Perspectives of value-based policy making in child health care in Japan
Introduction
In Japan, a serious concern on the sustainability of health care has raised from rapid population aging, soaring medical expenditure, but stagnant economy. For the solution, the allocation of public health resource is expected to be based on a rational judgement on the social value, and health technology assessment (HTA) serves as a powerful tool to inform the policy maker on the “value” of health care by using the best scientific evidence on the medical, social, economic and ethical implications. It tackles an essential question: “how to maximize health outcomes with limited health resources and budgets”. As widely applied in the world to inform decision making, HTA has been recently advocated for the health insurance system in Japan. In 2012, a special advisory panel for cost-effectiveness evaluation was established within the Central Social Insurance Medical Council under the Ministry of Health, Labor and Welfare (MHLW). After 4 years preparation, since April 2016, the council has launched a pilot plan of cost-effectiveness evaluation for pricing and reimbursement of health technologies (e.g., drugs, medical devices and clinical practices) in the health insurance system. Discussions on major specific issues of the appraisal that haven’t clarified in the pilot plan among various stakeholders will continue in order to promote a formal introduction plan in the upcoming years (1).
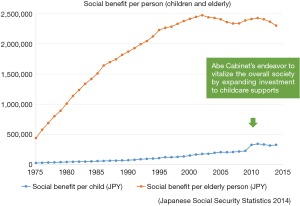
Child health care is inevitably influenced by such the tendency of value-based approach, while the related discussions and knowledge pooling for child health care are very rare in the country so far. As the very beginning stage of life course, health and development during childhood potentially contributes to productivity at both individual and societal level in future and has a long-term impact on health and wellbeing of human life. Although Japan is known for high quality, equity in utilization and good performance of health care, and has one of the best infant and child health outcomes in the world, epidemiological transition together with social transformation have brought a profound influence on the provision system of child health care and raised a challenging question how to evaluate the impacts of interventions and policies targeting children. The current population pattern is characterized as increasing aging population, continuing low fertility and shrinking proportion of children and young generation. During the past decades, the national social benefit budget for the elderly population has soared considerably; while policies targeting children, an essential preventive measure for rapid aging, has been left behind the priority until the Abe Cabinet’s Plan for Dynamic Engagement of All Citizens, which aims to boost economy, to vitalize society and to tackle issues of the aging and declining population and the recession (2). Compared to the elderly population, children have attracted much fewer social benefits (Figure 1). Meanwhile, partly due to stagnated economy, recently Japan’s traditional social pattern has gradually changed with increasing number of dual-income households and widening inequality. Childhood poverty rate is exceeding the average level of Organization for Economic Co-operation and Development (OECD) countries (3). A wide range of childcare supports in this background is now represented as 1 of 3 essential actions of Abe Cabinet’s Plan. The aim of this paper is to provide an overview of pediatric care and perspective of HTA development, under a context of epidemiological transition, social changes, and health system and policy making in Japan, with focus on two essential questions raising from the initiative of HTA: “What the value of child health care is” and “how to realize value-based approach in child health care”.
Child health issues in epidemiological transition
Epidemiological transition leads to a profound change in the pattern of disease burden in children. Recently, the top causes of child and adolescent mortality is first unintentional accidents, then followed by congenital malformations, cardiovascular disorders, cancers and suicide (4). The unprecedented progress and the endeavor of neonatal and pediatric medicine have largely improved child survival outcomes. The universal vaccination significantly reduced the incidence of acute infectious diseases (5). Recently in Japan, known for one of countries with the best child health outcomes in the world, the mortality due to congenital and neonatal disorders that would have occurred a generation ago has been dramatically averted. For example, survival of extremely preterm birth has been considerably improved (6). As much as 85% to 90% of infants born with congenital heart defects (CHDs) grow up to become adults (7). As the results, the decrease of the overall mortality has on aggregate led to relative increase in priority of two issues in child health care, targeting minority and majority of the overall children population, respectively: a largely expended need of the long-term care for survivors saved by advanced neonatal and pediatric medicine but with disabilities and chronic diseases; and an integrated support to child health and development targeting the majority of child population in various aspects.
A relevant proportion of health care for those with disabilities and chronic diseases is not curative, but needs life-long treatment and surveillance. Besides the facility-based medical services, home-based care provided by professionals and the social welfare service are urgently necessary for those pediatric patients as well. On the other hand, the current provision system doesn’t meet these needs: 22.9% of the tertiary and 40.2% of the secondary pediatric facilities don’t have a committee/team of home-based care (8). For those children, the provision system of medical services and that of social welfare services are completely separated. Moreover, in some pediatric chronic diseases such as CHDs and chronic kidney diseases (CKDs), which survival is now long enough to reach in adulthood, as well as in non-fatal but life-long disorders such as allergies, early-onset diabetes, and chromosomal abnormalities, transition of care from childhood to adulthood has recently been highlighted (9). Such the long-term care requires multidisciplinary involvement not only within different divisions of medicine, but also in various sectors such as social welfare and education, generating the efforts in the community.
As for the general population, among major problems in child and adolescent health presented are unhealthy behaviors on diet, physical activity and sleep, mental disorders, child abuse, bullying in the school, juvenile delinquency, sexual infectious diseases and injuries and harms. These health problems are “social” rather than “clinical” diseases, deriving from social environment for their development such as poor practices, anxiety and deficient social supports of child raising, poverty of children and expended gaps of the overall society. The solution is no longer limited in a disease-oriented curative approach, but also requires an integrated approach to comprehensively support child health and development, actively involving various stakeholders and professionals. For this, health promotion, primary prevention of diseases and injuries, and supports to parenthood besides clinical management of life-threatening complications have been recently added as the principle roles of pediatric care, with emphasis of active involvement of stakeholders at the community (10).
The pediatric care provision system
The pediatric care provision system has profoundly influenced by social changes such as increasing number of working mothers and dual-income households, and is expected to respond to increasing needs of professional supports to child-rearing of general population as well as the long-term care of those with chronic diseases and disabilities. It consists of three levels of the health facility: pediatric clinics and small hospitals at the primary level, regional pediatric center (pediatric department of general hospitals with around the clock emergency pediatric service) and community development pediatric center at the secondary level, and pediatric specialized hospitals and university hospitals at the tertiary level. Japan Pediatric Society intends to consolidate the pediatric care provision system in the country in Japan. In a total of 347 secondary medical care zones of the 47 prefectures, there are 399 regional pediatric centers and 106 core general hospitals and pediatric specialized hospitals registered (8). In those secondary medical care zones where neither the secondary nor the tertiary pediatric facility has been registered, Japan Pediatric Society plans to support a community development pediatric facility to strengthen the provision of pediatric care in the region level.
There have been some problems raising concerns on the sustainability of the pediatric division. Compared to that for adults, child health care is much more labor-intensive, while such the character has not well been reflected in the reimbursement tariff scheme of the health insurance, making it to be disadvantageous to that for adults. As the current health insurance system is based on fee-for-service and child health care has less practices on clinical examination and treatment compared to that for adults, the pediatric division often operate at a deficit loss. Moreover, according the latest survey of MHLW in 2014, the total number of pediatricians is 16,758, in which 60.3% working at hospitals with the average age of 43.0 years and 39.7% working at clinics with the average age of 60.3 years (11). Compared to decades ago, the aging of pediatricians is remarkable, making it difficult to maintain the pediatric emergency care and to respond to the increasing needs of night-time and weekend health care services. On the other hand, due to the heavy working load, disadvantages in the current health insurance system and worsened management, medical students tend to be less likely to desire to become a pediatrician, as there is no limitation for medical students to choose their specialty, causing a potential shortage of pediatricians and vicious cycle of personnel shortage and deteriorated working environment.
For the sustainability, the labor-intensiveness of pediatric care needs to be appropriately reflected in the reimbursement tariff scheme, which prices healthcare practices within the context of the universal health insurance system. The recent modification of the reimbursement tariff scheme and the national medical service plan has included those for children’s hospitalization, the pediatric intensive care unit (PICU), neonatal medicine, and the pediatric home-based care have been adopted (12). On the other hand, a discussion on the reimbursement for the advanced medicine and the expended preventive pediatric care is still ongoing. Although the decision on the pricing has been majorly based on the input of health services so far, in long-term it tends to depend on evaluation of the outcomes and the impacts based on the valid methodologies.
Financing child health care and its geographical disparity
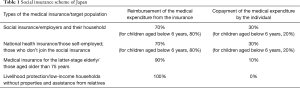
Japan is well known for a universal health insurance system covering all residents so-called “Kokumin Kaihoken” (Table 1). Within this system, the copayment rate for children depends on the age: 20% for those aged below 6 years and 30% for others, same as that for adults. The expensive medical costs are also subject to the health insurance system, and the identification of the expensiveness and its cap of the copayment is determined by a calculation scheme based on the household income.
Full table
Besides the social insurance system, children’s copayment is further covered fully or partly by various public subsidies funded by the central or the local government as well, including subsidies for medical costs of infants and children, as well as that to physical and mental disabilities, hospitalization of low-birthweight neonates, inpatient services for mental services, specific types of intractable and rare diseases, specific pediatric chronic diseases, livelihood protection and single-parent household. The entitlement and the user charge depending on the category of diseases or disabilities, health care services received and the household income. Because of the robust universal health insurance system, children have no restriction on healthcare accessibility by household income (13).
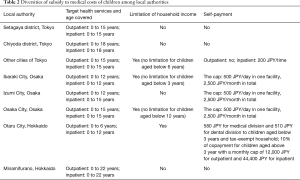
On the other hand, there is a huge geographical diversity in the public subsidies for medical costs of infants and children (14). According to a national survey, out-of-pocket payment of medical costs (including both those reimbursed later and self-paid) for children aged 0 to 4 years largely different among the 47 prefectures (14). Table 2 rises up the examples of some local authorities’ policy on the public subsidy for medical costs of infants and children in Tokyo, Osaka and Hokkaido. Diversities are present across not only among the 47 prefectures, but also among local authorities within each prefecture, in terms of health care services and age covered, upper limit of household income, and user charges across different local authorities. The range of age covered for the outpatient and the impatient service is from 0 to 18 years. Major options for the upper limit of the age subject to the subsidy are 12, 15 or 18 years. There are a relevant number of local authorities setting up an upper limit of the household income and user charges for the outpatient and the impatient service. In general, the outpatient and the impatient service of children aged below 6 years are fully subsidized in most local authorities without the upper limit of household income and user charges.
Full table
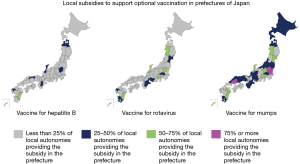
Such the geographical diversity also remains in the subsidy for optional vaccination provided by local authorities. Figure 2 summarized the proportion of local authorities that provide the subsidy fully or partly to support the vaccination for Hepatitis B, Rotavirus, and Mumps, respectively, in prefectures of Japan, among the surveyed local authorities. The survey was implemented by Know Vaccine Preventable Diseases, a non-profit organization during 2015 (15). The three vaccines are optional, rather than routine, and the decision whether to be vaccinated is made by parents. Because the optional vaccination is not covered by the social insurance, the payment is based on out-of-packet in general, unless local autonomies provide a subsidy to fully or partly cover it. Among all 47 prefectures, the number of the prefecture where less than 25% of local autonomies don’t have the subsidy for Hepatitis B, Rotavirus and Mumps are 40, 35 and 19, respectively (15). The target vaccines and the amount of the subsidy are different across local authorities even within each prefecture.
The decision making in local authorities often depends on various complicated factors such as the local financial status, epidemiological characteristics and political will to promote fertility and child rearing of the reproductive generation. Moreover, the Abe Cabinet’s Plan has promoted health financing to child health care. Still, expanding pediatric care services for the integrated support to child-rearing, addressing the geographical gap and strengthening the pediatric care provision system particularly at local level requires the injection of health resources, which challenges constrained health financing due to aging society at both central and local level, and impels to weigh the output against the input for decision making.
Limitations of the current methodology scheme of cost-effectiveness analysis (CEA) for child health care
Generation of evidence on health impacts and cost-effectiveness is a crucial process for value-based decision-making. Health impacts, the ultimate goal of every health technology, is an essential part of CEA. Although the “effectiveness” in CEA can be either effectiveness (clinical outcomes in a natural form, such as number of lives saved, complications prevented or diseases cured), utility (a generic and comprehensive metrics incorporating both length and health-related quality of life gained), or benefit (outcomes in monetary terms) (16), health utility measured by quality adjusted life year (QALY), has been regarded as a standard indicator to measure the impact of health technologies and recommended by most HTA agencies such as National Institute for Health and Care Excellence (NICE), as it facilitates comparison of health technologies with different purposes and outcomes. Similarly, the recent MHLW’s guideline for cost-effectiveness evaluation also requires a cost-utility analysis for targeted health technologies subject to appraisal, in which the health impacts are measured by QALYs and the incremental cost-effectiveness ratio (ICER) is calculated as costs per QALY gained (17).
On the other hand, the availability of such the evidence in children for priority setting lags behind due to limited methodologies to evaluate the outcomes/impacts of child health care. Compared to that in adults, the current standard methodology of CEA in children still has numerous limitations. As indicated by Ungar, among major limitations in the methodology are unclear perspective, incomplete costing, omission of productivity loss, and intermediate outcome measures (18). Particularly, there is no preference-based health utility measurement in children of all ages. The major methods to valuate health state, both direct choice approaches including standard gamble and time trade-off and indirect scaled instruments such as EQ-5D and Health Utility Index (HUI), are based on the report of an individual with adequate cognitive ability, and consequently not suitable for most children. Recently, child-friendly and child-specific health utility instruments such as EQ-5D-Y and Child Health Utility 9D (CHU9D) have been developed majorly targeting children with relevant cognitive ability to read and report their health in a simplified way. Preparation for the application of those instruments for Japanese children is ongoing. These instruments are nevertheless only applicable for children above 7 years. For very young children and those children unable to report their health status due to disabilities, researchers must rely on parent proxies to report health status and resource use, even though it cannot avoid potential biases. So far, there have been debates on whether health utility as measured by QALYs.
Besides the health utility soliciting individual preferences of choice for health states, health economists in pediatrics have recommended willingness-to-pay (WTP) to monetarize benefits of not only health but also non-health gains in terms of wellbeing of children and their family members and social welfare. Innovative methodologies, such as Discrete-choice experiment (DCE), have been tentatively applied to incorporate health and non-health gains of children and their family members by capturing preferences for one scenario over others. However, regarding the methodology, the instrument that is the most appropriate for measuring health impacts among children remains not clearly defined. The recent MHLW’s guideline compromises health impacts not measured by QALYs in case of such the technical limitation.
Refining the value of child health care
As pediatric care is shifting from a disease-driven curative approach to an integrated approach, the value of child health care now needs to be redefined with an integrated scope. As mentioned above, with rapid reduction of acute, severe and fatal diseases and increasing needs of comprehensive support to child-rearing to general population as well as long-term care to those with chronic diseases and disabilities, pediatric professionals need to tackle not only clinical diseases, but also “social diseases” such as various mental health problems in children and adolescents and child abuse. The principle function of pediatric care is no longer limited in facility-based treatment of diseases, but also including continuous preventive measures targeting general population and home-based care targeting children with life-long morbidities at the community. Both are expected to respond to individualized needs, by active involvements into community and education and close collaboration with various stakeholders. The outcomes of child health care are not limited in clinical and health indicators such as survival rate, cure rate and health related quality of life, but also various aspects other than health, such as education, well-being of children and their primary caregivers, especially when treatment of diseases is no longer the dominant role of health care. A comprehensive support to child-rearing by integrating various child care professionals at the community tends to have an impact in long-term, rather than short-term, as establishment of healthy behaviors in childhood is expected to contribute to healthy life in adulthood. For example of childhood obesity, several studies have reported that it is associated with unhealthy status in future life (19-21). Consequently, related interventions in childhood would bring potential benefits in adulthood. However, it is rather difficult to find out positive evidence for the significance to observe the difference in mortality and health-related quality-of-life before/after, or with/without such the interventions in short-term among the general population. Another concern in the evaluation raises from the fact that the expected outcomes of a long-term care for children with disabilities and chronic diseases are more likely to be the improved well-being of patients and their primary caregivers, but not merely improved typical clinical outcomes, as such health conditions is not curable but needing intensive medical and social welfare services. The related interventions seldom have the effect on cost saving. In particular, productivity loss, burdens due to home-based nursing care and well-being of caregivers have been omitted in the current outcome evaluation. In this regarding, the current standardized measurement of health outcomes in CEA, may have a limited capacity to appropriately generate these all aspects and methodologies used for child health care needs to be refined (22). With respect to the unique challenges in generation of value-based evidence for child health care, the evaluation should reflect the impacts of the integrated approach in a long-term scope.
Conclusions
In Japan, child health care has been involved in an unprecedented transformation of health sector and society. The value of child health care needs to be comprehensively evaluated with respect to guide financing and reform of the pediatric care and its quality improvement. Child-friendly instruments and methodologies to comprehensively reflect the value of child health care is urgently necessary to be refined, as a supplement to the current methodology scheme of HTA.
Acknowledgements
Funding: This study is granted by Health and Labor Sciences Research Fund (No. 28171101), Japan Society of the Promotion of Sciences (17K19948), Ministry of Health, Labor and Welfare (No. 24).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- The Central Social Insurance Medical Council. About the pilot introduction of cost-effectiveness evaluation [cited 2017 Jan 21]. Available online: http://www.mhlw.go.jp/file/05-Shingikai-12404000-Hokenkyoku-Iryouka/0000107178.pdf
- Prime Minister of Japan and His Cabinet. The Japan’s Plan for Dynamic Engagement of All Citizens [cited 2018 Jan 21]. Available online: https://www.kantei.go.jp/jp/singi/ichiokusoukatsuyaku/pdf/plan2.pdf
- Cabinet Office, government of Japan. Children and Youth White Paper 2015 [cited 2018 Jan 21]. Available online: http://www8.cao.go.jp/youth/whitepaper/h27honpen/b1_03_03.html
- Ministry of Health, Labor and Welfare. Vital Statistics 2016 [cited 2018 Jan 21]. Available online: http://www.mhlw.go.jp/toukei/saikin/hw/jinkou/geppo/nengai16/dl/h7.pdf
- Ishiwada N, Hishiki H, Nagasawa K, et al. The incidence of pediatric invasive Haemophilus influenza and pneumococcal disease in Chiba prefecture, Japan before and after the introduction of conjugate vaccines. Vaccine 2014;32:5425-31. [Crossref] [PubMed]
- Ishii N, Kono Y, Yonemoto N, et al. Outcomes of infants born at 22 and 23 weeks’ gestation. Pediatrics 2013;132:62-71. [Crossref] [PubMed]
- Niwa K. Adults with congenital heart disease transition. Curr Opin Pediatr 2015;27:576-80. [Crossref] [PubMed]
- Mori R, Eya Y, Ehara A, et al. Survey Report on pediatric provision system Nihon Shoni Kagakukai Zasshi 2015;119:1551-66. (in Japanese).
- Tahara T, Ishitani N. Transition medicine from pediatric to adult care (in Japanese). Nakayama Shoten Press, Tokyo, 2015.
- Japan Pediatric Society. Educational goals for the pediatrician Nihon Shoni Kagakukai Zasshi 2015;119:751-98. (in Japanese).
- Ministry of Health, Labor and Welfare. Summary of survey to clinicians, dentists and pharmacists in 2014 [cited 2018 Jan 21]. Available online: http://www.mhlw.go.jp/toukei/saikin/hw/ishi/14/
- Ministry of Health, Labor and Welfare, Japan. Summary of the revision of medical treatment fees for 2016 [cited 2018 Jan 21]. Available online: http://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000112857.html
- Ishida Y, Ohde S, Takahashi O, et al. Factors affecting health care utilization for children in Japan. Pediatrics 2012;129:e113-9. [Crossref] [PubMed]
- Ebara A. Out-of-pocket payment of medical costs among children aged 0 to 4 years Nichii Zasshi 2008;137:1492-5. (in Japanese).
- Non-Profit Organization for Vaccine Preventable Diseases. Information for subsidies to children’s vaccination [cited 2018 Jan 21]. Available online: https://www.know-vpd.jp/d_josei_list.php
- Drummond MF, Sculpher MJ, Claxton K, et al. Methods for the economic evaluation of health care programmes. 4th edition. Oxford: Oxford University Press, 2015.
- Shiroiwa T, Fukuda T, Ikeda S, et al. Development of an Official Guideline for the Economic Evaluation of Drugs/Medical Devices in Japan. Value Health 2017;20:372-8. [Crossref] [PubMed]
- Ungar WJ. Economic evaluation in child health. Oxford: Oxford University Press, 2015.
- Llewellyn A, Simmonds M, Owen CG, et al. Childhood obesity as a predictor of morbiditiy in adulthood: a systematic review and meta-analysis. Obes Rev 2016;17:56-67. [Crossref] [PubMed]
- Silverwood RJ, Pierce M, Thomas C, et al. Association between younger age when first overweight and increased risk for CKD. J Am Soc Nephrol 2013;24:813-21. [Crossref] [PubMed]
- Kuwahara E, Murakami Y, Okamura T, et al. Increased childhood BMI is associated with young adult serum uric acid levels: a linkage study from Japan. Pediatr Res 2017;81:293-8. [Crossref] [PubMed]
- Ungar WJ. Challenges in health state valuation in pediatric economic evaluation. Pharmacoeconomics 2011;29:641-52. [Crossref] [PubMed]