Metabolomics: a challenge for detecting and monitoring inborn errors of metabolism
Introduction
The term ‘inborn errors of metabolism’ (IEMs) was firstly coined in 1908 by Sir Archibald E. Garrod, a British physician, who observed patients with four genetically determined diseases: alkaptonuria, albinism, cystinuria, and pentosuria (1). He postulated that this cohort of a lifelong duration inherited conditions was caused by diminished activity or complete lack of a given enzyme which may either induce defects or block specific metabolic pathways. Notably, Garrod launched the very novel notion of ‘chemical individuality’, thus providing the background for a pioneering vision of system biology (2). His peculiar view translated human chemical individuality in a setting of heredity and dynamic metabolism, that currently means interplay between genetics, epigenetics, proteomics and metabolomics. Garrod hypothesized that each single enzyme is controlled by a single gene; curiously, the notion that enzymes are protein was unknown among scientists at that time. The relevance of Garrod’s ideas was underrated for many decades. First, the practice of medicine in Garrod’s lifetime could not considerably benefit from the discovery of congenital and inheritance nature of these diseases. Then, the apparent rarity of IEMs promoted medical profession to consider them as “clinically irrelevant”. Nowadays, based on the definition of rare disease (3), the estimated prevalence of IEMs is individually rare; however, the overall IEMs prevalence corresponds to about 1 of every 1,000 people (4). Geneticists also had a limited awareness on Mendelian’s principles, as well as on the physical nature of Mendel’s factors, namely genes. Probably, the most important obstacle for the pervasive diffusion of Garrod’s theory was the dominant influence of Biometricians, who were conducting a battle against Mendelians (5). In the second edition of Inborn Errors of Metabolism, published by Garrod in 1923, he reported two further inborn errors: congenital porphyrinuria and congenital steatorrhea (6). From that time on, hundreds of IEMs have been discovered and continue to be discovered. Currently, 1015 well-characterized IEMs, causing alterations in specific metabolic pathways, have been described in the literature (7); additional 111 supposed less well-characterized conditions that might be classified as IEMs do not meet strict criteria for inclusion in the current nosology (7). IEMs represent around 80% of rare (orphan) diseases, although their prevalence is highly variable, ranging from 25:100,000 for congenital hypothyroidism to 0.4:100,000 for disorders like branched chain ketoaciduria. Most IEMs consist of enzymes and transport proteins defects, leading to either inadequate production of critical substances (high-energy metabolite intermediates, hormones, proteins, lipids, metabolites, and so on) or undue accumulation of toxic metabolites. Due to their considerable heterogeneity, IEMs can be categorized by several criteria. Indeed, various informal systems of classification are available in the literature, based on clinical features, pathophysiology, affected enzymes, affected organelle and many other criteria. Nevertheless, no unique, universal classification system still exists. The Society for the Study of Inborn Errors of Metabolism (SSIEMs) has grouped IEMs according to the principle of homogeneity. Each group consists of diseases belonging to the same biochemical pathway, detected by the same diagnostic method, and treated by equivalent emergency protocol standards as well as by similar long-term management (8). A recent classification divides IEMS into two large clinical categories: (I) IEMs either involving only one functional system, or affecting only one organ; (II) IEMs characterized by biochemical impairments either affecting one metabolic pathway common to a large number of cells/organs, or restricted to one organ but giving rise to systemic disorders (9). The latter has been further categorized into three groups: disorders of intermediary metabolism affecting small molecules, disorders involving primarily energy metabolism, and disorders involving complex molecules (Table 1).
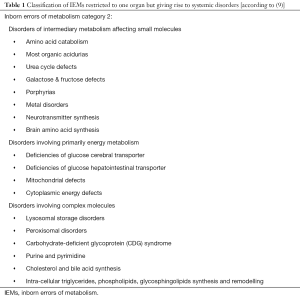
Full table
Laboratory screening of IEMs
In most developed nations, and in several low-income countries, each newborn is screened for IEMs by dry blood spot (DBS) testing. Timely newborn screening and genetic profiling are crucial in early recognition and treatment of IEMs. Diagnostic delay may result in acute metabolic decompensation, progressive neurologic injury, or death. The laboratory approach for screening IEMs can be schematically represented by four steps: (I) general metabolic screening test; (II) specific metabolite assays; (III) enzymes studies; (IV) DNA analysis. From their introduction in public health care, newborn screening programs have been expanded to include now more than 50 inherited metabolic disorders, including aminoacidopathies, organic acidemias, fatty acid oxidation disorders, and lysosomal storage disorders. The definitive diagnosis is based on more specialized tests such as plasma amino acid profiling, urine organic acid profiling, plasma acylcarnitine profiling, free fatty acid profiling, pyruvate, acetoacetate, 3-hydroxybutyrate, mucopolysaccharides, oligosaccharides, enzyme activity assays, functional assays, and mutational analyses. In 1980s, tandem mass spectrometry (MS/MS) was introduced as a reference technique for newborn screening, because of its capacity of screening a wide range of previously unscreened IEMs by a single test performed on a DBS. Currently, MS/MS techniques are routinely used for neonatal screening of IEMs, since they are rapid, highly sensitive and specific, requiring very low sample volume and offering a high throughput. As a priority objective of a Regional Genetics Collaborative project funded by the U.S. Health Resource and Service Administration (HRSA), in 2004 a collaborative project was launched, called Region 4 Stork (R4S). The main goals were facilitating universal implementation of newborn screening by MS/MS and confirmatory testing of newborns for IEMs, and improving laboratory quality of expanded newborn screening (10). The project was also aimed to reach three more objectives: (I) achieving uniformity of testing panels by MS/MS, thus maximizing the detection rate of affected newborns; (II) improving cumulative analytical performance; and (III) achieving and maintaining the lowest achievable rates of false positive and false negative results (11). The catalyst of this project is a multivariate pattern recognition software [Collaborative Laboratory Integrated Reports (CLIR)], which can significantly improve post-analytical interpretation of complex metabolic profiles (12). This has led to identification of 114 biomarkers, to be used in the newborn screening (13). In 2012, the R4S database became part of the Newborn Screening Translational Research Network, an initiative funded by the National Institute of Child Health and Human Development (NICHD).
Metabolomics, metabolites and metabolome
Metabolomics and metabolism share as their root the ancient Greek word “metabol”, which means “change”. The term metabolomics, defining the comprehensive analysis of small molecules involved in metabolic pathways of living organisms, was coined by Oliver Fiehn in 2002 (14). By using high throughput technologies, metabolomics allows identification and measurement of metabolites recognizable in a given biological sample. The term metabonomics was previously introduced to define the dynamic metabolic response of living systems to perturbations over time, mapped by appropriate analytical and statistical techniques (15). Nevertheless, a large degree of overlap in the way metabolomics and metabonomics have been used in the literature has led to their almost complete interchangeability, being analytical and modeling procedures identical (16). Metabolites refer to all the organic small molecules with a molecular weight <1,800–1,500 Dalton. These can act as substrates or products in biochemical metabolic pathways (17). Metabolites such as lipids, sugars, and amino acids are byproducts of cellular metabolism and control the way a cell transfers energy to, or communicates with, other cells. Indeed, metabolites show abrupt changes in their amount and composition within a biological system in response to either physiopathological perturbations or therapeutic treatments. Thus, they can generate vital information in patients care by unveiling alterations in biochemical pathways involved in diseases and/or in drug administration. Metabolomics can be considered one of the earliest medical and biological sciences. In ancient Greece, urine sweetness, an organoleptic feature due to excretion of metabolites into urine, was used to detect glycosuria in diabetes. Most of currently available clinical laboratory tests consist of measurement of blood and urine metabolites concentration (e.g., uric acid, glucose, creatinine, and so forth). However, this conventional approach is mainly hypothesis-driven and reductionist. Notably, it allows neither complete characterization of a biological system, nor systemic analysis of complex functional interrelationships between metabolites. Conversely, metabolomics offers a ‘top-down’ integrated view of biochemistry in complex organisms. This marks a basic difference between the current evaluation of single metabolites and the analysis of the whole set of metabolites recognizable in a biofluid, cell or tissue extract, namely the metabolic profile. The latter depicts an accurate view of the highly dynamic metabolic network, offering a plethora of biochemical data that can be analyzed and interpreted, and demonstrating the assumption that ‘the whole is more than the merely sum of parts’, as stated by Aristotle more than two thousand years ago (18). In 1998, Oliver et al. coined the word metabolome to define the holistic quantitative amount of metabolites in a given sample (19). Later, the definition has been adjusted as the molecular phenotype originating from the genotype’s interaction with the environment (20). The metabolome represents the molecular fingerprint of a biofluid or a tissue, and is highly dynamic. Changes in metabolites composition, concentration and interactions depend on complex interplay with different organs, environment and gut microbiota. Although the term environment embraces a wide spectrum of definitions, it can be argued that environment addresses all non-genetic factors influencing the homeostasis of reaction chains in metabolic pathways.
Metabolome profiling methods
The human metabolome shows a very high degree of complexity, requiring specific and more complex analytical platforms, methods and data analysis compared with those used for other “-omics”. Indeed, genomics, transcriptomics and proteomics can profile large molecules made of chemical building blocks, namely nucleotides and amino acids, constituted by a simple and limited set of subunits (4 and 20 for nucleic acids and proteins, respectively). Thus, the order combination of nucleotides or amino acids is what matters for identification and functional analysis of DNA, RNAs and proteins. In other words, the complexity of DNA, RNAs and proteins, closely related with the corresponding biological information, is the order of subunits. Conversely, no sequencing approach can be used for the analysis of metabolites in a complex biofluid or tissue, because no obvious order exists. Metabolites should be individually and selectively differentiated, identified, and quantified across a wide quantitative and qualitative chemical space (21). In addition, metabolites either individually or clustered in groups, can differ from each other for physicochemical properties. This high variability adds another layer of complexity to metabolomics. Nuclear magnetic resonance (NMR) spectroscopy and MS are reference methods for extracting comprehensive and unbiased chemical information from complex mixtures of metabolites. NMR spectroscopy measures an intrinsic magnetic property of atomic nuclei, namely the spin (22). One dimensional proton NMR (1H NMR) spectroscopy is the most common NMR approach in metabolomics. NMR has several advantages (23), the most important is the absence of any preanalytical step, which means avoiding sample manipulation, potential destruction of metabolites structure and reduction of interferences due to the co-migration of metabolites with compounds previously used for sample preparation. Further advantages consist of rapid analytical time, wide coverage of chemical classes, and high reproducibility. MS is very popular across metabolomic studies, being less expensive than NMR and highly sensitive for characterizing complex molecular phenotypes. Two main approaches are used in MS-based methods, (I) the direct infusion mode, consisting of the direct injection of biological samples into the ionization source of the mass spectrometer, and (II) MS in conjunction with high resolution separation techniques such as liquid chromatography (LC-MS), gas chromatography (GC-MS) and capillary electrophoresis (CE-MS). These preventive separation methods reduce the complexity of mass spectra, providing additional information about physicochemical properties of metabolites. The direct infusion mode has the advantage to be very helpful for quantifying metabolites in complex mixtures. Nevertheless, it can induce an extensive ion suppression, causing inability to separate isobaric and isomeric compounds (24). Currently, LC-MS is the most widely applied platform for targeted profiling of both polar and non-polar compounds, CE-MS is useful for analysis of polar charged metabolites, whilst GC-MS is helpful for analysis of volatile metabolites, as well as those made volatile by chemical derivatization (25). The introduction of ultra performance liquid chromatography (UPLC) and supercritical fluid chromatography (SFC) coupled with MS has improved both sample throughput and analytical sensitivity. In particular, the adoption of these techniques leads to a high-resolution separation of lipids, which constitute a large subset of the metabolome and should be carefully analyzed in many IEMs. Due to large differences in abundance and huge diversity of chemical structures, there is a growing trend in metabolomics to perform tandem studies, in which the same sample is analyzed by both NMR and MS (26). Indeed, no single available technology can definitively characterize the whole metabolome in a given biological sample (27).
Metabolomics for IEMs
With the increasing expansion of metabolomics in clinical biochemistry and laboratory medicine communities, several research groups have focused their interest on the application of metabolomics for diagnosing and monitoring IEMs, pursuing a deepened analysis of metabolites and their interconnections. Despite its unquestionable clinical value and its primary role in public health care, newborn screening offers only a snapshot of a very small subset of metabolic alterations; moreover, a number of IEMs are not identifiable by routine newborn screening programs. On the other hand, the metabolic profiling could significantly contribute to extend metabolic information with two main goals: achieving an accurate diagnosis for the individual patient, and discovering novel IEMs (28-30). However, genetics and metabolomics are not mutually exclusive. For each metabolic gene a new computational approach can be developed for predicting a set of metabolites whose concentration is predicted to change after gene knockout in urine, blood and other biological fluids (31). Structural and functional information on 247 metabolites associated with 147 IEMs and 202 metabolic pathways involved in various IEMs are reported in the human metabolome data base (HMDB). This tool was launched in 2005 by a multi-institutional, multi-national project (Human Metabolome Project) (32), and was designed to facilitate the investigation of links connecting genes, diseases and metabolites (33). HMDB is basic for elucidating the metabolic pathways disturbed, or blocked, in a given IEMs and for facilitating discovery, identification and quantification of key metabolites in patients with IEMs. Over the last decade, a growing number of metabolomic studies focused on IEMs have been published, with a special interest for those diseases displaying marked phenotypic and genotypic variability among affected patients, and therefore hard to diagnose by newborn screening programs. A paradigmatic example is Fabry disease, an X-linked complex, multisystemic lysosomal storage disorder caused by a deficiency of the enzyme α-galactosidase A and characterized by accumulation of globotriaosylsphingosine (lyso-Gb3) and globotriaosylceramide (Gb3) in biological fluids and tissues. By using an UPLC electrospray ionization time-of-flight (UPLC-ESI-TOF-MS)-based metabolomic approach, a Canadian researcher group aimed to find novel biomarkers reflecting disease severity and progression. In a sequence of consecutive studies, they found up to 15 different isoform/analogs of Gb3 (34-37) and 22 galabiosylceramide (Ga2) isoforms/analogs of Ga2 in urine of untreated Fabry patients (38). The discovery of these isoforms contributed to provide new insights into the pathophysiology of Fabry disease and into mechanisms inducing alterations in metabolic pathways.
Metabolomic studies can be conducted following two strategies, i.e., the targeted and the untargeted approach. In studies using the targeted approach, specific metabolites are detected, quantified and compared to establish reference ranges. The untargeted approach consists of analysis of all detectable metabolites known and unknown in a single test performed on a biological fluid or tissue, to determine any perturbation of single or multiple metabolites and of related biochemical pathways (39). Untargeted metabolomics can be considered a ‘discovery mode’ process. Both targeted and untargeted MS-based metabolomic approaches have been used to expand the range of disease-associate metabolites (40).
The targeted metabolomic approach
The quantitative targeted metabolomics in combination with chemometrics have been applied in several studies on IEMs for clinical validation of known diagnostic biomarkers. Aminoacidopathies, organic acidurias and fatty acid oxidation disorders were investigated by using the targeted metabolomic approach (30). A recent study evaluated an LC-MS/MS-based comprehensive targeted metabolic panel of 220 clinically relevant metabolites, encompassing a broad range of genetic metabolic disorders (41). The evaluation was made on animal tissue samples, on 20 healthy adults volunteers and on 56 DBS samples from patients with eight different IEMs. Results showed that the targeted panel is sensitive, robust and potentially useful as a screening tool for a large group of IEMs, thus avoiding multiple, time-consuming and expensive biochemical assays which would cause delay in clinical management. By analyzing 163 plasma metabolites in 50 controls and 34 patients with defects in amino acid metabolism, organic acidurias and mitochondrial defects, this combination has led to detecting all patients with inherited metabolic disorders, with complete discrimination for each patient sample from control samples (42). A targeted metabolomics approach was used to test whether specific plasma sphingolipids are useful as outcome measures in Niemann-Pick C1 (NPC1) disease therapies (43). As widely known, aberrant sphingolipid metabolism is the metabolic hallmark of NPC1 disease. By using a MS-based metabolomic profile, researchers identified a panel of plasma and cerebrospinal fluid (CSF) sphingolipids that were increased in human NPC1 subjects and, even more relevant, that responded to therapeutic treatment both in patients and in animal models.
The untargeted metabolomic approach
The untargeted approach is highly descriptive. A single metabolomic analysis provides a plethora of information currently requiring multiple targeted panel assays for organic acids, carnitine biosynthesis intermediates, acylcarnitines, nucleic acids, amino acids and other metabolites. The application of untargeted metabolomics to the diagnosis of metabolic diseases was early conducted for characterizing methylmalonic acidemia and propionic acidemia (44). The study demonstrated that the simultaneous profiling and detection of hundreds to thousands metabolites increases the likelihood of identifying new compounds associated with these diseases, such as five additional acyl-carnitine metabolites and γ-butyrobetaine. The study represents a cornerstone supporting the notion that untargeted approach enhances the identification of new biomarkers in known disorders (44). More recently, 120 plasma samples from patients with a confirmed IEM and 70 from patients tested for IEMs but with normal results were analyzed by using an untargeted metabolomic workflow based on three separate MS platforms run in parallel (GC-MS, LC-MS in positive ion mode and LC-MS in negative ion mode) (45). Based on pathway analysis, the authors successfully screened 20 of 21 IEMs, whilst homocysteine, methylmalonic acid, tetradecenoylcarnitine (C14:1), and guanidinoacetate (GAA) were not identified. This limitation was counterbalanced by the identification of multiple metabolite perturbations associated with homocystinuria and methylmalonic acidemia, thus confirming the usefulness of untargeted approach for IEMs screening when patient’s phenotype is undifferentiated. An untargeted approach combining 1H NMR spectroscopy and LC-MS/MS allowed elucidating the metabolic abnormalities and pathogenesis of Barth syndrome, a rare X-linked disorder consisting of deficiency in tafazzin expression and leading to abnormal cardiolipin content and reduction of mature cardiolipin (46). All metabolites detected by MS displayed a clear separation between samples from patients with Barth syndrome and controls. Interestingly, the pathway enrichment analysis showed the association between broad, previously unknown, metabolic impairments with etiology of Barth syndrome, thus revealing new potential therapeutic targets. Untargeted metabolomics has been applied to investigate plasma metabolome in 12 patients with long-chain hydroxy-acyl-CoA dehydrogenase and carnitine palmitoyltransferase 2 deficiency as well as in 11 healthy controls (47). Overall, 832 metabolites were detected. When results were analyzed following the metabolic profile of complex lipids (model 2), partial least squares-discriminant analysis (PLS-DA) score plot revealed 117 non-acylcarnitine variables discriminating controls from individuals with mitochondrial fatty acid oxidation disorders. This analysis had the potential to recognize the risk and severity of disease, as well as the identification of fatty acid oxidation disease subtypes. Finally, the untargeted global metabolic phenotyping was successfully tested in the CSF of a pediatric cohort with various IEMs (48). More than 60% of metabolites detected in CSF were simultaneously present in blood and urine, thus suggesting that a single CSF sample processed with an integrated metabolomic workflow can be used to identify a large breadth of biochemicals useful for identifying altered metabolic pathways associated with IEMs.
Metabolomics applied to the screening of IEMs
The potential role of metabolomics for IEMs screening was firstly explored on two inherited metabolic disorders, i.e., phenylketonuria and maple syrup urine disease (49). For the latter, characterized by increased levels of branched-chain amino acids, no screening was available at that time. DBS were collected and analyzed by 1H NMR spectroscopy. Metabolomics clearly discriminated not only the metabolome of samples from healthy children from that of children with maple syrup urine disease, but also represented a specific metabolic screening for this disease, allowing to discriminate phenylketonuria from maple syrup urine disease (49). In a study enrolling six patients with six distinct IEMs (argininosuccinic aciduria, classic homocystinuria, classic methylmalonic acidemia, maple syrup urine disease, phenylketonuria and type II tyrosinemia) and six controls, urine metabolome was explored by combining desorption electrospray ionization mass spectrometry (DESI-MS) with 1H NMR spectroscopy (50). This combination clearly discriminated the urine metabolic profile of each patient from that of remaining patients and from that of controls, thus offering a rapid and accurate screening of urine from diseased patients for a better characterization of IEMs. With the aim to reduce the false positive rate of traditional electrospray MS/MS newborn screening, a group of researchers proposed to introduce a novel approach based on direct flow injection analysis, namely nanospray ionization in conjunction with high-resolution MS (HR MS) (51). The metabolic profile of DBS was mapped, resulting in selective detection of more than 400 individual metabolites, including complex lipids, bile acids, organic acids, fatty acids, carbohydrates, acylcarnitines. Importantly, this strategy had the ability to screen galactosemia by detecting hexose and hexose-phosphate, as well as many other diseases involving global changes in metabolome. Expanded newborn screening for preclinical diagnosis of IEMs by using LC-MS/MS targeted metabolomics was included in a research project carried out in southern Italy, between 2007 and 2014 (52). The study was focused on the identification of newborns at risk for fatal diseases, including fatty acid oxidation disorders, organic acidemia, branched chain amino acid deficiency, hyperammonemia, and maternal acquired metabolic disorders. Results supported the important added value of metabolomics for improving prediction of clinical risk by a presymptomatic diagnosis of IEMs. Recently, a quantitative/qualitative HR MS platform tailored to metabolic disease was developed and validated, with the aim to detecting and quantifying many classes of both polar and non-polar/hydrophobic metabolites (53). This platform covers a multitude of various metabolites, including those commonly quantified by combining separate analytical instruments. A multi-center 1H NMR spectroscopy-based clinical study aimed to assess analytical variability on 20 metabolites always detectable in neonatal urine along with 45 pathological metabolites. Results from healthy newborns were embodied into a NMR database (54). The protocol involved 14 clinical centers, with collection of 989 urine samples from newborns aged 24 to 168 hours after birth. Nearly all samples (89.5%) were measured twice in two different laboratories. Reference ranges were established for 20 metabolites. The spectra of healthy neonates were characterized; statistical outliers were identified, and the urine spectra of diseased newborns were acknowledged and stored.
Urine sample for metabolomics: benefits and pitfalls
Urine is an ideal biological fluid for metabolomics in neonatology, since is sterile, easy to obtain in large volumes and minimally invasive. More importantly, the characterization of urine metabolome significantly contributes to identify biochemical signatures of cellular metabolism involved in many IEMs (55). The high reliability of urine samples for metabolomics applied to diagnosis and monitoring of IEMs was demonstrated in a recent study, performed on a sample consisting of 18 different IEMs, including 34 from subjects diagnosed with an IEM and 66 from those without a final diagnosis of IEM (56). Over 1,200 metabolites were detected. Moreover, biochemical signatures for 16 IEMs were unequivocally identified, while X-linked creatine transporter deficiency and ornithine transcarbamylase were not. However, the two patients with the two unidentified diseases were under therapeutic treatment, which may mask disease-specific biomarkers signature. The GC-MS-based urine metabolic profile for IEMs newborn screening was investigated in a retrospective study on 23,140 urine samples in an Indian setting (57). The study showed that GC-MS metabolomic approach significantly improved the effectiveness of neonatal screening programs in that Country, whilst also appeared more comprehensive for screening metabolic defects, easier and non-invasive. Beyond primary lactic acidemia, organic acidemia, and aminoacidopathies, GC-MS-based metabolomics revealed alkaptonuria, canavan disease, and 4-hydroxybutyric aciduria. Although highly advantageous, urine analysis may be biased by lack of standardization of preanalytical phase. In particular, sample collection and urea removal protocol are crucial steps for GC-MS analysis. They may both generate potential interferences in metabolomic studies. Most methods for urine collection (e.g., midstream specimens, clean catch specimens, urine collection bags, suprapubic catheter) are infeasible in the neonatal age; one popular method for collecting urine from babies is disposable diapers. Once the production and sale of ultra-absorbent diapers commenced, it became impossible to collect urine samples directly from the diaper itself. To overcome this problem, a cotton ball or a cotton pad were inserted into the disposable diaper, and the so-called ‘diaper plus cotton ball’ was introduced into practice (58). In such way, urine can be absorbed by the cotton. Unfortunately, the ‘diaper plus cotton ball’ technique may be a source of sample contamination. An experimental study examined eight diaper brands, observing that each diaper brand had a unique contaminant profile or signature, which could potentially interfere with results obtained both by NMR- and LC/MS-based metabolomics approaches (59). Authors recommended the metabolic characterization of the ‘diaper and cotton ball’ brand used in a given study prior to initiating the evaluation of urine metabolome. They also strongly discouraged the use of multiple diaper brands in a metabolomics study. Following this recommendation it is possible to evaluate whether or not contaminant profiles are minimal or manageable. Several additional factors should carefully be taken into account before analyzing results, since these factors could significantly influence extent and metabolic profile of a diaper contaminants, such as temperature, urine pH and osmolality, length of time that urine is exposed to diaper before collection, bacterial contamination and baby weight. Urine analyzed by GC-MS should be pre-treated by urease to remove the significant urea amount, since this metabolite may interfere with chemical derivatization, thus leading to incomplete chemical transformation. The lack of standardization of this step, namely unbalanced combination between volume of enzyme (urease) added to the sample with the sonication time, can lead to incomplete urea removal and thus to chromatographic column overloading, peak distortions, and likelihood of co-eluting metabolites peaks. A very recent study established a standardized protocol for urea removal, obtaining the optimal combination between urease volume and sonication time (60).
Future perspectives
Although IEMs are disorders genetically transmitted, typically in an autosomal recessive or X-linked recessive fashion (e.g., Duchenne muscular dystrophy), the model ‘one gene-one enzyme-one disease’ can no longer be considered appropriate. Indeed, the genome alone may turn out to be inadequate to explain the complexity of human metabolic diseases (61). On the other hand, metabolites derive from intermediate biological processes that bridge gene function, non-genetic factors, and phenotypic end points (62). Therefore, metabolic phenotypes can provide novel insights into gene function, biomarkers for diagnosis and prognostication, and mechanisms of disease pathogenesis. Metabolomics offers the opportunity to map metabolic pathways disturbances, as well as the network of metabolites involved in the origin of a metabolic disease (63,64). Actually, the best approach to metabolomic study of complex IEMs may be the combination between untargeted approach, which means to span the breadth of metabolome and perform pathways analysis, with targeted approach, which means measuring specific metabolites and assessing their reference intervals. This strategy, adopted in several studies (65-67), facilitates the identification of subtle phenotypes and biomarkers correlated with a specific phenotype. The integration of genomic with metabolomics data represents the current challenge for improving diagnosis and prognostication of IEMs. The goals here are identifying both metabolically active loci and genes relevant to a disease phenotype, thus deriving disease-specific biological insights (68). For example, the definitive diagnosis of maple syrup urine disease should be based at least on: (I) identification of pathogenic variants in either DBT [encoding dihydrolipoyl transacylase (E2) subunit], BCKDHB [encoding BCKA decarboxylase (E1) β-subunit] or BCKDHA [encoding BCKA decarboxylase (E1) α-subunit] genes; (II) measurement of high levels of alloisoleucine, isoleucine, leucine, valine; (III) detection of branched-chain 2-oxo acids (69). In the so-called pathway-based approach, genes in enriched metabolic pathways harbor variants that elucidate the patient’s biochemical phenotype (70). In conclusion, MS-based metabolomics is currently used in many published studies on IEMs (71). Concomitantly, most clinical laboratories have included MS in their technical equipment over the past 5 years. Therefore, there is no barrier to introducing metabolomics into clinical practice for expanding newborn screening programs.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Garrod AE. Inborn errors of metabolism. In: June 1908: The Croonian Lectures Delivered Before the Royal College of Physicians of London. London (UK): Oxford University Press, 1909.
- Gahl WA. Chemical individuality: Concept and outlook. J Inherit Metab Dis 2008;31:630-40. [Crossref] [PubMed]
- Richter T, Nestler-Parr S, Babela R, et al. Rare Disease Terminology and Definitions-A Systematic Global Review: Report of the ISPOR Rare Disease Special Interest Group. Value Health 2015;18:906-14. [Crossref] [PubMed]
- Stanton BF. New Understanding of Mechanisms and New Hope for Treatments. Pediatr Clin North Am 2018;65:xvii-xviii. [Crossref] [PubMed]
- Olby R. The Dimensions of Scientific Controversy: The Biometric-Mendelian Debat. Br J Hist Sci 1989;22:299-320. [Crossref] [PubMed]
- Garrod AE. Inborn Errors of Metabolism. 2nd Edition. London (UK): Oxford University Press, 1923.
- Ferreira CR, van Karnebeek CDM, Vockley J, et al. A proposed nosology of inborn errors of metabolism. Genet Med 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Zschocke, J. SSIEM Classification of Inborn Errors of Metabolism. In: Blau N, Duran M, Gibson KM, et al. editors. Physician’s Guide to the Diagnosis, Treatment, and Follow-up of Inherited Metabolic Diseases. Berlin Heidelberg (GE): Springer-Verlag, 2014:817-30.
- Saudubray JM, Garcia-Cazorla A. Inborn Errors of Metabolism Overview: Pathophysiology, Manifestations, Evaluation, and Management. Pediatr Clin North Am 2018;65:179-208. [Crossref] [PubMed]
- American College of Medical Genetics Newborn Screening Expert Group. Newborn screening: toward a uniform screening panel and system - executive summary. Pediatrics 2006;117:S296-307. [Crossref] [PubMed]
- McHugh D, Cameron CA, Abdenur JE, et al. Clinical validation of cutoff target ranges in newborn screening of metabolic disorders by tandem mass spectrometry: a worldwide collaborative project. Genet Med 2011;13:230-54. [Crossref] [PubMed]
- Hall PL, Marquardt G, McHugh DM, et al. Postanalytical tools improve performance of newborn screening by tandem mass spectrometry. Genet Med 2014;16:889-95. [Crossref] [PubMed]
- Marquardt G, Currier R, McHugh DM, et al. Enhanced interpretation of newborn screening results without analyte cutoff values. Genet Med 2012;14:648-55. [Crossref] [PubMed]
- Fiehn O. Metabolomics - the link between genotypes and phenotypes. Plant Mol Biol 2002;48:155-71. [Crossref] [PubMed]
- Nicholson JK, Holmes E, Kinross JM, et al. Metabolic phenotyping in clinical and surgical environments. Nature 2012;491:384-92. [Crossref] [PubMed]
- Nicholson JK, Lindon JC, Holmes E. 'Metabonomics': understanding the metabolic responses of living systems to pathophysiological stimuli via multivariate statistical analysis of biological NMR spectroscopic data. Xenobiotica 1999;29:1181-9. [Crossref] [PubMed]
- Lazar MA, Birnbaum MJ. Physiology. De-meaning of metabolism. Science 2012;336:1651-2. [Crossref] [PubMed]
- Scriver CR, Water PJ. Monogenic traits are not simple: lessons from phenylketonuria. Trends Genet 1999;15:267-72. [Crossref] [PubMed]
- Oliver SG, Winson MK, Kell DB, et al. Systematic functional analysis of the yeast genome. Trends Biotechnol 1998;16:373-8. [Crossref] [PubMed]
- Kell DB, Oliver SG. The metabolome 18 years on: a concept comes of age. Metabolomics 2016;12:148. [Crossref] [PubMed]
- Reymond JL, Ruddigkeit L, Blum I, et al. The enumeration of chemical space. WIREs Comput Mol Sci 2012;2:717-33. [Crossref]
- Beckonert O, Keun HC, Ebbels TM, et al. Metabolic profiling, metabolomic and metabonomic procedures for NMR spectroscopy of urine, plasma, serum and tissue extracts. Nat Protoc 2007;2:2692-703. [Crossref] [PubMed]
- Markley JL, Brüschweiler R, Edison AS, et al. The future of NMR-based metabolomics. Curr Opin Biotechnol 2017;43:34-40. [Crossref] [PubMed]
- González-Domínguez R, Sayago A, Fernández-Recamales Á. Direct infusion mass spectrometry for metabolomic phenotyping of diseases. Bioanalysis 2017;9:131-48. [Crossref] [PubMed]
- Begou O, Gika HG, Wilson ID, et al. Hyphenated MS-based targeted approaches in metabolomics. Analyst 2017;142:3079-100. [Crossref] [PubMed]
- Gonzalez-Dominguez A, Duran-Guerrero E, Fernandez-Recamales A, et al. An Overview on the Importance of Combining Complementary Analytical Platforms in Metabolomic Research. Curr Top Med Chem 2017;17:3289-95. [Crossref] [PubMed]
- Riekeberg E, Powers R. New frontiers in metabolomics: from measurement to insight. F1000Res 2017;6:1148. [Crossref] [PubMed]
- Moolenaar SH, Engelke UF, Wevers RA. Proton nuclear magnetic resonance spectroscopy of body fluids in the field of inborn errors of metabolism. Ann Clin Biochem 2003;40:16-24. [Crossref] [PubMed]
- Tebani A, Abily-Donval L, Afonso C, et al. Clinical Metabolomics: The New Metabolic Window for Inborn Errors of Metabolism Investigations in the Post-Genomic Era. Int J Mol Sci 2016;17. [Crossref] [PubMed]
- Sandlers Y. The future perspective: metabolomics in laboratory medicine for inborn errors of metabolism. Transl Res 2017;189:65-75. [Crossref] [PubMed]
- Shlomi T, Cabili MN, Ruppin E. Predicting metabolic biomarkers of human inborn errors of metabolism. Mol Syst Biol 2009;5:263. [Crossref] [PubMed]
- Wishart DS, Tzur D, Knox C, et al. HMDB: the Human Metabolome Database. Nucl Acids Res 2007;35:D521-26. [Crossref] [PubMed]
- Mandal R, Chamot D, Wishart DS. The role of the Human Metabolome Database in inborn errors of metabolism. J Inherit Metab Dis 2018;41:329-36. [Crossref] [PubMed]
- Auray-Blais C, Boutin M. Novel gb(3) isoforms detected in urine of fabry disease patients: a metabolomic study. Curr Med Chem 2012;19:3241-52. [Crossref] [PubMed]
- Auray-Blais C, Boutin M, Gagnon R, et al. Urinary globotriaosylsphingosine-related biomarkers for Fabry disease targeted by metabolomics. Anal Chem 2012;84:2745-53. [Crossref] [PubMed]
- Manwaring V, Boutin M, Auray-Blais C. A metabolomic study to identify new globotriaosylceramide-related biomarkers in the plasma of Fabry disease patients. Anal Chem 2013;85:9039-48. [Crossref] [PubMed]
- Dupont FO, Gagnon R, Boutin M, et al. A metabolomic study reveals novel plasma lyso-Gb3 analogs as Fabry disease biomarkers. Curr Med Chem 2013;20:280-8. [Crossref] [PubMed]
- Boutin M, Auray-Blais C. Metabolomic discovery of novel urinary galabiosylceramide analogs as Fabry disease biomarkers. J Am Soc Mass Spectrom 2015;26:499-510. [Crossref] [PubMed]
- Gertsman I, Barshop BA. Promises and pitfalls of untargeted metabolomics. J Inherit Metab Dis 2018;41:355-66. [Crossref] [PubMed]
- Coene KLM, Kluijtmans LAJ, van der Heeft E, et al. Next-generation metabolic screening: targeted and untargeted metabolomics for the diagnosis of inborn errors of metabolism in individual patients. J Inherit Metab Dis 2018;41:337-53. [Crossref] [PubMed]
- Jacob M, Malkawi A, Albast N, et al. A targeted metabolomics approach for clinical diagnosis of inborn errors of metabolism. Anal Chim Acta 2018;1025:141-53. [Crossref] [PubMed]
- Janečková H, Hron K, Wojtowicz P, et al. Targeted metabolomic analysis of plasma samples for the diagnosis of inherited metabolic disorders. J Chromatogr A 2012;1226:11-7. [Crossref] [PubMed]
- Fan M, Sidhu R, Fujiwara H, et al. Identification of Niemann-Pick C1 disease biomarkers through sphingolipid profiling. J Lipid Res 2013;54:2800-14. [Crossref] [PubMed]
- Wikoff WR, Gangoiti JA, Barshop BA, et al. Metabolomics identifies perturbations in human disorders of propionate metabolism. Clin Chem 2007;53:2169-76. [Crossref] [PubMed]
- Miller MJ, Kennedy AD, Eckhart AD, et al. Untargeted metabolomic analysis for the clinical screening of inborn errors of metabolism. J Inherit Metab Dis 2015;38:1029-39. [Crossref] [PubMed]
- Sandlers Y, Mercier K, Pathmasiri W, et al. Metabolomics Reveals New Mechanisms for Pathogenesis in Barth Syndrome and Introduces Novel Roles for Cardiolipin in Cellular Function. PLoS One 2016;11. [Crossref] [PubMed]
- McCoin CS, Piccolo BD, Knotts TA, et al. Unique plasma metabolomic signatures of individuals with inherited disorders of long-chain fatty acid oxidation. J Inherit Metab Dis 2016;39:399-408. [Crossref] [PubMed]
- Kennedy AD, Pappan KL, Donti TR, et al. Elucidation of the complex metabolic profile of cerebrospinal fluid using an untargeted biochemical profiling assay. Mol Genet Metab 2017;121:83-90. [Crossref] [PubMed]
- Constantinou MA, Papakonstantinou E, Benaki D, et al. Application of nuclear magnetic resonance spectroscopy combined with principal component analysis in detecting inborn errors of metabolism using blood spots: a metabonomic approach. Anal Chim Acta 2004;511:303-12. [Crossref]
- Pan Z, Gu H, Talaty N, et al. Principal component analysis of urine metabolites detected by NMR and DESI-MS in patients with inborn errors of metabolism. Anal Bioanal Chem 2007;387:539-49. [Crossref] [PubMed]
- Dénes J, Szabó E, Robinette SL, et al. Metabonomics of newborn screening dried blood spot samples: a novel approach in the screening and diagnostics of inborn errors of metabolism. Anal Chem 2012;84:10113-120. [Crossref] [PubMed]
- Scolamiero E, Cozzolino C, Albano L, et al. Targeted metabolomics in the expanded newborn screening for inborn errors of metabolism. Mol Biosyst 2015;11:1525-35. [Crossref] [PubMed]
- Gertsman I, Gangoiti JA, Barshop BA. Validation of a dual LC-HRMS platform for clinical metabolic diagnosis in serum, bridging quantitative analysis and untargeted metabolomics. Metabolomics 2014;10:312-23. [Crossref] [PubMed]
- Aygen S, Dürr U, Hegele P, et al. NMR-Based Screening for Inborn Errors of Metabolism: Initial Results from a Study on Turkish Neonates. JIMD Rep 2014;16:101-11. [Crossref] [PubMed]
- Bouatra S, Aziat F, Mandal R, et al. The human urine metabolome. PLoS One 2013;8. [Crossref] [PubMed]
- Kennedy AD, Miller MJ, Beebe K, et al. Metabolomic Profiling of Human Urine as a Screen for Multiple Inborn Errors of Metabolism. Genet Test Mol Biomarkers 2016;20:485-95. [Crossref] [PubMed]
- Hampe MH, Panaskar SN, Yadav AA, et al. Gas chromatography/mass spectrometry-based urine metabolome study in children for inborn errors of metabolism: An Indian experience. Clin Biochem 2017;50:121-6. [Crossref] [PubMed]
- Roberts SB, Lucas A. Measurement of urinary constituents and output using disposable napkins. Arch Dis Child 1985;60:1021-24. [Crossref] [PubMed]
- Goodpaster AM, Ramadas EH, Kennedy MA. Potential effect of diaper and cotton ball contamination on NMR- and LC/MS-based metabonomics studies of urine from newborn babies. Anal Chem 2011;83:896-902. [Crossref] [PubMed]
- Palmas F, Mussap M, Fattuoni C. Urine metabolome analysis by gas chromatography-mass spectrometry (GC-MS): Standardization and optimization of protocols for urea removal and short-term sample storage. Clin Chim Acta 2018;485:236-42. [Crossref] [PubMed]
- Lanpher B, Brunetti-Pierri N, Lee B. Inborn errors of metabolism: the flux from Mendelian to complex diseases. Nat Rev Genet 2006;7:449-60. [Crossref] [PubMed]
- Shin SY, Fauman EB, Petersen AK, et al. An atlas of genetic influences on human blood metabolites. Nat Genet 2014;46:543-50. [Crossref] [PubMed]
- Wangler MF, Hubert L, Donti TR, et al. A metabolomic map of Zellweger spectrum disorders reveals novel disease biomarkers. Genet Med 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Tebani A, Afonso C, Marret S, et al. Omics-Based Strategies in Precision Medicine: Toward a Paradigm Shift in Inborn Errors of Metabolism Investigations. Int J Mol Sci 2016;17. [Crossref] [PubMed]
- Dercksen M, Koekemoer G, Duran M, et al. Organic acid profile of isovaleric acidemia: a comprehensive metabolomics approach. Metabolomics 2013;9:765-77. [Crossref]
- Tebani A, Schmitz-Afonso I, Abily-Donval L, et al. Urinary metabolic phenotyping of mucopolysaccharidosis type I combining untargeted and targeted strategies with data modeling. Clin Chim Acta 2017;475:7-14. [Crossref] [PubMed]
- Sahoo S, Franzson L, Jonsson JJ, et al. A compendium of inborn errors of metabolism mapped onto the human metabolic network. Mol Biosyst 2012;8:2545-58. [Crossref] [PubMed]
- Graham E, Lee J, Price M, et al. Integration of genomics and metabolomics for prioritization of rare disease variants: a 2018 literature review. Inherit Metab Dis 2018. [Epub ahead of print].
- Strauss KA, Puffenberger EG, Morton DH. In: Adam MP, Ardinger HH, Pagon RA, et al. editors. Maple syrup urine disease. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle, 2013:93-7.
- Guo L, Milburn MV, Ryals JA, et al. Plasma metabolomic profiles enhance precision medicine for volunteers of normal health. Proc Natl Acad Sci 2015;112:E4901-10. [Crossref] [PubMed]
- Piras D, Locci E, Palmas F, et al. Rare disease: a focus on metabolomics. Exp Opin Orphan Dis 2016;4:1229-37. [Crossref]


