A comparison of peri-operative outcomes between elective and non-elective total hip arthroplasties
Introduction
Exponential rises in healthcare costs and utilization have resulted in the recent adoption of several different cost-containing strategies (1-4). Some of the more recent efforts through the Patient Protection and Affordable Care Act (ACA) include the development of the Bundled Payments for Care Improvement (BPCI) initiative and the Comprehensive Care for Joint Replacement (CJR) reimbursement models (5,6). These models provide reimbursement based on pre-negotiated terms for in-hospital and 90-day post-operative episodes of care (EOC). These reimbursement models have shown to be effective in improving clinical outcomes while reducing healthcare utilization and costs after primary total knee arthroplasty (TKA) and total hip arthroplasty (THA). However, while considering these potential reimbursement options, it is important to note that primary arthroplasties are indicated for different pre-operative diagnoses, and that non-elective cases may have varying post-operative outcomes compared to elective cases that require different healthcare resources and cost structures.
Although the majority of primary THAs are performed electively for primary osteoarthritis or inflammatory conditions, there are still a substantial number performed for non-elective reasons. A recent database study published in the Journal of the American Medical Association (JAMA) (7) compared 117,157 elective THA patients to 117,157 hip fracture surgery patients, and found a higher risk of mortality (1.82% vs. 0.31%, P<0.001) and increased rates of major post-operative complications (5.88% vs. 2.34%) in the non-elective cohort. However, the patient population was limited to those in the French National Hospital Discharge Database who underwent hip surgery between 2010 and 2013. Additionally, these results may be confounded by the fact that elective THA outcomes were compared to those of potentially any other surgical procedure for hip fractures, rather than THA alone.
With substantial changes in the United States healthcare system, it is critical to perform large-scale, US-centered analyses on post-operative complication rates between different surgery types. These nationwide analyses are required to complement those performed overseas in order to provide a better understanding of post-operative THA complications and to facilitate decision-making for the implementation of newer reimbursement models. Therefore, the purpose of this study was to: (I) determine nationwide trends in operative times and (II) evaluate the association between surgery type, elective or non-elective with respect to (I) operative times; (II) hospital lengths-of-stay (LOS); (III) discharge disposition; (IV) 30-day post-operative complications; (V) reoperations; and (VI) readmissions.
Methods
Data source
Data was obtained from the American College of Surgeons National Surgical Quality Improvement Program (NSQIP) database to compare short-term outcomes of elective and non-elective THAs. The NSQIP database contains years of publicly available information prospectively collected at multiple hospitals in the United States (8). The database provides its users access to a wide range of variables such as patient demographics and peri-and post-operative outcomes that can be further analyzed with the goal of improving surgical management and care in the country. IRB approval was not required as the NSQIP database provides public, de-identified health data.
Study population
The NSQIP database was queried for all primary TKAs (CPT code 27130) performed between 2011 and 2016. A total of 139,636 cases were identified. Cases that did not specify surgery type (elective vs. non-elective; n=191) or that did not contain LOS data (n=53) were excluded. Additionally, cases with operative times less than 30 minutes or greater than 500 minutes (n=570), and those including BMIs of less than 15 or more than 70 (n=817) were also excluded. This yielded 130,261 cases (93%), which were then stratified into elective (n=125,293) and non-elective (n=4,968) cases.
The American College of Surgeons defines elective patients as those who meet the following criteria: “patient must be brought from their normal living environment on the day of the surgery” and a “previously scheduled procedure”. In contrast, non-elective cases were defined as: “patients who are inpatient at an acute care hospital”, “patients who are transferred from an ED”, “patients who are transferred from a clinic”, “patients who undergo an emergent/urgent surgical case”, and “patients whose admission to the hospital was on any date prior to the date of the scheduled surgical procedure for any reason”.
Cohort characteristics
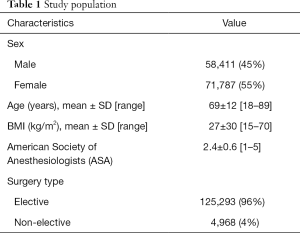
Each cohort was evaluated for age, sex, body mass index (BMI), and American Society of Anesthesiologists (ASA) score (Table 1). The average age of the elective patients was not significantly different from that of the non-elective patients (65±11 vs. 69±12 years, P=0.169; Table 2). The elective cohort had a greater proportion of male patients than the non-elective patients (45% vs. 35%, P<0.001; Table 2). Patients in the elective cohort also had a significantly greater mean BMI than the patients in the non-elective cohort (30±6 vs. 27±6 kg/m2, P<0.001), but a significantly lower ASA score (2±1 vs. 3±1, P<0.001; Table 2).
Full table

Full table
Outcomes of interest
Operative times, LOS, discharge destination, 30-day postoperative complications, reoperation, and readmissions rates were calculated for each cohort. Post-operative complications included superficial surgical site infections (SSI), deep SSI, organ/space SSI, wound dehiscence, pneumonia, reintubation, pulmonary embolism, ventilator required for more than 48 hours, renal insufficiency, acute renal failure, urinary tract infection, stroke, cardiac arrest, myocardial infarction, bleeding requiring transfusion, deep vein thrombosis (DVT), sepsis, and septic shock.
Data analyses
One-way analysis of variance (ANOVA) and Pearson correlation coefficients were used to evaluate associations between operative times and year of surgery. Univariate analyses of surgery type with the following outcomes of interest were also performed: operative times, LOS, and discharge disposition as well as 30-day complication, reoperation, and readmission rates. Chi-squared and t-tests were performed for categorical variables and continuous variables respectively.
A multiple linear regression model was used to evaluate the relationship of operative times with surgery types after adjusting for year of surgery and patient factors (age, sex, BMI, and ASA score). A log-transformed dependent variable was used to calculate the percentage difference in mean operative times. Multivariate logistic regression models adjusted for patient factors and year of surgery were used to evaluate associations of surgery type with complication, reoperation, and readmission rates.
Data analysis was performed with SPSS for Windows version 22.0 (IBM Corporation, Armonk, New York). A P value of less than 0.05 indicated statistical significance.
Results
Operative times
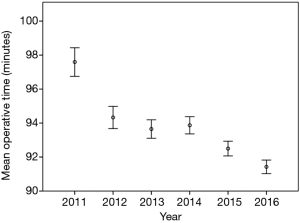
One-way ANOVA showed significant differences in operative times depending on the year of surgery (P<0.001). Operative time was inversely correlated with year of surgery (P<0.001; Figure 1) as operative time became progressively shorter from 2011 to 2016. The longest mean operative time was reported in 2011 with an average of 98±40 minutes and decreased to 91±37 minutes in 2016.
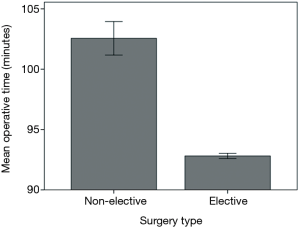
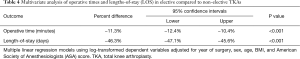
Elective patients had on average a significantly shorter operative time than non-elective patients by about 10 minutes (93±37 vs. 103±49 minutes, P<0.001; Figure 2). After adjusting for year of surgery, age, sex, and BMI, multivariate analysis showed that mean operative time remained significantly lower in the elective cohort compared to the non-elective cohort. Overall, elective THA surgeries were 11% shorter than the non-elective THAs [percent difference −11%; 95% confidence interval (CI), −12% to −10%, P<0.001].
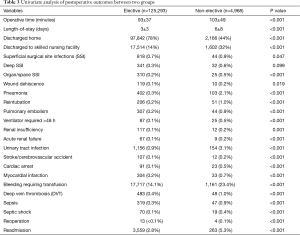
LOS and discharge disposition
Univariate analysis demonstrated that elective patients had a significantly shorter LOS than non-elective patients (3±3 vs. 6±8 days; P<0.001; Table 3). After adjusting for year of surgery, age, sex, and BMI, multivariate analysis showed that LOS remained significantly lower in the elective cohort compared to the non-elective cohort. Overall, mean LOS of elective THA patients were 46% shorter than those of the non-elective THA patients (percent difference −46.3%; 95% CI, −47.1% to −45.6%; P<0.001; Table 4).
Full table
Full table
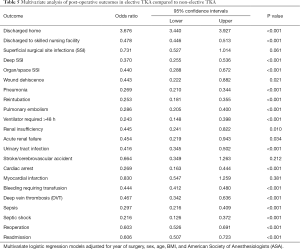
A significantly higher proportion of elective patients were discharged home after surgery than non-elective patients (78% vs. 44%; P<0.001; Table 3). In addition, fewer elective patients were discharged to a skilled nursing facility than non-elective patients (14% vs. 32%; P<0.001; Table 3). After multivariate analysis, elective patients remained more likely to be discharged home [odds ratio (OR) =3.676; 95% CI, 3.440–3.927; P<0.001; Table 5) and less likely to be discharged to a skilled nursing facility (OR =0.478; 95% CI, 0.446–0.513; P<0.001; Table 5) compared to non-elective THA patients.
Full table
30-day complication rates
After adjusting for year of surgery, age, sex, and BMI, elective patients had a lower risk of developing organ/space SSI (OR =0.440; 95% CI, 0.288–0.672; P<0.001), deep SSI (OR =0.370; 95% CI, 0.255–0.536; P<0.001), and wound dehiscence (OR =0.443; 95% CI, 0.222–0.882, P=0.021). The risk of the following additional medical complications were also lower among elective patients compared to non-elective patients: pneumonia (OR =0.269; 95% CI, 0.210–0.344; P<0.001), reintubation (OR =0.253; 95% CI, 0.181–0.355; P<0.001), pulmonary embolism (OR =0.286; 95% CI, 0.205–0.400; P<0.001), ventilator use for more than 48 hours (OR =0.243; 95% CI, 0.148–0.398; P<0.001), renal insufficiency (OR =0.445; 95% CI, 0.241–0.822; P=0.010), acute renal failure (OR =0.454; 95% CI, 0.219–0.943; P=0.034), UTI (OR =0.416; 95% CI, 0.345–0.502; P<0.001), cardiac arrest (OR =0.269; 95% CI, 0.163–0.444; P<0.001), bleeding requiring transfusion (OR =0.444; 95% CI, 0.412–0.480; P<0.001), DVT (OR =0.467; 95% CI, 0.342–0.636; P<0.001), sepsis (OR =0.297; 95% CI, 0.216–0.409; P<0.001), and septic shock (OR =0.216; 95% CI, 0.126–0.372; P<0.001).
30-day reoperation and readmission rates
Univariate analysis showed that elective patients had significantly lower rates of reoperation (<0.1% vs. 0.1%, P<0.001; Table 3) and readmission (2.8% vs. 5.3%, P<0.001; Table 3) than non-elective patients. After multivariate regression analysis, elective patients remained less likely to undergo any reoperations (OR =0.603; 95% CI, 0.526–0.691; P<0.001) or readmissions (OR =0.606; 95% CI, 0.507–0.723; P<0.001) compared to non-elective patients.
Discussion
Pre-operative planning has the potential to improve THA patient outcomes during and after surgery (9). Through patient optimization, risk factor modification and the anticipation of intra- and post-operative complications, elective procedures allow surgeons to adequately prepare for each surgery to decrease the rate of adverse outcomes and improve patient satisfaction. However, a direct, large-scale correlation between the effects of pre-operative planning on THA peri- and post-operative outcomes remains unclear, especially in large cohorts. This study demonstrated that elective THA surgeries were 11% shorter than non-elective THA surgeries even after adjusting for year of surgery, age, sex, and BMI and resulted in a 46% decrease in LOS compared to non-elective THAs. In addition to significant decreases in operative times and LOS, patients who underwent elective procedures with potentially more extensive pre-operative planning were also more likely to be discharged home and less likely to develop several different surgical and medical complications in the 30-day post-operative period.
The use of large databases such as the NSQIP database has inherent limitations. The NSQIP database provides restricted information, as only a specific set of variables are available to its users (8). Importantly, the variable used to determine pre-operative planning, as defined as elective surgery, does not specify the extent of pre-operative planning any further. Since data from the NSQIP database is collected from hundreds of hospitals across the United States, there may be variation in how elective patients undergo pre-operative planning. However, it is different from the non-elective group, in that elective procedures have been previously scheduled, allowing sufficient time even for minimal pre-operative planning such as templating or patient education. In addition, although it is required for clinical reviewers to be trained before entering patient data into the database, there may remain differences in data entry and familiarity with the database, which could result in missing data or errors. Hospital setting and protocols may also impact the amount of information that is available depending on the hospital, which may also lead to missing data. However, to limit the impact of missing data and coding errors, cases with missing data were excluded and only cases with specific ranges of operative times and BMI were included in the data analysis. Despite these exclusions, the study population analyzed constituted 93% of all primary THA cases isolated from the NSQIP database.
Other studies have found similar results. For example, in a Danish study, researchers observed that fast-track pre-operative planning, which consists in combining evidence-based clinical features with organizational optimization, decreased LOS by up to 3 days (6.3 to 3.1 days) in a series of 1,731 primary THAs and TKAs (10,11). Similarly, we found a 46% decrease in LOS between non-elective and elective surgeries (6 vs. 3 days, P<0.001). A different study in the UK compared the effects of an “enhanced recovery” protocol compared to the traditional protocol on outcomes in 4,500 THA and TKA patients (12). The program provided patients with enhanced patient education, pre-admission medication, and low-dose spinal anesthesia. Compared to the traditional cohort, patients in the enhanced recovery protocol had lower 30-day (0.5% to 0.1%, P=0.02) and 90-day (0.8% to 0.2%, P=0.01) mortality rates as well as median LOS that were 3 days shorter (6 vs. 3 days, P<0.001). Patients in the enhanced recovery cohort also required fewer blood transfusions (9.8% vs. 23%, P<0.001). Another study of 6,000 patients compared enhanced recovery protocols in THA and TKA patients to traditional THA and TKA patients (13). The enhanced recovery group had shorter LOS (3 vs. 6 days, P=0.01), required fewer blood transfusions (8% vs. 23%, P<0.001) and fewer reoperations (P=0.05). The enhanced recovery cohort also had a significantly lower 30-day incidence of myocardial infarction (0.4% vs. 0.9%, P=0.03). We observed similar decreases in LOS, blood transfusion (23% to 9%), and in the incidence of most 30-day complications in the elective cohort.
While the above studies show a decrease in LOS and blood transfusions in patients who underwent more pre-operative planning, most of the other complication or readmission rates do not significantly differ. For example, in the UK study, although the enhanced recovery cohort had a lower incidence of myocardial infarction, stroke, DVT, and pulmonary embolism, these results were not significantly lower (12). This contrasts with our results, as we observed that the elective group had significantly lower rates of MI, stroke, DVT, pulmonary embolism, among other complications. Of note, after adjusting for year of surgery, age, sex, and BMI in our study, the occurrences of stroke and MI were no longer significantly different. Therefore, some of those differences between studies may be accounted for by patient characteristics. Additionally, the Danish study found that readmission rates were not significantly different between the two cohorts (11). However, we observed that the elective group had significantly lower readmission rates than the non-elective group (2.8% vs. 5.3%, P<0.001) on univariate and multivariate analyses. While the Danish study took place from 2004 to 2008, the patients from our study were operated on between 2011 and 2016 and therefore advances in pre-operative planning and templating technologies could explain this discrepancy. New technologies such as CT-based 3D-templating could account for lower readmission rates and more successful surgeries than 10 years prior (14,15). As the accuracy of implant size prediction improves, surgeries may be faster and fewer complications are likely to develop with a resulting decrease in short-term reoperation and readmission rates.
Conclusions
This study demonstrated that pre-operative planning can benefit patients and healthcare providers alike. We observed that patients in the elective cohort had shorter operative times and LOS and were more likely to be discharged home compared to the non-elective cohort. Compared to non-elective THAs with minimal pre-operative planning, elective THAs were also associated with fewer short-term complications, readmissions or reoperations. These results reflect the development of more efficient surgical techniques, such as CT-based 3D-templating, as well as improved pre- and intra-operative planning guides. Moreover, these results highlight important discrepancies in short-term outcomes between elective and non-elective THAs that warrant consideration when implementing alternative reimbursement models for EOC.
Acknowledgements
None.
Footnote
Conflicts of Interest: MA Mont: AAOS, Cymedica, DJ Orthopaedics, Johnson & Johnson, Journal of Arthroplasty, Journal of Knee Surgery, Microport, National Institutes of Health (NIAMS & NICHD), Ongoing Care Solutions, Orthopedics, Orthosensor, Pacira, Peerwell, Performance Dynamics Inc, Sage, Stryker: IP royalties, Surgical Technologies International, Kolon TissueGene. The other authors have no conflicts of interest to declare.
Ethical Statement: IRB approval was not required as the NSQIP database provides public, de-identified health data.
References
- Padegimas EM, Verma K, Zmistowski B, et al. Medicare Reimbursement for Total Joint Arthroplasty: The Driving Forces. J Bone Joint Surg Am 2006;98:1007-13. [PubMed]
- Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 2007;89:780-5. [PubMed]
- Peterson J, Sodhi N, Khlopas A, et al. A Comparison of Relative Value Units in Primary versus Revision Total Knee Arthroplasty. J Arthroplasty 2018;33:S39-S42. [Crossref] [PubMed]
- Sodhi N, Piuzzi NS, Khlopas A, et al. Are We Appropriately Compensated by Relative Value Units for Primary vs Revision Total Hip Arthroplasty? J Arthroplasty 2018;33:340-4. [Crossref] [PubMed]
- Sood N, Shier VL, Nakata H, et al. The Impact of Comprehensive Care for Joint Replacement Bundled Payment Program on Care Delivery. J Arthroplasty 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Shah CK, Keswani A, Chi D, et al. Nonelective Primary Total Hip Arthroplasty: The Effect of Discharge Destination on Postdischarge Outcomes. J Arthroplasty 2017;32:2363-9. [Crossref] [PubMed]
- Le Manach Y, Collins G, Bhandari M, et al. Outcomes After Hip Fracture Surgery Compared With Elective Total Hip Replacement. JAMA 2015;314:1159-66. [Crossref] [PubMed]
- NSQIP.About ACS.
- Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg 2002;183:630-41. [Crossref] [PubMed]
- Husted H, Kristensen BB, Andreasen SE, et al. Time-driven activity-based cost of outpatient total hip and knee arthroplasty in different set-ups. Acta Orthop 2018;89:515-21. [Crossref] [PubMed]
- Husted H, Otte KS, Kristensen BB, et al. Readmissions after fast-track hip and knee arthroplasty. Arch Orthop Trauma Surg 2010;130:1185-91. [Crossref] [PubMed]
- Malviya A, Martin K, Harper I, et al. Enhanced recovery program for hip and knee replacement reduces death rate. Acta Orthop 2011;82:577-81. [Crossref] [PubMed]
- Khan SK, Malviya A, Muller SD, et al. Reduced short-term complications and mortality following Enhanced Recovery primary hip and knee arthroplasty: results from 6,000 consecutive procedures. Acta Orthop 2014;85:26-31. [Crossref] [PubMed]
- Hassani H, Cherix S, Ek ET, et al. Comparisons of Preoperative Three-Dimensional Planning and Surgical Reconstruction in Primary Cementless Total Hip Arthroplasty. J Arthroplasty 2014;29:1273-7. [Crossref] [PubMed]
- Marchand RC, Sodhi N, Bhowmik-Stoker M, et al. Does the Robotic Arm and Preoperative CT Planning Help with 3D Intraoperative Total Knee Arthroplasty Planning? J Knee Surg 2018. [Epub ahead of print]. [Crossref] [PubMed]