
Wilson disease—treatment perspectives
Introduction
Wilson disease (WD) is an autosomal recessive disorder of copper metabolism with pathological copper accumulation in different organs/tissues (mainly, liver and brain) with secondary organ damage and clinical symptoms related to this injury (mainly, hepatic, neurologic and psychiatric disorders) (1,2). WD is caused by mutations in the ATP7B gene that encodes the copper-transporting P-type ATPase, ATP7B, which is located mainly in the trans-Golgi network of hepatocytes and is involved in copper transport in the circulation and biliary excretion (2). Thus, according to WD pathogenesis, WD starts from liver (1,2).
WD belongs to just a few genetic, metabolic disorders that can, if diagnosed early, be successfully treated with pharmacological agents [chelators (d-penicillamine or trientine) or zinc salts, or both] with the goal of achieving a negative copper balance and lack of drug-related adverse events (1-5). To date, a negative copper body balance can be achieved therapeutically by: (I) mobilization of copper from tissues and increased urinary excretion (chelators) or (II) by decreased copper absorption from the digestive tract (zinc salts) (5). The ultimate treatment recommended in cases of acute liver failure or decompensated liver cirrhosis is liver transplantation (LT) (1,2,6-10). In LT, the disturbance of copper transport in WD hepatocytes is removed and normal liver copper metabolism is restored with corrected copper-transporting P-type ATPase function. We know, based on transplanted WD cases, that copper body metabolism is normalized after LT and patients no longer require anti-copper treatment (1,2,6-10).
Currently available pharmacological treatments for WD (d-penicillamine, trientine and zinc salts) are associated with several limitations. Firstly, although there is established efficacy in some patients, especially those with hepatic symptoms, neurological symptoms persist in about 50% of WD patients on treatment (2,11,12) and almost 10% deteriorate neurologically during treatment, often irreversibly (2,13). Secondly, about a third of WD patients suffer from drug-related adverse events, particularly on d-penicillamine, which lead to treatment discontinuation (WD treatment failure) or serious adverse events (nephrotic syndromes, myasthenia-like or lupus-like syndromes, or other autoimmune diseases) (1,2,14-21). Finally, WD treatment regimens are often complex and cumbersome (taking drugs on an empty stomach, 2 hours before meal, 3 times a day), which, together with adverse events, can result in poor compliance, with treatment failure as consequence (1,15,18,22). Problems with adherence are seen in almost 40% of WD patients (22). Due to the limitations of current WD treatments, there is a need to find new therapies with a better safety profile, without the possibility of neurological deterioration, with greater efficacy on neurological deficits, potentially taken once daily, as well as potential therapies to restore the function of ATP7B.
Perspectives of WD treatment
Investigations into future treatments for WD focus on: (I) pharmacological agents currently in clinical trials, e.g., bis-choline tetrathiomolybdate (TTM) and once-daily trientine; or (II) new treatment modalities currently tested in animal models, e.g., methanobactin or (III) cell/gene therapies that restore function of ATP7B, currently also being tested in animal models (23).
The potential new pharmacological treatments for WD particularly aim to avoid neurological deterioration during treatment. This may be achieved by better control of so-called “free copper” or non-ceruloplasmin bound copper (NCC). NCC can be calculated by subtracting ceruloplasmin-bound copper (3.15× ceruloplasmin in mg/L equals the amount of ceruloplasmin-bound copper in µg/L) from the total serum copper concentration (1). NCC was proposed as a diagnostic tool in WD (normal range <15 µg/dL; WD patients usually >25 µg/dL) and to monitor WD treatment (correct anti-copper treatment 5–15 µg/dL) (1,2,24). Of note, it has been suggested that paradoxical neurological deterioration is due to an increase in NCC at the beginning of WD treatment, especially after chelators use (13,25). Such data were presented in animal studies comparing chelators and TTM and also in clinical studies with bis-choline TTM where changes in calculated NCC was one of the endpoints (2,25,26).
However, NCC as a tool in WD diagnosis and treatment monitoring is not fully validated. Unfortunately, the equation for calculating NCC is only reliable at low ceruloplasmin levels. Further, due to inter-laboratory differences in ceruloplasmin assessment, different methods may lead to varying results, even false-negative results. There is a need to establish other tools to assess control of copper metabolism and measure “free” copper. Exchangeable copper is a new technique to determine plasmatic copper; however, this method is not widely used so far (apart from in France) and it is not validated in a large WD patient population (2).
Another common way to detect WD treatment efficacy is the determination of urinary copper after 2 days of chelator-treatment cessation (should be <100 µg/24 hours) or under therapy (should be 200–500 µg/24 hours during long-term chelating therapy and <100 µg/24 hours with long-term zinc use) (1,2). However, both methods show the systemic copper burden only indirectly, although they are helpful to detect treatment non-adherence (1,2).
In addition to pharmacological perspectives of WD treatment that aim to better control copper metabolism with different drugs with different advantages, another way to optimize WD treatment is by cell and gene therapy. As WD is a genetic disorder, replacement of defective hepatocytes with cells possessing normal ATPase7B function or genetic correction of the mutated ATP7B gene will normalize the copper metabolism more physiologically and may last lifelong (27-30). Below we present the current research activities in WD treatment, their initial results, limitations and perspectives (Table 1).
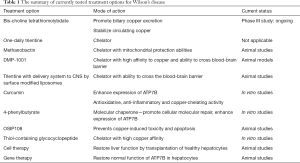
Full table
Pharmacological WD treatment options
Currently only two drugs/treatment options are being tested in phase II/III clinical trials: (I) bis-choline TTM and (II) one-daily trientine (pilot study).
Clinical trials of TTM as an ammonium salt were started by Brewer et al. in the 1980s (1,25,31). Ammonium TTM, working in different way than the chelators or zinc salts, led to a negative copper balance. Given with food, TTM complexes copper within food protein and prevents copper absorption. Given on an empty stomach, absorbed TTM complexes copper within albumin, preventing uptake by cells. This different mode of action led to the decision to use it 6 times a day (3 times before meals and 3 times after meals), which is a difficult regimen to use. Brewer et al. performed several clinical studies showing that treatment with TTM was safe, did not lead to neurological deterioration and led to rapid correction of copper metabolism in WD patients, without leading to an increase of serum “free copper” during treatment, which is observed with chelators. Based on his results, Brewer postulated to use TTM only in neurological WD and to discontinue chelators. However, the frequency of TTM dosing (6 times per day) and timing regarding meals was associated with a compliance problem and ammonium TTM was not used further apart from in trials (1,25,31). However, the idea of using TTM as a drug for WD with better control of copper metabolism than chelators and zinc salts, without paradoxical neurological deterioration, persisted. In 2014, the first multicenter phase II study of the bis-choline salt of TTM, WTX101, was initiated, testing once-daily dosing of 15–60 mg/day (mostly 30 mg/day) (26). In total, 28 WD patients were enrolled and 22 completed the study at week 24. Most patients achieved normalization or reduction of NCC and importantly, there were no cases of neurological deterioration (26). However, the data on copper metabolism were debatable and liver enzymes were elevated at higher doses (32). Nevertheless, a phase III FOCUS study with bis-choline TTM vs. standard of care (d-penicillamine/trientine/zinc salts) was started in 2018, with results expected in 2020.
Another tested approach to improve adherence to chelator therapy is reducing the frequency of drug application. Trientine is commonly given in 2–4 divided daily doses. Ala et al. performed a prospective pilot study of a single daily dose of trientine (33). Eight patients with stable WD were treated with a single daily dose of trientine (15 mg/kg) for 12 months. During that time, all patients remained clinically stable, without deterioration in liver function or liver cirrhosis (as assessed by FibroTest). Copper metabolism assessment during chelators use (urinary copper excretion) also showed evidence of treatment efficacy (mean 24-hour urine copper 313.4 µg/24 hours). However, the collection of urinary copper under chelation therapy may not provide reliable data. As this was not a prospective multicenter clinical trial and included only a small group of patients, further confirmative trials are needed.
Several drugs have been tested in animal models of WD, most promisingly: methanobactin (34), DMP-1001 (35), trientine with delivery system to the central nervous system (CNS) by surface modified liposomes (36) and curcumin (37-39); however, clinical trials in patients have not been performed to date.
Methanobactin is a modified peptide from the methanotrophic proteobacterium Methylosinus trichosporium with a very high copper affinity. These proteobacteria need a large amount of copper for their copper-dependent methane oxidase. They excrete methanobactin to sequester extracellular copper, then they reinternalize the methanobactin with copper into the cell and deliver copper to methane oxidase or store it within special proteins. Tested in acute liver failure in animal (rat) models of WD vs. standard chelators (d-penicillamine, trientine), only methanobactin was able to rapidly reverse the hepatocyte mitochondrial copper overload and acute liver failure. Additionally, no signs of drug toxicity in treated animals were recorded. Based on these preclinical studies, further evaluation in WD is warranted (34).
DMP-1001 (methyl 4-[7-hydroxy-10,13-dimethyl-3-{{4-pyridin-2ylmethyl)amino};butyl}amino)hexdecahydro-1H-cyclopental[a]phenanthren-17-yl]pentanoate) was used as a copper chelator firstly in tissues derived from WD patients (fibroblasts cultures), then further in a mice model of WD, where it lowered copper overload, especially in liver and brain, with increased copper elimination in feces and reduced WD symptoms (35). Additional advantages of DMP-1001 are oral intake, high affinity to copper, as well as the ability to cross the blood-brain barrier (BBB), which may result in reduced brain copper overload. This molecule appears to be attractive for WD treatment, however, it needs to be further tested, especially in humans (35).
Current WD drugs do not cross the BBB and the persistence of neurological symptoms or even neurological deterioration seem to be one of the biggest challenges in WD treatment. As such, a system to deliver trientine to the CNS by surface modified liposomes was developed by the team from Heidelberg to improve copper removal from brain tissue (36). Animal models confirmed its efficacy as high levels of trientine were recovered in brain tissue. The results are interesting; however, further studies are also needed in clinical trials.
Curcumin is another potential option for WD treatment as it has anti-inflammatory, antioxidant, copper-chelating as well as superoxide dismutase activity (37-39). The proposed mode of action includes decreased oxidative stress via free radicals scavenging, decreased lipid peroxidation and copper chelation via the ability to form curcumin-Cu(II) complexes. Together with the availability to cross the BBB, theoretically, curcumin may be a promising option for WD treatment. Due to its mode of action, curcumin has been widely investigated in other liver diseases (38). In alcoholic and non-alcoholic steatohepatitis in animal models, curcumin at high doses decreased liver fibrosis, steatosis and inflammation (along with reduction in pro-inflammatory cytokines, hepatocyte lipid accumulation, and oxidative stress markers) (38). Currently, in humans, two randomized double-blinded placebo studies in non-alcoholic fatty liver disease (NAFLD) were performed with curcumin treatment (500 or 1,000 mg/day for 8 weeks vs. placebo) with decreases of liver inflammation (laboratory values) as well as improved liver ultrasonography (NAFLD grading) (37-39). Until now, apart from one study performed by van den Berghe and colleagues in cell cultures (24), there are no data available regarding the use of curcumin in WD.
4-phenylbutyrate (4-PBA) is currently used as adjunctive therapy for urea cycle disorders (40). Recently, its property as a chemical chaperone was discovered. 4-PBA prevents protein aggregation in endoplasmic reticulum (ER) and may prevent ER stress and promote cellular repair (24,40). In addition to curcumin, van den Berghe et al. tested 4-PBA in cell cultures and these agents partially restored protein expression with most of the ATP7B mutations tested (24). These effects need to be further evaluated in animal models (24,40).
OSIP108 is a plant-derived decapeptide that prevents copper-induced toxicity and apoptosis in vitro (cells) and in in vivo models (zebrafish larvae), which also needs to be examined in further models (41).
Thiol-containing glycocyclopeptide (TCG) is a new anti-copper drug tested with success in hepatic cells lines as a copper chelator with high copper affinity (one study); however, TCG has not been tested in animal models of WD so far and the data regarding its efficacy are very limited (42).
Gene therapy
As in other genetic disorders, the idea of restoring systemic copper metabolism through gene transfer appears very promising. In theory, gene therapy introduced in asymptomatic WD patients should prevent clinical manifestations of WD. Additionally, in symptomatic cases, gene therapy may normalize copper metabolism and remove the stored copper from the liver leading to a disappearance of clinical symptoms (1,2).
So far, WD gene therapy has appeared successful in animal models of WD. The correct ATP7B gene can be delivered to hepatocytes with viral vectors. Initially, Merle et al. tested human immunodeficiency virus-derived lentiviral vectors (LV) (43). However, currently, the most promising approach are parvovirus adeno-associated viral vectors serotype 8 (AAV8) with attached ATP7B cDNA (29,30,44,45). The studies performed with AAV8 in mice models of WD documented that one injection led to normalization of copper metabolism (measured by serum holo-ceruloplasmin, urinary copper excretion, biliary copper excretion, brain and liver copper content), reduction of serum transaminases as well as normalization of liver histology (29). Given these encouraging results, clinical trials may be expected to start in 2019–2020.
Cell therapy
As LT in WD patients completely reverses systemic disturbances of copper metabolism, copper-transporting P-type ATPase from healthy donors may be capable of correcting copper metabolism following transplantation of healthy liver cells without full organ transplantation. Park et al. transplanted healthy hepatocytes by intrasplenic injection into 8-week old Long-Evans Cinnamon (LEC) rats with mutated ATP7B and clinical characteristics of WD (28). After further monitoring of the animals for 24 weeks, post-mortem analysis found reduced copper storage in hepatocyte-transplanted rats as well as a reduced chronic inflammatory response. These experiments were further confirmed by Sauer et al. (27), who additionally suggested that repeated hepatocyte transplantation lead to the better outcome.
Of course, the problem that needs to be addressed is how many healthy transplanted cells are required to improve liver copper metabolism. So far, data suggest that there is a need to achieve about 40% healthy hepatocytes to normalize copper metabolism (2,30) and this high number will probably limit cell therapy as an approach to WD treatment. Another study performed by Chen et al. (45) documented that transplantation of ATP-transduced bone marrow mesenchymal stem cells also decreased copper overload in LEC rats. However, apart from animal studies, there have been no studies with cell transplantations in humans with WD.
Conclusions
Several recent studies including new treatment modalities or gene/cell therapy in WD have been performed; however, currently TTM (bis-choline salt) is the only treatment in phase III development that seems to be close to approval due to its efficacy and safety in WD patients (2,26). Additionally, discussing WD treatment perspectives, methanobactin and curcumin look interesting as new and potentially safe treatment options; however, these have not been clinically tested in WD so far (34,37-39). Other treatment possibilities have been tested only in animal models, with promising results, and different modes of action that need to be verified in further studies, including in humans.
Current international recommendations on WD treatment exist (European Association for Study of Liver) and are updated (1). Until new treatment possibilities for WD are available, the most important considerations and objectives for treatment of WD are: (I) early diagnosis and anti-copper treatment introduction; (II) compliance and adherence with WD treatment (lifelong treatment); and (III) safety and efficacy assessment of anti-copper treatment during therapy (1,2).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- European Association for Study of Liver. EASL Clinical Practice Guidelines: Wilson’s Disease. J Hepatol 2012;56:671-85. [Crossref] [PubMed]
- Członkowska A, Litwin T, Dusek P, et al. Wilson Disease. Nat Rev Dis Primers 2018;4:21. [Crossref] [PubMed]
- Bruha R, Marecek Z, Pospisilova L, et al. Long-term follow-up of Wilson disease: natural history, treatment, mutations analysis and phenotypic correlation. Liver Int 2011;31:83-91. [Crossref] [PubMed]
- Członkowska A, Tarnacka B, Litwin T, et al. Wilson’s disease – cause of mortality in 164 patients during 1992-2003 observation period. J Neurol 2005;252:698-703. [Crossref] [PubMed]
- Członkowska A, Litwin T. Wilson disease - currently used anticopper therapy. Handb Clin Neurol 2017;142:181-91. [Crossref] [PubMed]
- Guillaud O, Dumortier J, Sobesky R, et al. Long term results of liver transplantation for Wilson’s disease: experience in France. J Hepatol 2014;60:579-89. [Crossref] [PubMed]
- Stracciari A, Tempestini A, Borghi A, et al. Effect of liver transplantation on neurological manifestations in Wilson’s disease. Arch Neurol 2000;57:384-6. [Crossref] [PubMed]
- Weiss KH, Schafer M, Gotthardt DN, et al. Outcome and developement of symptoms after orthotopic liver transplantation for Wilson disease. Clin Transplant 2013;27:914-22. [Crossref] [PubMed]
- Medici V, Mirante VG, Fassati LR, et al. Liver transplantation for Wilson’s disease: The burden of neurological and psychiatric disorders. Liver Transpl 2005;11:1056-63. [Crossref] [PubMed]
- Yagci MA, Tardu A, Karagul S, et al. Influence of liver transplantation on neuropsychiatric manifestations of Wilson disease. Transplant Proc 2015;47:1469-73. [Crossref] [PubMed]
- Litwin T, Dušek P, Członkowska A. Symptomatic treatment of neurologic symptoms in Wilson disease. Handb Clin Neurol 2017;142:211-23. [Crossref] [PubMed]
- Litwin T, Dusek P, Czlonkowska A. Neurological manifestations in Wilson’s Disease-possible treatment options for symptoms. Expert Opin Orphan Drugs 2016;4:719-28. [Crossref]
- Litwin T, Dzieżyc K, Karliński M, et al. Early neurological worsening in patients with Wilson’s Diseases. J Neurol Sci 2015;355:162-7. [Crossref] [PubMed]
- Czlonkowska A, Gajda J, Rodo M. Effects of long-term treatment in Wilson’s disease with d-penicillamine and zinc sulphate. J Neurol 1996;243:269-73. [Crossref] [PubMed]
- Członkowska A, Litwin T, Karlinski M, et al. D-penicillamine versus zinc sulfate as first-line therapy for Wilson’s Disease. Eur J Neurol 2014;21:599-606. [Crossref] [PubMed]
- Kalita J, Kumar V, Chandra S, et al. Worsening of Wilson Disease following penicillamine therapy. Eur Neurol 2014;71:126-31. [Crossref] [PubMed]
- Brewer GJ. Penicillamine should not be used as initial therapy in Wilson’s disease. Mov Disord 1999;14:551-4. [Crossref] [PubMed]
- Weiss KH, Gothardt DN, Klemm D, et al. Zinc monotherapy is not as effective as chelating agents in treatment of Wilson’s disease. Gastroenterology 2011;140:1189-98.e1. [Crossref] [PubMed]
- Brewer GJ, Terry CA, Aisen AM, et al. Worsening of neurologic syndrome in patients with Wilson’s disease with initial penicillamine therapy. Arch Neurol 1987;44:490-3. [Crossref] [PubMed]
- Kim B, Chung SJ, Shin HW. Trientine-induced neurological deterioration in a patient with Wilson’s disease. J Clin Neurosci 2013;20:606-8. [Crossref] [PubMed]
- Weiss KH, Stremmel W. Clinical considerations for an effective medical therapy in Wilson’s disease. Ann N Y Acad Sci 2014;1315:81-5. [Crossref] [PubMed]
- Masełbas W, Chabik G, Czlonkowska A. Persistence with treatment in patients with Wilson disease. Neurol Neurochir Pol 2010;44:260-3. [Crossref] [PubMed]
- Rupp C, Stremmel W, Weiss KH. Novel perspectives on Wilson disease treatment. Handb Clin Neurol 2017;142:225-30. [Crossref] [PubMed]
- van den Berghe PV, Stapelbroek J, Krieger E, et al. Reduced expression of ATP7B affected by Wilson disease-causing mutations is rescued by pharmacological folding chaperones 4-phenylbutrate and curcumin. Hepatology 2009;50:1783-95. [Crossref] [PubMed]
- Brewer GJ, Askari F, Dick RB, et al. Treatment of Wilson's disease with tetrathiomolybdate: V. Control of free copper by tetrathiomolybdate and a comparison with trientine. Transl Res 2009;154:70-7. [Crossref] [PubMed]
- Weiss KH, Askari FK, Czlonkowska A, et al. Bis-choline tetrathiomolybdate in patients with Wilson’s disease: an open-label, multicentre, phase 2 study. Lancet Gastroenterol Hepatol 2017;2:869-76. [Crossref] [PubMed]
- Sauer V, Siaj R, Stoppeler S, Bahde R, et al. Repeated transplantation of hepatocytes prevents fulminant hepatitis in a rat model of Wilson’s disease. Liver Transpl 2012;18:248-59. [Crossref] [PubMed]
- Park SM, Vo K, Lallier M, et al. Hepatocyte transplantation in the Long Evans Cinnamon rat model of Wilson’s disease. Cell Transplant 2006;15:13-22. [Crossref] [PubMed]
- Murillo O, Luqui DM, Gazquez C, et al. Long-term metabolic correction of Wilson’s disease in a murine model by gene therapy. J Hepatol 2016;64:419-26. [Crossref] [PubMed]
- Roy-Chowdhury J, Schilsky ML. Gene therapy of Wilson disease: A “golden” opportunity using rAAV on the 50th anniversary of the discovery of the virus. J Hepatol 2016;64:265-7. [Crossref] [PubMed]
- Brewer GJ, Askari F, Lorincz MT, et al. Treatment of Wilson disease with ammonium tetrathiomolybdate: IV. Comparison of tetrathiomolybdate and trientine in a double-blind study of treatment of the neurologic presentation of Wilson disease. Arch Neurol 2006;63:521-7. [Crossref] [PubMed]
- Stremmel W. Commentary on the paper entitled “Bis‐choline tetrathiomolybdate in patients with Wilson's disease: an open‐label, multicentre, phase II study” Hepatology 2019;69:901-3. [PubMed]
- Ala A, Aliu E, Schilsky ML. Prospective pilot study of single daily dose of trientine for the treatment of Wilson disease. Dig Dis Sci 2015;60:1433-9. [Crossref] [PubMed]
- Lichtmannegger J, Leitzinger C, Wimmer R, et al. Methanobactin reverses acute liver failure in a rat model of Wilson disease. J Clin Invest 2016;126:2721-35. [Crossref] [PubMed]
- Krishnan N, Felice C, Rivera K, et al. DPM-1001 decreased copper levels and ameliorated deficits in a mouse model of Wilson’s disease. Genes Dev 2018;32:944-52. [Crossref] [PubMed]
- Tremmel R, Uhl P, Helm F, et al. Delivery of copper-chelating trientine (TETA) to the central nervous system by surface modified liposomes. Int J Pharm 2016;512:87-95. [Crossref] [PubMed]
- Ji HF, Shen L. Potential of curcumin as a multifunctional agent to combat Wilson disease. Hepatology 2010;51:2226. [Crossref] [PubMed]
- Farzaei MH, Zobeiri M, Parvizi F, et al. Curcumin in liver diseases: a systematic review of the cellular mechanisms of oxidative stress and clinical perspective. Nutrients 2018;10:E855. [Crossref] [PubMed]
- Berzina A, Martinsone I, Svirkis S, et al. Curcumin effect on copper transport in HepG2 cells. Medicina 2018;54:14. [Crossref] [PubMed]
- Peña-Quintana L, Llarena M, Reyes-Suárez D, et al. Profile of sodium phenylbutyrate granules for the treatment of urea-cycle disorders: patient perspectives. Patient Prefer Adherence 2017;11:1489-96. [Crossref] [PubMed]
- Spincemaille P, Pham DH, Chandhok G, et al. The plant decapeptide OSIP108 prevents copper-induced toxicity in various models for Wilson disease. Toxicol Appl Pharmacol 2014;280:345-51. [Crossref] [PubMed]
- Pujol AM, Cuillel M, Renaudet O, et al. Hepatocyte targeting and intracellular copper chelation by a thiol-containing glycocyclopeptide. J Am Chem Soc 2011;133:286-96. [Crossref] [PubMed]
- Merle U, Encke J, Tuma S, et al. Lentiviral gene transfer ameliorates disease progression in Long-Evans cinnamon rats: an animal model for Wilson disease. Scand J Gastroenterol 2006;41:974-82. [Crossref] [PubMed]
- Uerlings R, Moreno D, Murillo O, et al. Brain copper storage after genetic long-term correction in a mouse model of Wilson disease. Neurol Genet 2018;4:e243. [Crossref] [PubMed]
- Chen S, Shao C, Dong T, et al. Transplantation of ATP7B-transduced bone marrow mesenchymal stem cells decreases copper overload in rats. PLoS One 2014;9:e111425. [Crossref] [PubMed]


