
Systemic therapy of elderly patients with advanced non-small cell lung cancer—individualized treatment is key
Approximately 2.1 million individuals are diagnosed with lung cancer worldwide every year. Non-small cell lung cancer (NSCLC) comprises 80−85% of these cancers. About 40% of patients with NSCLC present with advanced disease at the time of initial diagnosis and receive palliative therapy. Patients without documented driver mutations in their cancers receive first-line chemotherapy with platinum-based doublets. Chemotherapy can be combined with bevacizumab or necitumumab in selected patients. At the time of disease progression, these patients are treated with docetaxel plus/minus nintedanib, docetaxel plus/minus ramucirumab, pemetrexed, erlotinib or afatinib. Immune checkpoint inhibitors have recently become part of the standard treatment for patients with advanced NSCLC. Patients with driver mutation-positive NSCLC receive first-line therapy with corresponding tyrosine kinase inhibitors.
Patients who are 70 years or older comprise up to 50% of patients with advanced NSCLC (1). In comparison to younger patients, these elderly patients often have impaired organ functions, high co-morbidity rates, a higher risk for increased toxicity of systemic therapies, a greater need for social support, and shorter life expectancy. These specific characteristics must be considered when selecting elderly patients for palliative therapy. In particular, elderly patients require well tolerated treatment protocols, enhanced supportive care and careful monitoring during treatment.
Chemotherapy in elderly patients
Elderly patients were often under-represented in or excluded from clinical trials. Therefore, data on palliative chemotherapy are limited for elderly patients with advanced NSCLC. Available data are based on either subgroup analyses of trials or few trials specifically performed in elderly patients. Subgroup analyses of major trials suggested similar survival outcomes between elderly and younger patients but more frequent dose reductions among elderly patients. The most relevant phase 3 trials specifically conducted in elderly patients are summarized in Table 1. The ELVIS trial demonstrated superior overall survival and possibly also quality of life for vinorelbine compared to best supportive care alone and established vinorelbine as standard treatment for elderly patients (2). Because of its good tolerability and ease of administration, gemcitabine became another treatment option for elderly patients.
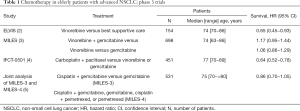
Full table
After single agents had become widely accepted for palliative chemotherapy of elderly patients, the question whether elderly patients benefit from doublets over single agents became of increasing clinical interest (6,7). The first strategy to improve outcome focussed on non-platinum-based doublets. Two phase 3 trials compared vinorelbine plus gemcitabine with either one of these drugs (3,8). Superior outcome could be demonstrated for the doublet in one trial (8) but not in the other trial (3). Because of these conflicting results, monotherapy remained the preferred treatment option for elderly patients with advanced NSCLC. The second strategy to improve outcome of palliative chemotherapy in elderly patients focussed on platinum-based doublets.
The MILES-3 and MILES-4 phase 3 trials compared cisplatin-based doublets with single agents (5). The rationale for these parallel trials were better outcome with doublets than single agents in patients with advanced NSCLC (6) and superiority of cisplatin-based protocols over carboplatin-based protocols (9). Overall survival was the primary endpoint and progression-free survival, objective response rate, toxicity and quality of life were secondary endpoints in both trials. Eligible patients had to have previously untreated advanced NSCLC with any histology (MILES-3) or non-squamous NSCLC (MILES-4). Further inclusion criteria were age 70 years or older and Eastern Cooperative Oncology Group (ECOG) performance status of 0 or 1. The MILES-3 trial randomized 299 patients to cisplatin plus gemcitabine or gemcitabine. The MILES-4 trial assigned 232 patients to cisplatin plus gemcitabine, gemcitabine, cisplatin plus pemetrexed, or pemetrexed. Both trials had to be closed prematurely because of slow patient accrual. A joint analysis of 531 patients from both trials was recently published (5). Patients had a median age of 75 years with approximately half of them being 75 years or older. ECOG performance status 0 and 1 was present in 44% and 56% of the patients, respectively. Most patients (94%) had stage IV disease. Non-squamous and squamous NSCLC were present in 70% and 30%, respectively. Overall survival was non-significantly improved among patients treated with cisplatin-based doublets compared to those treated with single agents. The hazard ratio was 0.86 (95% CI, 0.70−1.05; P=0.14). Median survival times were 9.6 (95% CI, 8.1−11.7) and 7.5 (95% CI, 6.2−9.5) months, respectively. Progression-free survival was significantly prolonged among patients treated with cisplatin-based doublets. The hazard ratio was 0.76 (95% CI, 0.63−0.92; P=0.006). Median progression-free survival times were 4.6 (95% CI, 4.1−5.3) and 3.0 (95% CI, 2.5−3.8) months, respectively. Overall response rates were higher with cisplatin-based doublets (15.5% versus 8.5%). The quality of life was not improved among patients treated with doublets compared to those treated with single agents. Thus, the combined analysis of the MILES-3 and MILES-4 trials failed to prove a survival benefit for patients treated with cisplatin-based doublets compared to those treated with single agents. The authors concluded that cisplatin-based doublets should no longer be proposed to elderly patients with advanced NSCLC.
Carboplatin-based doublets also lend themselves for palliative treatment of elderly patients with advanced NSCLC because these protocols do not require hydration, are more easily to administer and less time-consuming. The Intergroupe Francophone de Cancerologie Thoracique (IFT) 0501 phase III trial made use of these advantages and compared carboplatin plus paclitaxel with monotherapy consisting of either gemcitabine or vinorelbine in elderly patients with advanced NSCLC (4). The trial randomised 451 elderly patients with a median age of 77 years (range, 70−89 years) and a performance status WHO 0-1 in 73% of the patients. The doublet resulted in superior outcome in terms of overall survival, progression-free survival and response rates. The hazard ratio for death was 0.64 (95% CI, 0.52−0.78), median survival times were 10.3 months versus 6.2 months, and 1-year survival rates were 44.5% versus 25%. Progression-free survival also favoured the doublet with a hazard ratio of 0.51 (95% CI, 0.42−0.62), median progression-free survival times of 6.0 versus 2.8 months, and progression-free survival rates at one year of 13.4% versus 1.8%. Response rates at six weeks were 27% and 10%, respectively. Performance status and the activities of daily living score were prognostic but not predictive for the benefit of chemotherapy. The doublet was associated with slightly increased toxicity, in particular with regard to neutrophil counts (48% versus 12%), febrile neutropenia (9% versus 3%) and asthenia (10% versus 6%). Thus, the overall better efficacy at only slightly increased toxicity established carboplatin plus paclitaxel as a preferred treatment over monotherapy with gemcitabine or vinorelbine for fit elderly patients with advanced NSCLC.
Targeted therapies in elderly patients
Clinical trials with targeted therapies enrolled various percentages of patients older than 70 years. In a retrospective analysis of the ECOG Trial 4599, the addition of bevacizumab to carboplatin plus paclitaxel resulted in higher toxicity without improving overall survival in patients who were at least 70 years of age (10). In particular, neutropenia, bleeding, and proteinuria were increased in these patients. Based on these data, bevacizumab should be administered with caution in elderly patients. Based on subgroup analyses of large trials, patients aged 65 or older did not benefit from the addition of cetuximab to chemotherapy and patients aged 70 years or older did not benefit from the addition of necitumumab to chemotherapy (11,12).
Tyrosine kinase inhibitors directed against epidermal growth factor receptor, anaplastic lymphoma kinase (ALK) or c-ros oncogene 1 receptor tyrosine kinase (ROS1) were shown to be superior to chemotherapy also among elderly patients with degrees of benefit similar between elderly and younger patients (Table 2) (13-19). The potential side effects of these drugs, however, have to be carefully monitored among elderly patients in whom the clinical consequences from these side effects could be more pronounced. As an example, drug-mediated diarrhea could result in more severe dehydration and its consequencies in elderly than younger patients.

Full table
Immune checkpoint inhibitors in elderly patients
Immune checkpoint inhibitors recently entered clinical practice in patients with advanced NSCLC. In patients who had progressed after first-line chemotherapy, immune checkpoint inhibitors improved overall survival compared to docetaxel (20-23). In chemo-naive patients, pembrolizumab as single agent improved overall survival compared to first-line chemotherapy among patients with PD-L1 expression in ≥50% of tumor cells (24), and platinum-based doublets combined with pembrolizumab or atezolizumab prolonged overall survival and/or progression-free survival compared to chemotherapy alone (25-27). The combination nivolumab plus ipilimumab improved progression-free survival compared to chemotherapy among patients with high tumor mutational load (28). Therefore, treatment with immune checkpoint inhibitors has become standard for patients with advanced NSCLC. The magnitude of benefit from immune checkpoint inhibitors appeared to be somewhat less among patients aged 65 years or older compared to those younger than 65 years but the benefit remained clinically meaningful also in the older age group (Table 3). With regard to patients who are 70 years or older, no definite conclusions on the efficacy and toxicity of immune checkpoint inhibitors can be drawn because trials enrolled only low numbers of patients of this age group.
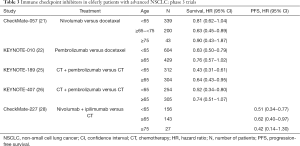
Full table
Conclusions
The authors of the MILES-3 and MILES-4 phase 3 trials attempted to clarify whether cisplatin-based doublets are suited as palliative chemotherapy for fit elderly patients with advanced NSCLC. Two major conclusions can be drawn from their studies. Firstly, accrual of elderly patients into clinical trials remains difficult. Although the trials planned to enrol 480 and 550 patients, respectively, only 531 patients in total could be randomized. Poor patient accrual into clinical trials is well known, remains particularly challenging in elderly patients, and its reasons are multifactorial. Potential solutions for increased accrual of elderly patients include better information of the general public about the importance of clinical trials, joint trials by co-operative groups and increased international co-operation. Another promising solution could be that clinical trials enrol patients regardless of age but stratify between patients below 70 years and those 70 years or older. Secondly, the MILES-3 and MILES-4 trials do not completely exclude a role of cisplatin-based chemotherapy in elderly patients. The number of randomized patients is insufficient in order to exclude a small but clinically still meaningful benefit. The possibility that cisplatin-based protocols might benefit patients is also supported by the fact that these protocols demonstrated longer progression-free survival and higher response rates (5). In my opinion, therefore, cisplatin-based doublets protocols can still be considered as a treatment option for fit elderly patients in whom increased efficacy may clearly outweigh toxicity.
Carboplatin-based doublets particularly lend themselves for elderly because of their easier administration and lack of requirement for hydration. Therefore, the superiority of carboplatin plus paclitaxel over single agents as demonstrated in the French trial (4) is of clinical relevance. The results in elderly patients are also consistent with those of a meta-analysis that demonstrated the superiority of doublets over single agents in patients with advanced NSCLC (6). The performance status was an important prognostic factor but did not predict for benefit of chemotherapy. These findings are consistent with subgroup analyses of phase III trials on palliative chemotherapy which suggested no differences in survival between younger and elderly patients.
In terms of the type of platin, carboplatin might be preferred for elderly patients, although cisplatin at lower doses, like in the MILES-3 and MILES-4 trials, might also be considered in patients with good performance status and adequate function of the heart and kidneys. Irrespective of the chemotherapy protocol, efficient antiemetic therapy, obstipation prophylaxis and adequate hydration are important in elderly patients. Because hematotoxicity is increased in elderly patients, the use of haematopoietic growth factors can be considered for selected patients. While geriatric assessment scales might be of some help, performance status and organ functions should primarily guide the selection of the chemotherapy protocols in elderly patients. Other relevant factors include tumor symptom burden, patient preference and life expectancy.
In summary, elderly patients with advanced NSCLC benefit from palliative chemotherapy. Fit patients with good performance may be offered platinum-based doublets and patients unfit for doublets should be considered for treatment with single agents. Elderly patients also clearly benefit from tyrosine kinase inhibitors. With regard to immune checkpoint inhibitors, additional data from clinical trials are necessary in order to define their impact on elderly patients with advanced NSCLC. Overall, individualization of treatment is particularly important for elderly patients. In order to achieve this, medical judgements by experienced doctors and nurses remain crucial.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has received speaker’ fees from Boehringer Ingelheim, and honoraria for Advisory Boards from Boehringer Ingelheim, Jansen and Takeda, and for Data Monitoring Committee participation from Genmab, Gedeon Richter, Merck Sharp Dohme and Regeneron.
References
- Davidoff AJ, Tang M, Seal B, et al. Chemotherapy and survival benefit in elderly patients with advanced non-small-cell lung cancer. J Clin Oncol 2010;28:2191-7. [Crossref] [PubMed]
- Effects of vinorelbine on quality of life and survival of elderly patients with advanced non-small-cell lung cancer. The elderly lung cancer vinorelbine Italian study group. J Natl Cancer Inst 1999;91:66-72. [Crossref] [PubMed]
- Gridelli C, Perrone F, Gallo C, et al. Chemotherapy for elderly patients with advanced non-small-cell lung cancer: the Multicenter Italian Lung Cancer in the Elderly Study (MILES) phase III randomized trial. J Natl Cancer Inst 2003;95:362-72. [Crossref] [PubMed]
- Quoix E, Zalcman G, Oster JP, et al. Carboplatin and weekly paclitaxel doublet chemotherapy compared with monotherapy in elderly patients with advanced non-small-cell lung cancer: IFCT-0501 randomised, phase 3 trial. Lancet 2011;378:1079-88. [Crossref] [PubMed]
- Gridelli C, Morabito A, Cavanna L, et al. Cisplatin-based first-line treatment of elderly patients with advanced non-small-cell lung cancer: joint analysis of MILES-3 and MILES-4 phase III trials. J Clin Oncol 2018;36:2585-92. [Crossref] [PubMed]
- Delbaldo C, Michiels S, Syz N, et al. Benefits of adding a drug to a single-agent or a 2-agent chemotherapy regimen in advanced non-small-cell lung cancer: a meta-analysis. JAMA 2004;292:470-84. [Crossref] [PubMed]
- Pirker R. Chemotherapy: advanced NSCLC - should we use doublets in elderly patients? Nat Rev Clin Oncol 2011;8:694-6. [Crossref] [PubMed]
- Frasci G, Lorusso V, Panza N, et al. Gemcitabine plus vinorelbine versus vinorelbine alone in elderly patients with advanced non-small-cell lung cancer. J Clin. Oncol 2000;18:2529-36. [Crossref] [PubMed]
- Ardizzoni A, Boni L, Tiseo M, et al. Cisplatin- versus carboplatin-based chemotherapy in first-line treatment of advanced non-small-cell lung cancer: an individual patient data meta-analysis. J Natl Cancer Inst 2007;99:847-57. [Crossref] [PubMed]
- Ramalingam SS, Dahlberg SE, Langer CJ, et al. Outcomes for elderly, advanced-stage non-small-cell lung cancer patients treated with bevacizumab in combination with carboplatin and paclitaxel: analysis of Eastern Cooperative Oncology Group Trial 4599. J Clin Oncol 2008;26:60-5. [Crossref] [PubMed]
- Pirker R, Pereira JR, Szczesna A, et al. Cetuximab plus chemotherapy in patients with advanced non-small-cell lung cancer (FLEX): an open-label randomised phase III trial. Lancet 2009;373:1525-31. [Crossref] [PubMed]
- Thatcher N, Hirsch FR, Luft AV, et al. Necitumumab plus gemcitabine and cisplatin versus gemcitabine and cisplatin alone as first-line therapy in patients with stage IV squamous non-small-cell lung cancer (SQUIRE): an open-label, randomised, controlled phase 3 trial. Lancet Oncol 2015;16:763-74. [Crossref] [PubMed]
- Mok TS, Wu YL, Thongprasert S, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 2009;361:947-57. [Crossref] [PubMed]
- Zhou C, Wu YL, Chen G, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol 2011;12:735-42. [Crossref] [PubMed]
- Wu YL, Zhou C, Hu CP, et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): an open-label, randomised phase 3 trial. Lancet Oncol 2014;15:213-22. [Crossref] [PubMed]
- Mok TS, Wu Y-L, Ahn M-J, et al. Osimertinib or Platinum-Pemetrexed in EGFR T790M-Positive Lung Cancer. N Engl J Med 2017;376:629-40. [Crossref] [PubMed]
- Soria JC, Ohe Y, Vansteenkiste J, et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med 2018;378:113-25. [Crossref] [PubMed]
- Solomon BJ, Mok T, Kim DW, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med 2014;371:2167-77. [Crossref] [PubMed]
- Sequist LV, Yang JC, Yamamoto N, et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol 2013;31:3327-34. [Crossref] [PubMed]
- Brahmer J, Reckamp KL, Baas P, et al. Nivolumab versus docetaxel in advanced squamous-cell non-small-cell lung cancer. N Engl J Med 2015;373:123-35. [Crossref] [PubMed]
- Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N Engl J Med 2015;373:1627-39. [Crossref] [PubMed]
- Herbst RS, Baas P, Kim DW, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet 2016;387:1540-50. [Crossref] [PubMed]
- Rittmeyer A, Barlesi F, Waterkamp D, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet 2017;389:255-65. [Crossref] [PubMed]
- Reck M, Rodríguez-Abreu D, Robinson AG, et al. Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med 2016;375:1823-33. [Crossref] [PubMed]
- Gandhi L, Rodríguez-Abreu D, Gadgeel S, et al. Pembrolizumab plus chemotherapy in metastatic non-small-cell lung cancer. N Engl J Med 2018;378:2078-92. [Crossref] [PubMed]
- Paz-Ares LG, Luft A, Tafreshi A, et al. Phase 3 study of carboplatin-paclitaxel/nab-paclitaxel with or without pembrolizumab for patients with metastatic squamous NSCLC. J Clin Oncol 2018;36:105. [Crossref]
- Socinski MA, Jotte RM, Cappuzzo F, et al. Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med 2018;378:2288-301. [Crossref] [PubMed]
- Hellmann MD, Ciuleanu TE, Pluzanski A, et al. Nivolumab plus ipilimumab in lung cancer with a high tumor mutational burden. N Engl J Med 2018;378:2093-104. [Crossref] [PubMed]


