
Clinical outcomes after absorbable suture fixation of patellar osteochondral fracture following patellar dislocation
Introduction
Patellar dislocation is a common sports injury of the knee in adolescents (1). During the dislocation and reduction process, the medial facet of the patella shears with the lateral femoral condyle, which often results in patellar or lateral femoral condylar osteochondral fractures (OCFs) (2,3). The incidence of OCF following a patellar dislocation varies from 5% to 54% (4,5). Implants have been introduced to achieve a fixation of the lateral condylar OCF, including headless screws or bioabsorbable pins (6-9). However, as compared with the satisfactory outcomes of the lateral condylar OCF fixation, previously reported prognoses of the patellar OCF fixation were much poorer by the same fixation methods, due to the insufficient fixation reliability and higher operation difficulty, with it relying on the limited thickness of the patella.
Suture fixation of patellar OCFs after patellar dislocation has been reported since 1995 (10), but little is known about the mid-term or long-term outcomes of this suture fixation for OCFs of the patella. This study aimed to review the mid-term clinical outcomes of patients who have undergone absorbable suture fixation of patellar OCFs.
Methods
All patients who had received surgical fixation for OCFs were reviewed between January 2011 and December 2015. The institutional review board approved this study, and the informed consent was signed and obtained from each patient. The baseline information was collected from the medical record database retrospectively, while the identification of each patient had been removed during the study. The inclusion criteria of this study were (I) diagnosis of patellar dislocation (primary or recurrent), (II) history of acute injury less than four weeks before surgery, and (III) the existence of patellar OCFs confirmed by MRI and arthroscopy. Exclusion criteria were (I) the existence of other locations of OCFs confirmed by MRI and arthroscopy, and (II) a history of knee surgeries.
Each patient had knee anteroposterior view and lateral view X-ray, CT, and MRI exams performed preoperatively. The same surgeon and his group performed all surgeries.
Surgical techniques
Before other procedures, a knee arthroscopy was carried out for the diagnosis of the intra-articular injury, the size and location of the OCF were confirmed. The surgeon attentively evaluated whether the fracture fragment was fresh or not. While the rim of fragment stayed sharp and the donor surface of the patella was fresh; then the suture fixation procedure was performed.
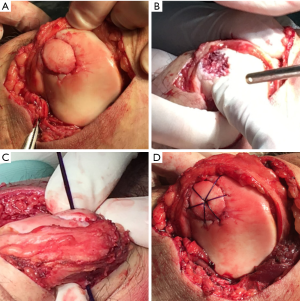
A medial parapatellar incision was made to identify the fracture fragment, and it was then reduced to the main body of the patella. A 2.0 mm Kirschner wire was drilled through the middle of the fragment. Six holes were then similarly made by 1.0 mm Kirschner wire around the fracture fragments, and each location was optimally selected. The distances between the holes and fracture edges were 2.0 mm. The PDS suture (Ethicon Inc., NJ, US) penetrated into the holes by spinal needle, and was then fixed and knotted in the back of the patella (Figure 1). The joint capsule and the medial retinaculum were repaired with appropriate tension.
The medial patellofemoral ligament (MPFL) was repaired or reconstructed if necessary. For the primary dislocation of the patella, the MPFL repair was available. Sutures were placed into the MPFL to overlap the tissue medially. The lateral translation was evaluated during passive flexion of the knee to 90°, and then the sutures were tied in place. Otherwise, for the recurrent patellar dislocation with MPFL lesions, the semitendinosus tendon was harvested for double-stranded anatomic MPFL reconstruction. On the medial patella side, the graft was fixed into a sulcus and two suture anchors (Smith&Nephew, 5.0 mm, US) on the upper half of the medial bone surface. On the femoral side, the graft was fixed with a bone tunnel and an interface screw (Smith&Nephew, 5.0/6.0 mm, US).
Rehabilitation
After fracture fixation and MPFL repair or reconstruction, patients were asked to wear a knee brace during the first 6 weeks after surgery, and 30 degree extension exercise was permitted for the first 4 weeks. For the next 2 weeks and before 6 weeks postoperatively, 90 degree extension exercise was allowed. Partial weight bearing was permitted after surgery and full weight bearing was allowed until 6 weeks postoperatively. Strengthening exercise began at 3 months. No sports activities were permitted before 6 months postoperatively.
Evaluation and statistical analysis
The patients were followed up at 6 weeks, 3, 6 months and then once every year postoperatively. Evaluation criteria included the satisfaction degree of patients with the surgery and postoperative daily activities, and recurrence of dislocation. Functional assessment of Lysholm and Kujala knee function score was performed at the latest follow-up. Regular X-ray and 3-Tesla MRI imaging were taken during the follow-up to evaluate the fracture healing. For all statistical analysis, the paired sample t-test was performed using the software SPSS 19.0.
Results
Between January 2011 and December 2015, 18 patients met the inclusion criteria, including 2 males and 16 females. The average age of the patients was 18.6 years, ranging from 13 to 32 years. The mean follow-up period of all patients was 36 months (12 to 58, SD =36 months). The duration from the latest patellar dislocation to the surgery operation ranged from 5 to 10 days, for an average of 8 days. During the operation, cartilage defects were all found in the medial facet of the patella, and the sizes of the OCFs were measured. In this group, the mean length was 20 mm (SD =5 mm; range, 10–30), and the mean width was 16 mm (SD =4 mm; range, 10–25).
During the intraoperative examination, 4 of the 18 patients had a primary dislocation, and these patients had the MPFL repaired. The 14 patients with a recurrent dislocation, underwent double-stranded anatomic MPFL reconstruction by autologous semitendinosus tendons. Clinical and radiographic preoperative findings of patients are in Table 1. No tibial tubercle transfer or other surgical procedures were needed according to the examination results.
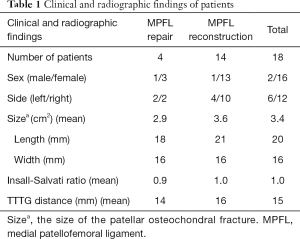
Full table
All patients were satisfied with the outcomes after surgery. No recurrence of patellar dislocation and other complication was found. Twelve of the 18 patients fully returned to physical activity, and the other 6 patients could also perform daily activities independently. Lysholm score increased from preoperative average (37.6, SD =6.8) to (80.9, SD =7.4) at the latest follow-up, and Kujala score increased from preoperative average (45.9, SD =6.4) to (89.4, SD =6.8) at the latest follow-up; the difference was statistically significant (P<0.01).
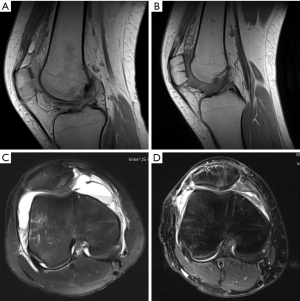
Each patient had two-viewed X-ray (Figure 2A), CT, and MR exams preoperatively. MRI showed lateral femoral condylar bone marrow edema and MPFL lesions (Figure 2B). Computer tomography reconstruction images were also available for further diagnosis of the OCFs (Figure 2C,D). All 18 patients underwent X-ray (Figure 3) and MRI examinations postoperatively. Postoperative MRI showed the fixation fracture fragments and the image of drill channels (Figure 4). All of them showed good healing of the OCFs. However, the MRI showed that 4 patients had anterior patellar bursa with no clinical symptoms. There were small areas of cartilage thinning but no obvious sign of joint degeneration.


Discussion
As a common injury of the knee, patellar dislocation mainly occurs in young people and athletes (11). Patellar or femoral condylar OCFs often combines with a MPFL injury (12,13) as the medial patellar facet and the lateral femoral condyle shear against each other. Preoperative MRI results of patients following patellar dislocation are mainly consistent with the surgical findings (14,15), which highlights the importance of an MRI scan in early diagnosis.
It remains controversial whether or not to choose a conservative treatment or a surgical treatment for the patients of a first-time acute patellar dislocation (16). Surgical fixation should be performed for the patellar dislocation complicated by OCFs, even if it is a primary dislocation (17). Buckwalter et al. believed that for large OCFs, without effective reduction and fixation, even if the fracture region had formed fibrous cartilage, the process of articular degeneration may be accelerated (18). Fragments of smaller size can be removed as loose bodies, and the larger ones should be fixed to restore knee function. According to the previous study, when the fragment’s diameter is less than 5 mm, it is recommended to be removed at the time of knee arthroscopy (19). Buckwalter et al. (20) suggested that the fragments within 3–4 mm in diameter could take conservative treatment or be removed as loose bodies, while those bigger than 9 mm in diameter required surgical fixation.
Various materials have been reported in the fixation of patellar or lateral condylar OCFs, including metal screws (21), bioabsorbable screws or pins (6,8,22), bone screws (23), and suture (10,24). Bioabsorbable screws or bone screws have the advantage of not requiring a second surgery for fixation removal, whereas bioabsorbable materials still have certain complications, such as allergic reactions (25), breakage (26), or loosening (27,28).
The purpose of surgical fixation is to restore the articular surface congruity, provide compression between the fragment and the patella for osseous healing, and ensure rotational stability to allow an immediate range of motion. According to the present study, the novel absorbable suture fixation method has its advantages. Firstly, the bone tunnels for penetrating PDS suture are smaller than screws, which cause less damage to the osteochondral fragments. Secondly, the compression pressure can distribute evenly to the cartilage surface, which provides good stability and makes early non-weight-bearing exercises possible. Also, absorbable suture fixation does not require removal and has its specific economic superiority.
Additionally, suture fixation may cause anterior patellar bursa by leading fluid flow through the bone tunnel (29). In this study, we also found that 4 out of 18 patients had anterior patellar bursa after surgery without obvious symptoms.
There were some limitations to the present study. The sample size is relatively small, which prompts further study in the future. Also, this is a retrospective study with no control group. Longer term follow-up and a comparative control study with different fixation methods could garner more powerful results.
Conclusions
To summarize, for the patellar dislocation combined with OCFs, absorbable suture fixation promises to be a simple and reliable method for treatment. Mid-term follow-up from the present study showed full recovery of knee function outcomes. Meanwhile, imaging evidence confirmed the OCFs healing.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The institutional review board approved this study, and the informed consent was signed and obtained from each patient.
References
- Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med 2004;32:1114-21. [Crossref] [PubMed]
- Mashoof AA, Scholl MD, Lahav A, et al. Osteochondral injury to the mid-lateral weight-bearing portion of the lateral femoral condyle associated with patellar dislocation. Arthroscopy 2005;21:228-32. [Crossref] [PubMed]
- Milgram JW, Rogers LF, Miller JW. Osteochondral fractures: mechanisms of injury and fate of fragments. AJR Am J Roentgenol 1978;130:651-8. [Crossref] [PubMed]
- Nietosvaara Y, Aalto K, Kallio PE. Acute patellar dislocation in children: incidence and associated osteochondral fractures. J Pediatr Orthop 1994;14:513-5. [Crossref] [PubMed]
- Nomura E, Inoue M, Kurimura M. Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy 2003;19:717-21. [Crossref] [PubMed]
- Jehan S, Loeffler MD, Pervez H. Osteochondral fracture of the lateral femoral condyle involving the entire weight bearing articular surface fixed with biodegradable screws. J Pak Med Assoc 2010;60:400-1. [PubMed]
- Kono M, Mori R, Uchio Y. Bone screws have advantages in repair of experimental osteochondral fragments. Clin Orthop Relat Res 2012;470:2043-50. [Crossref] [PubMed]
- Walsh SJ, Boyle MJ, Morganti V. Large osteochondral fractures of the lateral femoral condyle in the adolescent: outcome of bioabsorbable pin fixation. J Bone Joint Surg Am 2008;90:1473-8. [Crossref] [PubMed]
- Lee BJ, Christino MA, Daniels AH, et al. Adolescent patellar osteochondral fracture following patellar dislocation. Knee Surg Sports Traumatol Arthrosc 2013;21:1856-61. [Crossref] [PubMed]
- Pritsch M, Velkes S, Levy O, et al. Suture fixation of osteochondral fractures of the patella. J Bone Joint Surg Br 1995;77:154-5. [Crossref] [PubMed]
- Hinton RY, Sharma KM. Acute and recurrent patellar instability in the young athlete. Orthop Clin North Am 2003;34:385-96. [Crossref] [PubMed]
- Lording T, Lustig S, Servien E, et al. Chondral Injury in Patellofemoral Instability. Cartilage 2014;5:136-44. [Crossref] [PubMed]
- Seeley MA, Knesek M, Vanderhave KL. Osteochondral injury after acute patellar dislocation in children and adolescents. J Pediatr Orthop 2013;33:511-8. [Crossref] [PubMed]
- Elias DA, White LM, Fithian DC. Acute lateral patellar dislocation at MR imaging: injury patterns of medial patellar soft-tissue restraints and osteochondral injuries of the inferomedial patella. Radiology 2002;225:736-43. [Crossref] [PubMed]
- Kirsch MD, Fitzgerald SW, Friedman H, et al. Transient lateral patellar dislocation: diagnosis with MR imaging. AJR Am J Roentgenol 1993;161:109-13. [Crossref] [PubMed]
- Sillanpää PJ, Maenpaa HM. First-time patellar dislocation: surgery or conservative treatment? Sports Med Arthrosc 2012;20:128-35. [Crossref] [PubMed]
- Stefancin JJ, Parker RD. First-time traumatic patellar dislocation: a systematic review. Clin Orthop Relat Res 2007.93-101. [Crossref] [PubMed]
- Buckwalter JA, Brown TD. Joint injury, repair, and remodeling: roles in post-traumatic osteoarthritis. Clin Orthop Relat Res 2004.7-16. [Crossref] [PubMed]
- Stanitski CL, Paletta GJ. Articular cartilage injury with acute patellar dislocation in adolescents. Arthroscopic and radiographic correlation. Am J Sports Med 1998;26:52-5. [Crossref] [PubMed]
- Buckwalter JA, Martin JA, Olmstead M, et al. Osteochondral repair of primate knee femoral and patellar articular surfaces: implications for preventing post-traumatic osteoarthritis. Iowa Orthop J 2003;23:66-74. [PubMed]
- Hoshino CM, Thomas BM. Late repair of an osteochondral fracture of the patella. Orthopedics 2010;33:270-3. [PubMed]
- Matsusue Y, Nakamura T, Suzuki S, et al. Biodegradable pin fixation of osteochondral fragments of the knee. Clin Orthop Relat Res 1996.166-73. [Crossref] [PubMed]
- Kumahashi N, Kuwata S, Imade S, et al. Fixation of osteochondral fractures of the patella using autologous bone screws when reconstructing the medial patellofemoral ligament after recurrent patellar dislocation: report of two cases. J Orthop Sci 2014;19:359-64. [Crossref] [PubMed]
- Böstman OM, Pihlajamaki HK. Adverse tissue reactions to bioabsorbable fixation devices. Clin Orthop Relat Res 2000.216-27. [Crossref] [PubMed]
- Mastrokalos DS, Paessler HH. Allergic reaction to biodegradable interference poly-L-lactic acid screws after anterior cruciate ligament reconstruction with bone-patellar tendon-bone graft. Arthroscopy 2008;24:732-3. [Crossref] [PubMed]
- Lembeck B, Wulker N. Severe cartilage damage by broken poly-L-lactic acid (PLLA) interference screw after ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 2005;13:283-6. [Crossref] [PubMed]
- Macdonald P, Arneja S. Biodegradable screw presents as a loose intra-articular body after anterior cruciate ligament reconstruction. Arthroscopy 2003;19:E22-4. [Crossref] [PubMed]
- Millington KL, Shah JP, Dahm DL, et al. Bioabsorbable fixation of unstable osteochondritis dissecans lesions. Am J Sports Med 2010;38:2065-70. [Crossref] [PubMed]
- Marberry KM, Ginsburg Z. Extra-articular synovial fluid extravasation following operative fixation of an osteochondral fracture of the patella. Orthopedics 2012;35:e1267-71. [Crossref] [PubMed]


