
There is another new method for cryopreserving small numbers of human sperm cells
The manuscript by Berkovitz et al. (1), re-opens the debate on a niche, but important, issue in in vitro fertilization concerning the cryopreservation of a very small number of spermatozoa form an ejaculate or with a surgical origin.
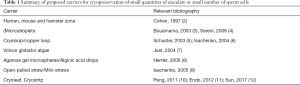
A small but not negligible percentage of infertile subjects can benefit from an efficient program of cryopreservation of the few available sperms because: (I) it can prevent the execution of repeated testicular biopsies in the azoospermic patient; (II) it may limit the risk of being without sperm on the day of in vitro fertilization; (III) it eliminates the issues associated with the coordination of the women’s oocyte retrieval with the surgical sperm retrieval. For these reasons several technical strategies have been proposed over time with the intent of cryopreserving spermatozoa ensuring good survival, easy recovery and fertilization potential at thawing and limiting in the meantime the sperm loss [see Table 1 and the review (13)]. However, due to limited efficiency and various shortcomings, none of these methods has been chosen by a preponderant portion of laboratories to become the method of choice. Possible limits to the dissemination of these strategies may be technical difficulties, excess costs and time, non-standardized results, limited demand in clinical practice. For this reason, novel cryopreservation approaches are welcome to the scientific community.
Full table
The common cryopreservation systems, whether they are slow, rapid or vitrification-based, have been showed to be applicable for the sperm cell. In fact, due to their specific cellular characteristics and in particular to the low presence of intracellular water and the high fluidity of the membrane, spermatozoa are rather resistant to cryo injuries in controlled conditions (14).
The method proposed by Berkovitz et al. (1) uses a sperm vitrification device to cryopreserve a small number of sperm cells in very reduced volumes of media (<1 microliter). The tool is certainly of interest as it can be directly used in the intracytoplasmic sperm injection (ICSI) dish at warming and the study is particularly valid as it consists of pre-clinical validation and subsequent results in the clinical setting including pregnancy and delivery outcomes. The proposed procedure is considered a vitrification technique made possible by the very reduced volume used together with the above-mentioned intrinsic characteristics of the sperm cell. It should be noted that the lack of direct contact between the sample and the liquid nitrogen and the heating at the time of thawing at room temperature make the temperature variation less rapid than generally occurs in the vitrification of reproductive cells. This condition could make it possible, at least in theory, the formation of deleterious ice crystals for cell survival, but the results seem to exclude this hypothesis. On the other hand, these two specific aspects have a significant value ameliorating the handling of the sample.
The method can be evaluated based on the following main points:
- Ease of use: the method seems to be practical even if laborious. However, it should be recognized that the time required is dictated mainly by the type of samples treated, and in particular by the time needed to find the few available spermatozoa, and not by the method itself. It should also be noted that the time devoted to research before freezing can significantly reduce the time required to search for sperm at the time of ICSI.
- Cell survival: the survival of spermatozoa is high even when the sample is particularly poor in sperm cells. In the case of availability of motile spermatozoa at freezing, it was possible to find cells with motility at thawing in over 90% of cases. This result is particularly encouraging and adds to the possibility of effectively using even immobile, but vital, sperm cells as in the case of spermatozoa coming from testicular biopsies. Although controls treated with the “standard” method are drawn from the same source as the intervention cohort, the comparison in the paper is not really informative since the standard cryopreservation technique has not been described in details and the reader can’t be sure that it was the best available procedure. Within these limits, results are encouraging beyond the comparison with other methods.
- Ease of recovery of spermatozoa at thawing: the spermatozoa are conveniently cryopreserved on a support compatible directly with the microinjection procedure and no further processing between thawing and ICSI is required. The carrier used for vitrification can be placed in the ICSI dish facilitating the detection of spermatozoa which occurs in the hands of the authors, in 96% of cases. This is a remarkable result based on which it is possible to estimate in advance the probability of being able to successfully use cryopreserved spermatozoa on a specific number of oocytes that will become available for ICSI.
- Safety: it has been reported an increased risk of contamination with pathogens during the vitrification procedure or cross-contamination during long-term storage (15,16). The risk of cross-contamination between cryopreserved cells in liquid nitrogen or of infection of patients through cryopreserved cells is probably overestimated (17); however, the possibility of eliminating the risk—even if low—of contamination through liquid nitrogen is to be considered important. The method proposed by Berkowitz (1), avoiding direct contact between the sample and liquid nitrogen during both vitrification and storage, offers the opportunity to minimize risks without the need for liquid nitrogen sterilization.
- Reproducibility and validation in clinical studies: reproducibility data are still limited because the results were obtained in only 2 centers. The particularity of the device and the constructive characteristics could limit the diffusion of the preliminary experiences as it will be necessary to have access to the commercial distribution of the device. The manuscript has the advantage of showing the results in the clinical practice, also reporting pregnancy rates and obstetric outcomes. This is an important fact that on the one hand confirms the potentiality of the method and on the other shows a methodological rigor often not found in similar areas.
- Cost: it is premature to estimate the costs of a potential use of this method. Certainly the cost may be higher than the traditional methods of cryopreservation, typically unexpensive. The need for a double session of micromanipulation in order to load the spermatozoa on the device and to retrieve them at the time of ICSI is to be taken into account. Today, the standard methods of conservation in bulk do not offer the opportunity to accurately estimate the chances of possible use at the time of ICSI. In this sense, the method proposed here seems to represent, even if not for the first time, an important advantage that nevertheless entails the need to increase the costs and time necessary for the freezing phase.
The possibility of cryopreserving sperm cells in a directly usable way for the ICSI technique is the main feature of the method by Berkovitz et al. Although this aspect is not fully new, it deserves consideration. Sun et al. (12) recently reported the successful use of a cryopiece system based on microstrips that can be placed at the bottom of ICSI dishes. The two methods share some important technical aspects aimed at ensuring an easy and efficient recovery of thawed sperm cells.
In the evaluation of the cost/effectiveness ratio it should be considered that the recovery of spermatozoa in apparently azoospermic subjects could be satisfactorily even using the freshly ejaculate specimen making the sample conserved only a stock not always necessary. These limits may have contributed to the development of the previously proposed methods.
In conclusion, the proposed method certainly represents a significant improvement of the techniques available today. However, it is possible to foresee that there is room for improvement both from the technical point of view and for the identification of the specific categories of patients who can effectively benefit from this approach.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Berkovitz A, Miller N, Silberman M, et al. A novel solution for freezing small numbers of spermatozoa using a sperm vitrification device. Hum Reprod 2018;33:1975-83. [Crossref] [PubMed]
- Cohen J, Garrisi GJ. Micromanipulation of gametes and embryos: Cryopreservation of a single human spermatozoon within an isolated zona pellucida. Hum Reprod Update 1997;3:453. [Crossref] [PubMed]
- Bouamama N, Briot P, Testart J. Comparison of two methods of cryoconservation of sperm when in very small numbers. Gynecol Obstet Fertil 2003;31:132-5. [Crossref] [PubMed]
- Sereni E, Bonu MA, Fava L, et al. Freezing spermatozoa obtained by testicular fine needle aspiration: a new technique. Reprod Biomed Online 2008;16:89-95. [Crossref] [PubMed]
- Schuster TG, Keller LM, Dunn RL, et al. Ultra-rapid freezing of very low numbers of sperm using cryoloops. Hum Reprod 2003;18:788-95. [Crossref] [PubMed]
- Isachenko V, Isachenko E, Katkov II, et al. Cryoprotectant-free cryopreservation of human spermatozoa by vitrification and freezing in vapor: effect on motility, DNA integrity, and fertilization ability. Biol Reprod 2004;71:1167-73. [Crossref] [PubMed]
- Just A, Gruber I, Wöber M, et al. Novel method for the cryopreservation of testicular sperm and ejaculated spermatozoa from patients with severe oligospermia: a pilot study. Fertil Steril 2004;82:445-7. [Crossref] [PubMed]
- Herrler A, Eisner S, Bach V, et al. Cryopreservation of spermatozoa in alginic acid capsules. Fertil Steril 2006;85:208-13. [Crossref] [PubMed]
- Isachenko V, Isachenko E, Montag M, et al. Clean technique for cryoprotectant-free vitrification of human spermatozoa. Reprod Biomed Online 2005;10:350-4. [Crossref] [PubMed]
- Peng QP, Cao SF, Lyu QF, et al. A novel method for cryopreservation of individual human spermatozoa. In Vitro Cell Dev Biol Anim 2011;47:565-72. [Crossref] [PubMed]
- Endo Y, Fujii Y, Shintani K, et al. Simple vitrification for small numbers of human spermatozoa. Reprod Biomed Online 2012;24:301-7. [Crossref] [PubMed]
- Sun J, Chen W, Zhou L, et al. Successful delivery derived from cryopreserved rare human spermatozoa with novel cryopiece. Andrology 2017;5:832-837. [Crossref] [PubMed]
- AbdelHafez F, Bedaiwy M, El-Nashar SA, et al. Techniques for cryopreservation of individual or small numbers of human spermatozoa: a systematic review. Hum Reprod Update 2009;15:153-64. [Crossref] [PubMed]
- Di Santo M, Tarozzi N, Nadalini M, Borini A. Human Sperm Cryopreservation: Update on Techniques, Effect on DNA Integrity, and Implications for ART. Adv Urol 2012;2012:854837. [Crossref] [PubMed]
- Fountain D, Ralston M, Higgins N, et al. Liquid nitrogen freezers: a potential source of microbial contamination of hematopoietic stem cell components. Transfusion 1997;37:585-91. [Crossref] [PubMed]
- Tedder RS, Zuckerman MA, Goldstone AH, et al. Hepatitis B transmission from contaminated cryopreservation tank. Lancet 1995;346:137-40. [Crossref] [PubMed]
- Cobo A, Bellver J, de los Santos MJ, et al. Viral screening of spent culture media and liquid nitrogen samples of oocytes and embryos from hepatitis B, hepatitis C, and human immunodeficiency virus chronically infected women undergoing in vitro fertilization cycles. Fertil Steril 2012;97:74-8. [Crossref] [PubMed]


