
Pathophysiology of pain in patients with peritoneal endometriosis
Endometriosis is a chronic disease characterized by the presence of hormone-responsive endometriotic glands and stroma outside the uterus that affect at least 4% of reproductive age women (1). It may be asymptomatic, but it frequently causes pain symptoms that negative influence social activities, working efficiencies and sexual life (2,3). Furthermore, endometriosis may cause symptoms depending on the location of the disease, such as urinary symptoms in case of bladder nodules and intestinal complains in case of colorectal lesions. Endometriosis may superficially involve the peritoneum (named superficial or peritoneal endometriosis, PE), it may deeply infiltrate the peritoneum and the abdominal organs (infiltration >5 mm, named deep infiltrating endometriosis, DIE) or it may involve the ovaries. The diagnosis of endometriosis is based on the visualization of the lesions during laparoscopy and, ideally, on the histological exam of the nodules excised during surgery. However, enhanced and non-enhanced transvaginal ultrasonography allow to accurately establish the presence of DIE and endometriomas (4,5). Endometriosis-related pain can be treated by administering hormonal therapies which usually suppress ovarian function (6-8); however, a percentage of patients do not respond to endocrine therapies and, thus, they require surgical treatment. However, pain may persist or recur after surgery exposing the patients to multiple surgical procedures during reproductive years.
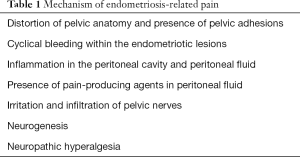
The pathophysiology of the association between pain and endometriosis is still enigmatic. The cause of pain is likely to be multifactorial (Table 1) (9,10). In patients with severe endometriosis with large ovarian cysts and DIE, pain can be caused by the distortion of the pelvic anatomy and by the presence of extensive adhesions (involving the uterus, the ovaries and the rectosigmoid) (Figure 1) (10). However, there is a poor correlation between the degree of pain and the severity of endometriosis. Some patients with intense pain symptoms have only small endometriotic implants on the peritoneal surface while other patients with severe endometriosis are almost asymptomatic. Therefore, other mechanisms should justify endometriosis-related pain. Ectopic endometriotic lesions are responsive to hormonal stimuli which may cause cyclical bleeding within the lesions. This process causes a chronic inflammation that promote pain (10). Furthermore, patients with endometriosis have an inflammatory process within the peritoneal cavity. In fact, women with endometriosis have increased concentration of inflammatory cells (macrophages and T lymphocytes), chemokines (MCP1, RANTES), inflammatory cytokines (IL1β, IL6, IL8, TNFα) and inflammatory molecules in the peritoneal fluid (11). These molecules and cells can sensitize peripheral nerves promoting the generation of pain (12). In addition, some pain-inducing molecules (such as prostaglandins) have elevated concentration in peritoneal fluid of women with endometriosis. Finally, endometriotic nodule can also directly irritate and infiltrate pelvic nerves promoting endometriosis-associated pain (13).
Full table

In the last 10 years, several studies demonstrated that endometriotic nodules contain new nerve fibers that may contribute to the pathogenesis of pain (9,10). A histological study by Anaf et al. found that, among patients with DIE, those with more severe pain had higher nerve fibers density within the endometriotic lesions and, in particular, within the fibrosis associated with endometriosis. Furthermore, in patients with more severe pain, endometriosis invaded both the nerves (intraneural invasion) and the spaces surrounding the nerves (perineural invasion) (14). An immunohistochemical study used protein gene product 9.5 (PGP 9.5 also named ubiquitin C-terminal hydrolase 1, UCHL-1) to demonstrate that there are more nerve fibers in DIE than in PE. In addition, this study showed that DIE is richly innervated by afferent fibers of nociceptors (sensory Aδ nerve fibers), unmyelinated sensory C nerve fibers, cholinergic and adrenergic nerve fibers. Finally, DIE strongly expressed nerve growth factor (NGF) and two receptors for neurotrophis: tropomyosin receptor kinase A (TrkA) and p75 (15).
Another immunohistochemical study showed that bowel DIE contained significantly more nerve fibers than other deep lesions (such as those on the uterosacral ligaments). In fact, sensory Aδ, sensory C, cholinergic, and adrenergic nerve fibers were abundantly present in intestinal DIE. These endometriotic lesions strongly expressed NGF, the receptors for neurotrophis and growth associated protein 43 (GAP43) (16). In patients with endometriosis, there is also evidence of a correlation between high nerve fiber number of in the eutopic endometrium and the intensity of pain (17). Endometriosis causes also a deregulation of the peripheral autonomic nervous system. In fact, a loss of sympathetic nerve close to endometriotic lesions and an increased expression in distant areas has been documented (18,19).
While most of previous research investigated nerve fibers density in DIE, Asally et al. in a study recently published in Molecular Neurobiology tried to better understand the pathophysiology of pain associated with PE (20). The authors used immunohistochemical staining to assess nerve fiber density, the expression of neurotrophins [glial cell derived neurotrophic factor (GDNF), persephin, neurotrophin-3 (NT-3) and neurotrophin-4 (NT-4)], neuronal guidance molecules [semaphorin 3E and slit guidance ligand 2 (Slit-2)] and their receptors (Plexin-D1 and Robo4) in PE. Four areas were identified within PE: the area inside the glandular epithelium; the area adjacent to the glandular epithelium (gland region); the area at the edge of the endometriotic stroma (stromal region); and an area at about 250 µm distance from the edge of the stroma (surrounding region). Furthermore, one peritoneal region collected away from ectopic endometriosis was evaluated (“healthy peritoneum”). Sensory nerve fibers had higher density in the stroma of PE compared to the surrounding region and to the healthy peritoneum. The authors observed that PE express neurotrophins, neuronal guidance molecules and their receptors which promote the neurogenesis. In detail, persephin, GDNF and NT-4 had higher expression in the gland region and in healthy peritoneum compared to the stromal and surrounding regions. NT-3 was similarly expressed in all the areas examined in the study. Neuronal guidance molecules and their receptors were overexpressed in the glandular epithelium. Semaphorin 3E was overexpressed in the gland region and in the heathy peritoneum compared to the surrounding region. Semaphorin 3E receptor and Plexin-D1 were overexpressed in the gland region and in the surrounding region. Slit-2 was more expressed in the gland region than in the other areas. Slit-2 receptor and Robo-4 were overexpressed in the gland region and stromal region. Therefore, the authors hypothesized that the overexpression of neuronal guidance molecules and their receptors in PE facilitates neurogenesis in this tissue. Thus, this study improved our understanding of pain mechanisms in patients with PE.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ferrero S, Arena E, Morando A, et al. Prevalence of newly diagnosed endometriosis in women attending the general practitioner. Int J Gynaecol Obstet 2010;110:203-7. [Crossref] [PubMed]
- Aerts L, Grangier L, Streuli I, et al. Psychosocial impact of endometriosis: From co-morbidity to intervention. Best Pract Res Clin Obstet Gynaecol 2018;50:2-10. [Crossref] [PubMed]
- Ferrero S, Esposito F, Abbamonte LH, et al. Quality of sex life in women with endome-triosis and deep dyspareunia. Fertil Steril 2005;83:573-9. [Crossref] [PubMed]
- Guerriero S, Condous G, Van den Bosch T, et al. Systematic approach to sonographic evaluation of the pelvis in women with suspected endometriosis, including terms, defi-nitions and measurements: a consensus opinion from the International Deep Endome-triosis Analysis (IDEA) group. Ultrasound Obstet Gynecol 2016;48:318-32. [Crossref] [PubMed]
- Menada MV, Remorgida V, Abbamonte LH, et al. Transvaginal ultrasonography com-bined with water-contrast in the rectum in the diagnosis of rectovaginal endometriosis infiltrating the bowel. Fertil Steril 2008;89:699-700. [Crossref] [PubMed]
- Ferrero S, Barra F, Leone Roberti Maggiore U. Current and Emerging Therapeutics for the Management of Endometriosis. Drugs 2018;78:995-1012. [Crossref] [PubMed]
- Ferrero S, Alessandri F, Racca A, et al. Treatment of pain associated with deep endo-metriosis: alternatives and evidence. Fertil Steril 2015;104:771-92. [Crossref] [PubMed]
- Ferrero S, Remorgida V, Venturini PL. Current pharmacotherapy for endometriosis. Expert Opin Pharmacother 2010;11:1123-34. [Crossref] [PubMed]
- Morotti M, Vincent K, Becker CM. Mechanisms of pain in endometriosis. Eur J Obstet Gynecol Reprod Biol 2017;209:8-13. [Crossref] [PubMed]
- Asante A, Taylor RN. Endometriosis: the role of neuroangiogenesis. Annu Rev Physiol 2011;73:163-82. [Crossref] [PubMed]
- Ferrero S, Gillott DJ, Remorgida V, et al. Proteomic analysis of peritoneal fluid in women with endometriosis. J Proteome Res 2007;6:3402-11. [Crossref] [PubMed]
- Barcena de Arellano ML, Arnold J, Vercellino F, et al. Overexpression of nerve growth factor in peritoneal fluid from women with endometriosis may promote neurite out-growth in endometriotic lesions. Fertil Steril 2011;95:1123-6. [Crossref] [PubMed]
- Anaf V, Simon P, El Nakadi I, et al. Hyperalgesia, nerve infiltration and nerve growth factor expression in deep adenomyotic nodules, peritoneal and ovarian endometriosis. Hum Reprod 2002;17:1895-900. [Crossref] [PubMed]
- Anaf V, Simon P, El Nakadi I, et al. Relationship between endometriotic foci and nerves in rectovaginal endometriotic nodules. Hum Reprod 2000;15:1744-50. [Crossref] [PubMed]
- Wang G, Tokushige N, Markham R, et al. Rich innervation of deep infiltrating endo-metriosis. Hum Reprod 2009;24:827-34. [Crossref] [PubMed]
- Wang G, Tokushige N, Russell P, et al. Hyperinnervation in intestinal deep infiltrating endometriosis. J Minim Invasive Gynecol 2009;16:713-9. [Crossref] [PubMed]
- Zhang X, Lu B, Huang X, et al. Endometrial nerve fibers in women with endometriosis, adenomyosis, and uterine fibroids. Fertil Steril 2009;92:1799-801. [Crossref] [PubMed]
- Ferrero S, Haas S, Remorgida V, et al. Loss of sympathetic nerve fibers in intestinal endometriosis. Fertil Steril 2010;94:2817-9. [Crossref] [PubMed]
- Arnold J, Vercellino GF, Chiantera V, et al. Neuroimmunomodulatory alterations in non-lesional peritoneum close to peritoneal endometriosis. Neuroimmunomodulation 2013;20:9-18. [Crossref] [PubMed]
- Asally R, Markham R, Manconi F. The Expression and Cellular Localisation of Neuro-trophin and Neural Guidance Molecules in Peritoneal Ectopic Lesions. Mol Neurobiol 2018. [Epub ahead of print]. [Crossref] [PubMed]


