (Figure 1).
Results
Nonsteroidal anti-inflammatory drugs
In the past two decades, numerous studies have described the use of NSAIDs for knee OA (6-13). Many of these studies have demonstrated that NSAIDs are relatively safe and effective options to reduce pain and to improve function with long-term use. In a large meta-analysis, Puljak et al. (7) reviewed 15,337 patients who had a mean duration of OA for 8 years who were treated with celecoxib or a placebo. At an average of 6 months, there was a 12% improvement in the WOMAC pain and function scales without any serious adverse events (Table 1). Similarly, Bjordal et al. (8) reviewed 10,845 knee OA patients from 23 trials comparing NSAIDs (72%) to a placebo (28%). The mean duration of symptoms prior to intervention was 8 years. At a mean follow up of 13 weeks, VAS pain scores significantly improved by 16% and functional disability was decreased with NSAIDs (P<0.05) without any serious events. Additionally, a 6-month multi-center, randomized, double blind trial compared the efficacy of celecoxib (50%) and naproxen (50%) and found Western Ontario and McMasters Universities (WOMAC) pain, stiffness, and function scores improved in both groups (12). One patient developed atrial fibrillation and another patient suffered anaphylaxis in the celecoxib group. One patient in the naproxen group developed a serious adverse event of thrombocytopenia.
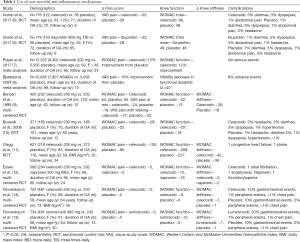
Full table
Conversely, Gordo et al. (6) retrospectively reviewed 301 knee OA patients treated with ibuprofen, celecoxib, or placebo over 6 weeks. Compared to the placebo groups, VAS pain and total WOMAC scores (measuring pain, stiffness, and function) were not significantly decreased in the treatment groups. Limitations of this study include a small sample size and the possibility of prior chronic use of NSAIDs. There is also literature to suggest that long-term NSAID use lead to renal, gastrointestinal, and cardiovascular adverse effects.
NSAIDs are most effective when used continuously, however, many patients will use them only when they have pain resulting in potentially less than optimal outcomes. They may be used in conjunction with other forms of treatment for knee OA as they have been shown to provide some pain relief as well as functional improvements.
Weight loss
Obesity is a modifiable risk factor for knee OA. It has been shown to improve pain, function, and stiffness with no adverse effects (14-21). There are multiple studies evaluating low energy diets, exercise, or both for the treatment of knee OA. Foy et al. (19) studied 2,203 obese diabetic patients with symptomatic knee OA and a mean BMI of 37 kg/m2 who were randomized into either weight stable (n=1,095) or weight loss (n=1,108) groups for 1 year. Participants in the weight loss group lost 9 kg and reported significantly better WOMAC pain, function, and stiffness scores compared to those in the weight stable group (P<0.05) (Table 2). Edwards et al. (21) studied 24 patients who had a mean BMI of 42 and radiographic evidence of knee OA who underwent bariatric surgery. At one-year follow-up, the average reduction in BMI was 13 kg/m2 and WOMAC pain, function, and stiffness scores significantly improved when compared to baseline (P<0.05).
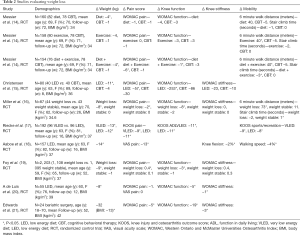
Full table
Similarly, Messier et al. (14) studied 316 obese participants with radiographic evidence of knee OA over 18 months. Participants were randomized into lifestyle changes, diet only, exercise only, or diet plus exercise cohorts. Participants treated with diet plus exercise showed a significant decrease in weight, WOMAC pain and function scores, 6-minute walk distance, and stair climb time compared to a healthy lifestyle control group (P<0.05). Miller and colleagues studied 87 obese individuals randomized to a low energy diet or no diet (16). Participants in the low energy diet lost 8 kg and had significant improvements in WOMAC pain and function scores, along with improvements in 6-minute walk distance and stair climb time when compared to control diets (P<0.05).
Based on the above studies, weight loss is a promising modality for the treatment of knee OA. It is a safe and effective way to improve knee pain, function, and stiffness without serious adverse effects. However, weight loss can be very challenging for obese patients with knee OA due to their limited mobility and lack of adherence to a low-calorie diet. Patients should be educated on alternative methods such as low-calorie diets, medications, and bariatric surgery.
Intra-articular injections
Intra-articular injections for knee OA have been in use for many years, but their efficacy have been questionable in the current literature (22-30). Some patients will experience minimal pain relief, while others have substantial relief for months. Despite inconclusive outcomes, there has been an increasing prevalence in the use of intra-articular injections to treat knee OA often with the aim to postpone a TKA. Corticosteroid and hyaluronic acid (HA) injections are the two main types of intraarticular injections. Corticosteroids take 24 to 48 hours to provide relief and may be repeated every 3 months (24). Patients with uncontrolled diabetes are not good candidates for corticosteroid injections due to the acute rise in serum glucose. HA is a naturally occurring substance in synovial fluid and acts as a shock absorber for the knee, but is decreased in arthritic knees (31). Treatment with HA injections may be repeated every 3 months and can come in a series of three to five injections administered weekly or by a single injection (24).
Jüni and colleagues retrospectively reviewed 27 trials including a total of 1,749 patients treated with either corticosteroid or placebo injections (22). Overall, corticosteroid injections showed significant improvements in pain and function when compared to placebo (P<0.05). The greatest benefits were noticed at 1 to 2 weeks followed by 4 to 6 weeks post-treatment. However, no benefits were noticed at 26 weeks after injection (P>0.05) (Table 3).
Full table
Askari et al. retrospectively reviewed 69 patients treated with corticosteroid injections and 71 patients treated with HA injections (24). There was no difference in pain or stiffness after 3 months in either group (P>0.05), but there was a significant improvement in WOMAC function scores at 3 months (P<0.05). Unlike corticosteroid injections, there was a significant decrease in the VAS pain score with HA at 3 months. Both groups showed a significant decrease in pain at one and two months follow-up (P<0.05). Campos and colleagues prospectively studied the addition of corticosteroid to HA injections versus HA alone in 90 Kellgren-Lawrence stage 3 knees (29). At 4 weeks, VAS pain scores improved by 49% (P<0.05) and WOMAC function scores improved by 43% in patients who received corticosteroid plus HA. There was also significant improvement in pain and function with HA injections. The addition of corticosteroid was superior to HA injections alone for all scores (P<0.05).
The use of corticosteroid injections may be of benefit in the short term, especially when combined with HA. Injections proved to be safe without any reported short term adverse events in the cited studies, however, the long term effects of intraarticular injections remain uncertain.
Physical therapy
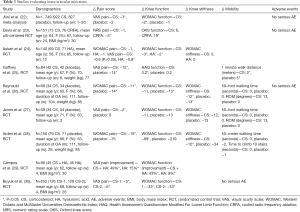
Muscle strengthening exercises have led to improved pain and functional outcomes in knee OA patients (32-35). Silva et al. (32) randomized 64 patients with knee OA into land or water-based physical therapy cohorts and at 3 months follow-up, both groups reported a reduction in pain (P<0.05). Knee function was only improved in patients treated with hydrotherapy (water-based physical therapy) at final follow up, but improvements in both groups were observed at 9 weeks (P<0.05) (Table 4). Similarly, Foley et al. (33) randomized 105 patients to be treated with hydrotherapy, gym strengthening exercises, or no therapy and also noted a reduction of pain with hydrotherapy at 6 weeks (P<0.05). A randomized controlled trial including 102 patients with knee OA treated with high-resistance exercise, low-resistance exercise, or no exercise for 8 weeks found that both high-resistance and low-resistance exercises improved knee pain and function when compared to baseline (P<0.05), however, there was no difference between the groups (35).

Full table
Physical therapy in the form hydrotherapy, resistance training, or land-based exercises led to significant improvements in pain and function without any adverse effects. This is another form of a non-pharmacological intervention that is safe and highly effective. Decreased compliance rates of physical therapy are thought to be the result of high copayments, pain with activity, lack of transportation, and time commitment. Therefore, cost issues are a major barrier for usage. Physical therapy programs are varied and therefore patients and physicians should discuss these in order to improve compliance.
Braces
Knee braces are frequently used for knee OA and the American Academy Orthopaedic Surgeons recommends bracing for biomechanical stability (5). Knee malalignment associated with OA can cause significant pain and dysfunction and knee braces have shown to help with stability and function, especially in unicompartmental arthritis (36-42). There are two types of braces that are commonly used for knee OA, an unloader brace and a support brace. An unloader brace relieves pressure from the affected compartment and a support brace provides compression.
Yu et al. (37) prospectively studied 204 osteoarthritic knees treated with an unloader brace (n=86), patellofemoral brace (n=50), or no brace (n=68). At 26 weeks there was a significant improvement with bracing compared to no bracing (P<0.05). At 1-year follow-up, pain, activities of daily living (ADLs), 6-minute walk test, and timed up and go (TUG) test were significantly improved in all groups compared to baseline, however, no significant differences were noted between the brace and no brace groups. (Table 5).

Full table
Kirkley and colleagues performed a randomized controlled trial comparing unloader braces and neoprene sleeves to a control group (38). Significant differences in pain after the 6-minute walk test and 30-second stair-climbing test were reported with the unloader brace when compared to neoprene brace at 6 months (P<0.05). When comparing braced to unbraced patients, there were significant differences in WOMAC function scores (P<0.05).
Chughtai et al. (40) randomized 36 patients with Kellgren-Lawrence grades 3 to 4 knee OA to receive either a pneumatic unloader brace with conventional treatment or just conventional treatment. At a follow-up of one year, there were significantly fewer patients who received injections (46% vs. 83%, P<0.05) and less subsequent TKAs in the brace group (18% vs. 36%, P<0.05).
Imoto et al. (43) 100 patients who were randomized to either NMES bracing or control and were evaluated based on a numerical pain scale from 0 to 10, timed up and go (TUG) test, Lequesne index and activities of daily living (ADL) scale. The authors found the NMES cohort to have a statistically significant improvement regarding pain intensity [difference between means: 1.67 (0.31 to 3.02); P=0.01]; Lequesne index [difference between means: 1.98 (0.15 to 3.79); P=0.03]; and ADL scale [difference between means: −11.23 (−19.88 to −2.57); P =0.01] compared to the control cohort. In a smaller case series, Stevens et al. (44) also found 80% of patients treated with NMES and exercise to have greater increases in quadriceps strength compared to the contralateral leg treated with exercise only. Cherian et al. (45) also evaluated a prospective case-control cohort, and found NMES to help improve quadriceps strength and potentially improve knee functionality in knee OA patients. Other studies have also reported a number of other patient-specific and financial advantages to NMES (46,47).
Based on these data, braces help knee OA patients achieve marked improvements in pain, function, and may prolong their time to a TKA. This is a non-pharmacological treatment option that can improve symptoms and limit the use of other treatment modalities which are associated with greater risks.
Conclusions
Knee OA is a chronic condition that is often challenging to treat for clinicians and confers a substantial burden for affected patients. For clinicians, it is crucial to understand patient goals, insurance coverage, financial status, comorbidities, severity of OA, and the efficacy of treatment options to determine what is most beneficial for the patient. NSAIDs, weight loss, intraarticular injections, and physical therapy have all been shown to be effective non-surgical treatment options for knee OA. Bracing for knee OA is a noninvasive, nonpharmacologic option that can significantly reduce pain and improve function without any adverse effects. Therefore, based on this literature review, knee braces, in combination with other non-operative modalities, should be one mainstay of treatment in conjunction with other treatment modalities to reduce pain, improve function, stiffness, and mobility in knee OA.
Acknowledgments
None.
Footnote
Conflicts of Interest: MA Mont: AAOS, Cymedica, DJ Orthopaedics, Johnson & Johnson, Journal of Arthroplasty, Journal of Knee Surgery, Microport, National Institutes of Health (NIAMS & NICHD), Ongoing Care Solutions, Orthopedics, Orthosensor, Pacira, Peerwell, Performance Dynamics Inc, Sage, Stryker: IP royalties, Surgical Technologies International, Kolon TissueGene. A Bhave: Cymedica, DJ Orthopaedics, Guardian Inc, On Going Care, Journal of Society of Indian Physiotherapists. M Chughtai: DJ Orthopaedics, Sage Products, Stryker, Peerwell, Reflexion, Astym: Pain consultant. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Lawrence RC, Felson DT, Helmick CG, et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States: Part II. Arthritis Rheum 2008;58:26-35. [Crossref] [PubMed]
- Felson DT, Lawrence RC, Dieppe PA, et al. Osteoarthritis: new insights. Part 1: the disease and its risk factors. Ann Intern Med 2000;133:635-46. [Crossref] [PubMed]
- Shih M, Hootman JM, Kruger J, et al. Physical Activity in Men and Women with Arthritis. Am J Prev Med 2006;30:385-93. [Crossref] [PubMed]
- Sodhi N, Piuzzi NS, Dalton SE, et al. What Influence Does the Time of Year Have on Postoperative Complications Following Total Knee Arthroplasty? J Arthroplasty 2018;33:1908-13. [Crossref] [PubMed]
- AAOS. Treatment of Osteoarthritis of the Knee, 2nd edition summary of recommendations.
- Gordo AC, Walker C, Armada B, et al. Efficacy of celecoxib versus ibuprofen for the treatment of patients with osteoarthritis of the knee: A randomized double-blind, non-inferiority trial. J Int Med Res 2017;45:59-74. [Crossref] [PubMed]
- Puljak L, Marin A, Vrdoljak D, et al. Celecoxib for osteoarthritis. Cochrane Database Syst Rev 2017;5:CD009865. [PubMed]
- Bjordal JM, Ljunggren AE, Klovning A, et al. Non-steroidal anti-inflammatory drugs, including cyclo-oxygenase-2 inhibitors, in osteoarthritic knee pain: meta-analysis of randomised placebo controlled trials. BMJ 2004;329:1317. [Crossref] [PubMed]
- Bensen WG, Fiechtner JJ, McMillen JI, et al. Treatment of Osteoarthritis With Celecoxib, a Cyclooxygenase-2 Inhibitor: A Randomized Controlled Trial. Mayo Clin Proc 1999;74:1095-105. [Crossref] [PubMed]
- Boswell DJ, Ostergaard K, Philipson RS, et al. Evaluation of GW406381 for treatment of osteoarthritis of the knee: two randomized, controlled studies. Medscape J Med 2008;10:259. [PubMed]
- Clegg R, Harris DJ, Clegg DO, et al. Publication Date Glucosamine, Chondroitin Sulfate, and the Two in Combination for Painful Knee Osteoarthritis. N Engl J Med 2006.354.
- Essex MN, Bhadra P, Sands GH. Efficacy and Tolerability of Celecoxib versus Naproxen in Patients with Osteoarthritis of the Knee: a Randomized, Double-blind, Double-dummy Trial. J Int Med Res 2012;40:1357-70. [Crossref] [PubMed]
- Tannenbaum H, Berenbaum F, Reginster JY, et al. Lumiracoxib is effective in the treatment of osteoarthritis of the knee: a 13 week, randomised, double blind study versus placebo and celecoxib. Ann Rheum Dis 2004;63:1419-26. [Crossref] [PubMed]
- Messier SP, Loeser RF, Miller GD, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: The arthritis, diet, and activity promotion trial. Arthritis Rheum 2004;50:1501-10. [Crossref] [PubMed]
- Christensen R, Astrup A, Bliddal H. Weight loss: the treatment of choice for knee osteoarthritis? A randomized trial. Osteoarthr Cartil 2005;13:20-7. [Crossref] [PubMed]
- Miller GD, Nicklas BJ, Davis C, et al. Intensive Weight Loss Program Improves Physical Function in Older Obese Adults with Knee Osteoarthritis*. Obesity 2006;14:1219-30. [Crossref] [PubMed]
- Riecke BF, Christensen R, Christensen P, et al. Comparing two low-energy diets for the treatment of knee osteoarthritis symptoms in obese patients: a pragmatic randomized clinical trial. Osteoarthr Cartil 2010;18:746-54. [Crossref] [PubMed]
- Aaboe J, Bliddal H, Messier SP, et al. Effects of an intensive weight loss program on knee joint loading in obese adults with knee osteoarthritis. Osteoarthr Cartil 2011;19:822-8. [Crossref] [PubMed]
- Foy CG, Lewis CE, Hairston KG, et al. Intensive Lifestyle Intervention Improves Physical Function Among Obese Adults With Knee Pain: Findings From the Look AHEAD Trial. Obesity 2011;19:83-93. [Crossref] [PubMed]
- A de Luis D, Izaola O, García Alonso M, et al. Effect of a hypocaloric diet with a commertial formula in weight loss and quality of life in obese patients with chronic osteoarthritis. Nutr Hosp 2012;27:1648-54.
- Edwards C, Rogers A, Lynch S, et al. The Effects of Bariatric Surgery Weight Loss on Knee Pain in Patients with Osteoarthritis of the Knee. Arthritis 2012;2012:504189. [PubMed]
- Jüni P, Hari R, Rutjes AW, et al. Intra-articular corticosteroid for knee osteoarthritis. Cochrane Database Syst Rev 2015.CD005328. [PubMed]
- Davis T, Loudermilk E, DePalma M, et al. Prospective, Multicenter, Randomized, Crossover Clinical Trial Comparing the Safety and Effectiveness of Cooled Radiofrequency Ablation With Corticosteroid Injection in the Management of Knee Pain From Osteoarthritis. Reg Anesth Pain Med 2018;43:84-91. [Crossref] [PubMed]
- Askari A, Gholami T. Hyaluronic acid compared with corticosteroid injections for the treatment of osteoarthritis of the knee: a randomized control trail. Springerplus 2016;5:442. [Crossref] [PubMed]
- Gaffney K, Ledingham J, Perry JD. Intra-articular triamcinolone hexacetonide in knee osteoarthritis: factors influencing the clinical response. Ann Rheum Dis 1995;54:379-81. [Crossref] [PubMed]
- Raynauld JP, Buckland-Wright C, Ward R, et al. Safety and efficacy of long-term intraarticular steroid injections in osteoarthritis of the knee: A randomized, double-blind, placebo-controlled trial. Arthritis Rheum 2003;48:370-7. [Crossref] [PubMed]
- Jones A, Doherty M. Intra-articular corticosteroids are effective in osteoarthritis but there are no clinical predictors of response. Ann Rheum Dis 1996;55:829-32. [Crossref] [PubMed]
- Arden NK, Reading IC, Jordan KM, et al. A randomised controlled trial of tidal irrigation vs corticosteroid injection in knee osteoarthritis: the KIVIS Study. Osteoarthr Cartil 2008;16:733-9. [Crossref] [PubMed]
- Campos G. 511 evaluation of the effect of adding corticosteroid to viscosupplementation: a prospective and randomized study. 2011.
- Buyuk AF, Kilinc E, Camurcu IY, et al. Compared efficacy of intra-articular injection of methylprednisolone and triamcinolone. Acta Ortop Bras 2017;25:206-8. [Crossref] [PubMed]
- .Viscosupplementation Treatment for Knee Arthritis - OrthoInfo - AAOS.
- Silva LE, Valim V, Pessanha APC, et al. Hydrotherapy Versus Conventional Land-Based Exercise for the Management of Patients With Osteoarthritis of the Knee: A Randomized Clinical Trial. Phys Ther 2008;88:12-21. [Crossref] [PubMed]
- Foley A, Halbert J, Hewitt T, et al. Does hydrotherapy improve strength and physical function in patients with osteoarthritis-a randomised controlled trial comparing a gym based and a hydrotherapy based strengthening programme. Ann Rheum Dis 2003;62:1162-7. [Crossref] [PubMed]
- Deyle GD, Henderson NE, Matekel RL, et al. Effectiveness of Manual Physical Therapy and Exercise in Osteoarthritis of the Knee. Ann Intern Med 2000;132:173. [Crossref] [PubMed]
- Jan MH, Lin JJ, Liau JJ, et al. Investigation of Clinical Effects of High- and Low-Resistance Training for Patients With Knee Osteoarthritis: A Randomized Controlled Trial. Phys Ther 2008;88:427-36. [Crossref] [PubMed]
- Brouwer RW, van Raaij TM, Verhaar JAN, et al. Brace treatment for osteoarthritis of the knee: a prospective randomized multi-centre trial. Osteoarthr Cartil 2006;14:777-83. [Crossref] [PubMed]
- Yu SP, Williams M, Eyles JP, et al. Effectiveness of knee bracing in osteoarthritis: pragmatic trial in a multidisciplinary clinic. Int J Rheum Dis 2016;19:279-86. [Crossref] [PubMed]
- Kirkley A, Webster-Bogaert S, Litchfield R, et al. The effect of bracing on varus gonarthrosis. J Bone Joint Surg Am 1999;81:539-48. [Crossref] [PubMed]
- Larsen BL, Jacofsky MC, Brown JA, et al. Valgus bracing affords short-term treatment solution across walking and sit-to-stand activities. J Arthroplasty 2013;28:792-7. [Crossref] [PubMed]
- Chughtai M, Bhave A, Khan SZ, et al. Clinical Outcomes of a Pneumatic Unloader Brace for Kellgren-Lawrence Grades 3 to 4 Osteoarthritis: A Minimum 1-Year Follow-Up Study. J Knee Surg 2016;29:634-8. [Crossref] [PubMed]
- Duivenvoorden T, Brouwer RW, van Raaij TM, et al. Braces and orthoses for treating osteoarthritis of the knee. Cochrane Database Syst Rev 2015.CD004020. [PubMed]
- Sattari S, Ashraf AR. Comparison the effect of 3 point valgus stress knee support and lateral wedge insoles in medial compartment knee osteoarthritis. Iran Red Crescent Med J 2011;13:624-8. [Crossref] [PubMed]
- Imoto AM, Peccin MS, Teixeira LEP de P, et al. Is neuromuscular electrical stimulation effective for improving pain, function and activities of daily living of knee osteoarthritis patients? A randomized clinical trial. Sao Paulo Med J 2013;131:80-7. [Crossref] [PubMed]
- Stevens JE, Mizner RL, Snyder-Mackler L. Neuromuscular electrical stimulation for quadriceps muscle strengthening after bilateral total knee arthroplasty: a case series. J Orthop Sports Phys Ther 2004;34:21-9. [Crossref] [PubMed]
- Cherian JJ, McElroy MJ, Kapadia BH, et al. Prospective Case Series of NMES for Quadriceps Weakness and Decrease Function in Patients with Osteoarthritis of the Knee. J Long Term Eff Med Implants 2015;25:301-6. [Crossref] [PubMed]
- Chughtai M, Piuzzi N, Yakubek G, et al. Use of an App-Controlled Neuromuscular Electrical Stimulation System for Improved Self-Management of Knee Conditions and Reduced Costs. Surg Technol Int 2017;31:221-6. [PubMed]
- Pal S, Chughtai M, Sultan AA, et al. Impact of Neuromuscular Electrical Stimulation (NMES) on 90-Day Episode Costs and Post-Acute Care Utilization in Total Knee Replacement Patients with Disuse Atrophy. Surg Technol Int 2017;31:384-8. [PubMed]
- Brouwer RW, van Raaij TM, Jakma TTSC, et al. Braces and orthoses for treating osteoarthritis of the knee. In: Brouwer RW. editor. Cochrane Database of Systematic Reviews. Chichester, UK: John Wiley & Sons, Ltd, 2005:CD004020.