
The role of acute kidney injury duration in clinical practice
Acute kidney injury (AKI) can be caused by various factors such as toxins, ischemia, sepsis, obstructive uropathy, and others. Currently, there are two main classification systems that are used for determination of AKI severity in clinical practice, and these are the Risk/Injury/Failure/Loss/End-stage (RIFLE) criteria and Acute Kidney Injury Network (AKIN) criteria. Both have implemented the rise of creatinine level and decreased in urine output as two major factors in determining the severity of AKI and act as a guide to start renal replacement therapy (RRT). However, none of the classification systems have implicated AKI duration as another dimension for defining the true severity of kidney dysfunction.
It is known that a short-term AKI diagnosis has a better clinical outcome when compared with a patient with persistent AKI. In clinical practice, modern physicians are still facing the challenges to care for patients with AKI because the course of AKI is unpredictable. Some patients with AKI will eventually progress to end-stage renal disease and others will fully or partially recover. Any preexisting co-morbidities and intrinsic kidney health status will directly affect the kidney outcomes after the stress or inciting factors are removed. For example, a patient who experienced severe diarrhea that provoked a profound kidney dysfunction by renal hypoperfusion can be hindered from dialysis if deficit volume is replenished as early as possible after the AKI episode. However, the recovery of renal function in a patient with chronic kidney disease (CKD) who experienced dehydration related to AKI might be delayed or even needed long-term RRT due to non-recovery of kidney function. The maladaptive response to kidney injury in established CKD patients will bring significant mortality and morbidity. The recovery of AKI becomes a crucial entity because a patient with short term AKI has a better clinical outcome when compared with a patient with persistent AKI.
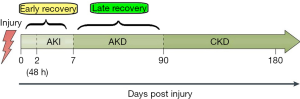
The distinction between short term AKI and persistent AKI is not delineated across several studies. Lately, a consensus report from the Acute Disease Quality Initiative Workgroup has defined transient AKI with a duration of 48 h, and persistent AKI that continues beyond 48 h. They also applied a new term for AKI that lasted between 7 and 90 days as acute kidney disease (AKD) (1). Persistent AKI and AKD are a continuum and AKD can progress into CKD when AKD had progressed beyond 90 days. In their report, they have illustrated various possible scenarios of AKD occurrence to show the complexity of AKD development after AKI.
The objectives of the consensus report are to clarify the interplay between AKI, AKD, and CKD. They emphasized that increasing intensity of monitoring in a patient with AKD is important due to the susceptibility of AKD patients to kidney damage. Early nephrology referral and increased the frequency of kidney function measurements during follow up might be necessary for this particular stage of kidney disease. The timeline of AKI-AKD-CKD continuum also can represent our concept of AKI duration.
The duration of AKI is associated with renal recovery. In other words, a patient with transient AKI will have early renal recovery and a patient with persistent AKI is considered to have a late recovery of renal function. The capability of the damaged kidney to been recovered from injury, basically through self-repaired mechanism already became an area of interest (2). Forni et al. well illustrates the distinction between early recovery and late recovery of renal function in his article entitled “Renal recovery after acute kidney injury” (3). Figure 1 depicts the interrelations between AKI-AKD-CKD continuum and their respective recovery time course.
The recovery of renal function becomes an interesting topic for investigators to focus. As it is known that serum creatinine level is affected by muscle mass, age, sex, body size, drugs, and other factors. Thus, serum creatinine level has its limitations for being used as an indicator for early kidney damage or an indicator for renal recovery. This leads to a robust search for potentially useful biomarkers that can predict renal recovery and non-renal recovery. Inflammatory markers such as neutrophil gelatinase-associated lipocalin (NGAL), interleukin (IL)-6 and IL-18, cell injury biomarkers such as kidney injury molecule-1 (KIM-1) and liver fatty acid binding protein (L-FABP) and markers of cell cycle arrest, insulin growth factor binding protein 7 (IGFBP7) and tissue inhibitor of metalloproteinase 2 (TIMP-2) have been identified as potential biomarkers for the prediction of AKI progression in several studies. The study by Du et al. revealed the potential role of urine microRNA-21 as a prognostic biomarker of AKI progression after cardiac surgery (4). Shortly, discovering new biomarkers that have high prognostic value for renal recovery will have an impact on the clinical care for AKI patients. In precision medicine, those biomarkers that can reflect the etiologies of AKI is worth exploring in the future to prevent AKI or promotes renal recovery (5).
The work done by Truche et al. has shown that the duration of AKI is correlated with ICU mortality and the need for RRT in critically ill patients (6). Mehta et al. did a recent meta-analysis which also showed that AKI duration is independently associated with long-term mortality, cardiovascular events, and development of incidents in CKD stage 3 (7). Although both authors have advocated that the duration of AKI can be incorporated as another dimension for the assessment of AKI severity, they also pointed out that their studies have some limitations. They have elucidated that their study results can be biased by unknown confounders and the assessment of baseline creatinine level was not always available during the study. These might lead to an overestimation of AKI incidents and interpretations of the results will be a misguided.
The concept of AKI duration is overlapped with renal recovery. There is no doubt that a higher mortality and morbidity is associated with a non-recovery of kidney function. The biomarkers that were correlated with renal recovery may have important prognostic values with clinical survival rate. Different modalities of dialysis such as continuous RRT (CRRT) and intermittent hemodialysis (IHD) may have different outcomes on renal recovery (8). In a clinical practice, we recommended that CRRT to be a favorable modality for RRT in critically ill patients with unstable hemodynamics. This signified that different interventions or dialysis methods might affect the progression of AKI or shorten AKI duration.
In conclusion, in the real world, the cause of AKI may be multifactorial, a kidney biopsy may be needed in some circumstance if the diagnosis of the causes of AKI is in doubt or the AKD is in progression. The priority work and optimal management for a patient with acute renal function impairment are to prevent the disease from becoming chronic. Physicians in care should be alerted to non-renal recovery incidents in AKI patients. In other words, the duration of AKI should become an important deciding factor for the care of patients with AKI and especially in critically ill patients. A cause directed search for possible pathological insults should be initiated as soon as possible. Any diagnostic tools that assisted for the prediction of AKI progression or interventions that will enhance renal recovery should be implemented in daily clinical practice.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Disclaimer: The views expressed in this editorial do not necessarily represent the view of the Ministry of Health and Welfare, Taiwan.
References
- Chawla LS, Bellomo R, Bihorac A, et al. Acute kidney disease and renal recovery: consensus report of the Acute Disease Quality Initiative (ADQI) 16 Workgroup. Nat Rev Nephrol 2017;13:241-57. [Crossref] [PubMed]
- He L, Wei Q, Liu J, et al. AKI on CKD: heightened injury, suppressed repair, and the underlying mechanisms. Kidney Int 2017;92:1071-83. [Crossref] [PubMed]
- Forni LG, Darmon M, Ostermann M, et al. Renal recovery after acute kidney injury. Intensive Care Med 2017;43:855-66. [Crossref] [PubMed]
- Du J, Cao X, Zou L, et al. MicroRNA-21 and risk of severe acute kidney injury and poor outcomes after adult cardiac surgery. PLoS One 2013;8:e63390. [Crossref] [PubMed]
- Kiryluk K, Bomback AS, Cheng YL, et al. Precision Medicine for Acute Kidney Injury (AKI): Redefining AKI by Agnostic Kidney Tissue Interrogation and Genetics. Semin Nephrol 2018;38:40-51. [Crossref] [PubMed]
- Truche AS, Ragey SP, Souweine B, et al. ICU survival and need of renal replacement therapy with respect to AKI duration in critically ill patients. Ann Intensive Care 2018;8:127. [Crossref] [PubMed]
- Mehta S, Chauhan K, Patel A, et al. The prognostic importance of duration of AKI: a systematic review and meta-analysis. BMC Nephrol 2018;19:91. [Crossref] [PubMed]
- Schneider AG, Bagshaw SM. Effects of renal replacement therapy on renal recovery after acute kidney injury. Nephron Clin Pract 2014;127:35-41. [Crossref] [PubMed]


