e-thrombosis: epidemiology, physiopathology and rationale for preventing computer-related thrombosis
Introduction
The considerable advancements and large geographic and localized diffusion of information technology (IT) and computers has revolutionized human life more than any other discovery or invention over the past century. Although there is a widespread perception that computers have brought considerably more advantages than risks to mankind (thus including “e-health”) (1), the technology has also brought about a number of challenges and potential dangers to human health. Beside computer addiction, which has recently been recognized as a global health care issue by the World Health Organization (WHO) (2), the long-term use of computers may directly promote the development of several serious diseases, including computer vision syndrome, sleep and metal disorders, accidental injuries along with musculoskeletal problems, such as carpal tunnel syndrome (2). Nevertheless, the prolonged use of computers may also be seen as an important risk for developing many biological and metabolic dysfunctions, including those consequent to physical inactivity, obesity and hypertension (2). Among the many and multifaceted disturbances that prolonged computer usage may carry, is also the risk of developing venous thromboembolism (VTE), thus including both deep vein thrombosis (DVT) and pulmonary embolism (PE), a situation that is widely misrecognized or overlooked.
The term “e-thrombosis” was originally coined by Beasley et al. in 2003 (3), who put forward the hypothesis that the increasing diffusion of computers for work or recreational activities would have dramatically enhanced the epidemiological burden of seated immobility thrombosis. Soon thereafter, the trueness of this assumption was substantiated by a series of case reports, and clinical studies, which have provided clear and solid evidence, that long seated immobility while using computers should now be regarded as a major contributing factor of acute VTE. Therefore, the aim of this article is to provide a narrative update on computer-related thrombosis, delivering also potentially useful suggestions for preventing this rare but potentially lethal “syndrome”.
Epidemiology computer-related thrombosis
The very first case of VTE associated with prolonged sitting, described by Homans, more than 60 years ago (4), was at a time when the modern personal computers were still in infancy. This is when the relatively short history of e-thrombosis began, with the description of some case reports in the early 2000s. As later followed by the publication of epidemiological investigations, these helped to provide a clearer picture on the epidemiology of e-thrombosis.
Case reports
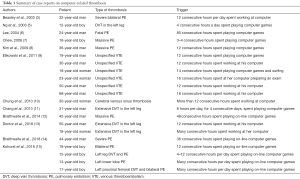
As mentioned earlier, the term e-thrombosis was coined by Beasley et al. in 2003 (3), who described the case of a 32-year-old man who developed an extensive bilateral proximal PE. The investigation of the potential risk factors for VTE had revealed that the patient spent over 12 hours per day (up to 18 hours occasionally, 6 of which without standing up) working at his personal computer. This original case report was then followed by many others, as summarized in Table 1 and briefly discussed in the following part of this section.
Full table
Soon after the first report, Ng et al. described the case of a 12-year-old boy who developed DVT of the left popliteal vein with proximal extension to the distal superficial femoral vein, which was attributed to prolonged immobility (for up to 4 hours a day) while playing computer games (5). Another case of fatal PE was then reported by Lee in a 24-year-old man, who had spent 80 consecutive hours seated playing computer games (6). Chew described the case of a 16-year-old boy who was diagnosed with acute PE, complicated by right middle lobe pulmonary infarction, after several sessions of computer gaming lasting approximately 3 hours (7). Notably, the patient had also a previous history of bilateral DVT, also developed after prolonged computer gaming sessions.
Kim et al. described the case of a 36-year-old man who was diagnosed with massive PE after playing computer games (seated) for approximately 12 hours per day for 2 weeks (8). In 2011, Elikowski et al. described as many as 6 cases of computer-related thrombosis (9). Briefly, the first case was a 19-year-old man who developed VTE after playing for 12 consecutive hours (up to 4 hours uninterrupted) of computer games, the second case was a 30-year-old man who developed VTE after working at his computer for 12 consecutive hours (up to 4 hours uninterrupted), the third was a 19-year-old woman who developed VTE after playing for 14 consecutive hours (up to 5 hours uninterrupted) computer games and internet surfing, the fourth was a 23-year-old woman who developed VTE after having prepared for an examination using her computer for 16 consecutive hours (up to 5 hours uninterrupted), the fifth was a 50-year-old male radiologist who developed VTE after remaining seated for 12 consecutive hours (up to 3 hours uninterrupted) working at a computer, whilst the sixth was a 68-year-old man who developed VTE after using his computer for up to 16 consecutive hours (up to 4 hours uninterrupted) for professional education.
Chung et al. then described the case of a 30-year-old woman who was diagnosed with cerebral venous sinus thrombosis after prolonged sitting (i.e., for over 12 hours) in front of her personal computer (10). Chang et al. also reported the case of 31-year-old man who developed an extensive DVT in the left leg, after having spent as many as 8 hours per day, for 4 consecutive days, playing computer games (11). Braithwaite et al. described the case of a 42-year-old man who developed bilateral pulmonary emboli accompanied with right heart strain, after having spent 48 consecutive hours playing on-line computer games, leaving his chair just for toilet breaks (12). More recently, Doctor and Seth described two other cases of venous thrombosis developing after prolonged computer use (13). The former case was a 50-year-old male, software professional, who developed a DVT in the iliac, femoral and popliteal veins of the left leg after having worked on his computer for 12 consecutive hours, with less than 4 breaks. The latter case was an 18-year-old girl who developed a DVT in the iliac, femoral and saphenous veins of the left leg after having spent many hours working at her computer. Braithwaite et al. described another case of a 44-year-old man who developed a severe PE at the bifurcation of the right main pulmonary artery, progressing into the lobar and segmental arteries and accompanied by pulmonary infarction, after having spent 36 hours (remaining seated for up to 12 consecutive hours) playing on-line computer games (14). Kohorst et al. described four additional cases of severe PE in adolescents who had recently spent a long time playing computer games before the acute thrombotic event (15). The first of these was a 18-year-old obese boy who was diagnosed with bilateral pulmonary emboli complicated by right lower pulmonary lobe infarction after having spent up to 12 consecutive hours per day playing computer games; the second was a 15-year-old obese boy who developed acute DVT in the veins of left upper calf followed by PE in the right pulmonary artery after having spent between 4–12 hours per day playing computer games; the third was a13-year-old obese boy who developed a left lower lobe PE, after having played computer games for several consecutive hours each day; whilst the fourth was a 17-year-old obese boy who was diagnosed with left proximal femoral DVT and bilateral basilar PE complicated by pulmonary infarction after having spent several hours playing computer games.
Albeit not directly related to computer-related immobility, it is also worthwhile mentioning here that an atypical case of upper limb DVT has been described by Phipps and Ng and in a 33-year-old man, who spent long periods playing with his gaming console in an unusual position (16).
Epidemiological studies
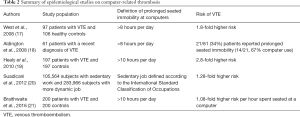
Along with the many cases described in the previous section of this article, some notable epidemiological investigations have also been published, as summarized in Table 2. The first article, published by West et al. in 2008, was a cross-sectional study that was based on 97 patients with VTE, and 106 healthy people as a control (17). In the final multivariate model, prolonged seated immobility at work (thus including time spent seated at a personal computer for more than 8 hours) was associated with a 1.8-fold higher risk [odds ratio (OR), 1.8; 95% confidence interval (CI), 0.71–4.80] of VTE. Notably, each 1 hour of seated immobility was found to enhance the cumulative risk of VTE by 10% (OR, 1.1; 95% CI, 1.0–1.2).
Full table
Aldington et al. then studied 61 patients with a recent diagnosis of VTE (18), and reported that 21/61 (34%) of these experienced prolonged seated immobility at work (i.e., between 8 and 14 consecutive hours, between 1 to 5 of which was without getting up) before the event. Most of these patients (14/21; 67%) were using computer devices.
Healy et al. performed a cross-sectional study that was based on the 197 VTE patients, and the 197 subjects admitted to a coronary care unit with conditions other than VTE who served as the control group (19). Prolonged, computer-related, seated immobility (i.e., for more than 10 hours) was found to be more frequently present in VTE cases than in controls (16.8% versus 9.6%; P=0.040). In multivariate analysis, prolonged computer-related seated immobility was associated with a 2.8-fold higher risk (OR, 2.8; 95% CI, 1.2–6.1) of VTE. Overall, the VTE risk was found to be enhanced by 10% (OR, 1.1; 95% CI, 1.0–1.2) for each additional hour spent seated at a computer.
Suadicani et al. carried out a large dynamic cohort study based on the two groups of subjects with characteristically sedentary (n=105,564) and typically dynamic (n=283,966) jobs (20). Overall, 77 cases (0.07%) of fatal PE were recorded in the sedentary work group, when compared to the 167 cases (0.06%) of subjects with a more active work style. In multivariate analysis, sedentary work was associated with a 28% higher risk of developing PE [relative risk (RR), 1.28; 95% CI, 0.97–1.67; P=0.04 in one-sided test].
More recently, Braithwaite et al. carried out another cross-sectional study, which included 200 patients with a VTE episode that was diagnosed over the previous 6 months. It also included 200 control group individuals, who had been treated for an upper limb injury during the same period of time (21). Although the frequency of prolonged computer-related seated immobility was almost identical between the tested cases and the control group (18% versus 16%; P=0.50), a subsequent multivariate analysis revealed that work/computer seated immobility (per hour) was associated with an 8% higher risk (OR, 1.08; 95% CI, 1.01–1.60) of developing VTE.
Physiopathology of computer-related thrombosis
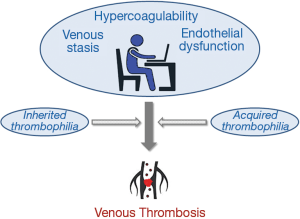
The leading assumptions of venous thrombosis have been originally formulated by the German physician Rudolf Virchow, more than 160 years ago (22). Briefly, the generation of venous blood clots is fostered by the presence of the three leading and synergistic mechanisms, represented by venous blood stasis, hypercoagulability and endothelial dysfunction/injury (23), and can then be triggered by a variety of conventional, or atypical factors (24,25). Usually, along with the existence of new convincing epidemiological evidence, the next essential step for reasonably linking a putative risk factor to given clinical outcome necessitates the identification of one or more plausible biological links. Therefore, the basic assumption here, is that prolonged computer seated immobility should lead or predispose, to developing one or more of the three components of the so-called Virchow’s triad.
Regarding venous blood stasis, Levin et al. carried out an elegant study on 12 healthy subjects, who all had their popliteal vein blood flow assessed by the means of a Doppler ultrasound, while being prone or seated with legs in different positions (i.e., flexed at either 90° or 120°) (26). Although there was no difference in peak systolic velocity that could be observed between the two sitting positions, a considerable reduction of popliteal vein blood flow (i.e., between 83–87%) was found between the prone, and either sitting position. Similar data was published by Hitos et al. (27), who measured the blood flow in the popliteal vein of 22 subjects, and found a blood flow reduction of 1.4- and 2-fold in a conventional sitting position and while being seated motionless with the feet not touching the ground, respectively. Most notably, original blood flow could be restored by performing foot exercises.
The development of hypercoagulability during prolonged permanence in a seated position has also been convincingly reported in many studies. Schobersberger et al. investigated coagulation and fibrinolysis biomarkers in 19 healthy subjects prior to, during, and immediately after a 10-hour bus travel (28), and found a significant activation of blood coagulation by thrombelastography assessment, combined with a significant increase of prothrombin fragment F1+2 values after the journey. Notably, significant venous stasis could also be observed, as mirrored by enhanced leg volume, especially in the calf. Howard et al. studied the effect of either interrupted or uninterrupted 5-hour sitting on some coagulation parameters in 19 sedentary, middle-age, overweight adults (29). Overall, uninterrupted sitting was effective to significantly increase the plasma concentration of fibrinogen to a much larger extent than interrupted sitting (i.e., +0.24 g/L versus +0.07 g/L; P<0.05), whilst no other significant changes could be observed in D-dimer, von Willebrand factor and activated partial thromboplastin time (APTT) values. Interestingly, a remarkable hemoconcentration was also noted, with hemoglobin concentration displaying a ~1.5-fold increase during uninterrupted compared to interrupted sitting. Similar evidence was also reported by Lippi et al. (30), who investigated the changes of APTT and fibrinogen values in 19 healthy subjects, after remaining supine for 25 min, seated for 20 min and upright for 20 min. The change from supine to sitting position induced a significant increase of fibrinogen concentration (from 2.20 to 2.27 g/L; +3%), whilst the value of APTT remained virtually unchanged. Interestingly, Kabrhel et al. studied a total of 4,346 patients who were admitted to the emergency department for suspected PE (31), and reported that history of immobility was significantly associated with D-dimer values, which exhibited a 50–60% increase across different categories of immobility.
Even stronger appears the relationship between maintaining prolonged sitting positions and endothelial dysfunction. In a recent review, Thosar et al. has collected a large volume of supporting data, to confirm that a prolonged sitting position may contribute to enhancing stress in the legs, increasing oxidative stress, and finally impairing endothelial function (32). This evidence was then confirmed in the recent study of Restaino et al. (33), who showed an impaired flow-mediated dilation in the legs after 3 hours of immobility in seated position. Interestingly, Morishima et al. also demonstrated that the endothelial dysfunction in the legs following prolonged sitting could be prevented by short bouts of leg movements (34). Virtually identical findings were published earlier by Thosar et al. (35), who also observed that a 3-hour sitting posture induced a substantial impairment of shear rate and flow-mediated dilation, both potentially preventable by light activity breaks.
Likewise thrombosis developing during or immediately after long-haul travels (36,37), it seems reasonable to conclude that computer-related immobility may be regarded as an independent prothrombotic risk factor, and that its impact on the cumulative risk of developing venous clots and thromboembolism will be predictably magnified by the presence of one or more, acquired or inherited, prothrombotic conditions, including obesity (Figure 1). This hypothesis has been persuasively substantiated by the results published by Siniarski et al. (38). The authors studied 493 patients with a previous episode of VTE, and showed that the thrombotic risk, which was resulting from seated immobility, was substantially enhanced in patients bearing Factor V Leiden, prothrombin G20210A polymorphism or after protracted computer usage.
Rationale prevention of computer-related thrombosis
Although e-thrombosis is still be regarded as a relatively rare disorder (i.e., with a cumulative frequency <1:2,000) (39), the use of personal computers has consistently grown during the past 20 years, with worldwide sales having nearly doubled from the year 2000 (i.e., 134.7 million) to present time (259.4 million in the year 2017), reaching a peak around the years 2009–2012, and slightly declining afterwards due to a growing market and increasing usage of smartphones and tablet computers (40). Notably, the cumulative shipment of desktop, laptop and tablet computers is predicted to increase to nearly 400 million units in the year 2020, and it is hence predictable that the burden of e-thrombosis will increase further, since approximately 80% of users are expected to spend a large part of their life working, playing or internet surfing with these devices in the next decade (41). This far-reaching prediction will project the epidemiology of e-thrombosis far ahead than that of a “rare disease”, thus urgently calling for the establishment of a set of preventive measures aimed at lowering the risk of thrombosis caused by computer-related seated immobility. Notably, alertness about such risk has already been raised for certain work practices, encompassing several hours of the day which are spent working with computers (e.g., radiology) (42).
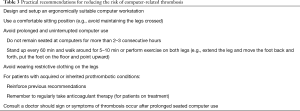
Although it may seem paradoxical to link immobility with travels, the potential suggestions for preventing computer-related thrombosis are not really different from those that can be formulated for preventing other forms of seated immobility thrombosis, such as the well-known “traveler’s thrombosis” which typically develops during, or immediately after, long haul flights or prolonged car journeys (37,43) (Table 3). These tentative recommendations basically entail designing, and setting up ergonomically suitable computer workstations, using comfortable sitting positions, avoiding long, computer-seated immobility, and avoiding wearing restrictive clothing on the legs. Reinforced measures should additionally be advisable in patients with acquired, or inherited prothrombotic conditions. Interestingly, Sherman and Hedge reported that lower leg circulation may be significantly improved, and perhaps the risk of thrombosis reduced, by placing the feet on a dynamic footrest which passively moves the lower limbs (44). Development of these tools may hence be seen as a valuable perspective for lowering the risk of computer-related thrombosis, similarly to the use of mechanical prophylaxis in patients with forced immobility of lower limbs (i.e., during prolonged bedridden, after surgery) (45).
Full table
Conclusions
Convincing epidemiological and biological evidence now exists that computer-related thrombosis (i.e., e-thrombosis) should be regarded as an independent clinical entity, deserving enhanced healthcare focus and interventions, due to the growing worldwide diffusion of laptops, and personal or tablet computers. Special attention should be paid to the youth (15,46) and perhaps to men, since most cases of computer-related VTE have been described in male subjects playing computer games. Although the incidence of VTE is relatively low in childhood and adolescence (i.e., typically lower than 5 per 100,000), the increasing addition of internet surfing and computer game playing, may contribute to the change of fate for e-thrombosis, and turn it from a rare disease to a noticeably frequent pathology (47).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Disclaimer: The views expressed in this article are those of the authors, and do not necessarily reflect those of the University Hospital of Verona, or of NSW Health Pathology.
References
- Granja C, Janssen W, Johansen MA. Factors Determining the Success and Failure of eHealth Interventions: Systematic Review of the Literature. J Med Internet Res 2018;20. [Crossref] [PubMed]
- World Health Organization. Public Health Implications of Excessive Use of the Internet, Computers, Smartphones and Similar Electronic Devices. Geneva, Switzerland: WHO Press, World Health Organization, 2014.
- Beasley R, Raymond N, Hill S, et al. eThrombosis: the 21st century variant of venous thromboembolism associated with immobility. Eur Respir J 2003;21:374-6. [Crossref] [PubMed]
- Homans J. Thrombosis of the deep leg veins due to prolonged sitting. N Engl J Med 1954;250:148-9. [Crossref] [PubMed]
- Ng SM, Khurana RM, Yeang HW, et al. Is prolonged use of computer games a risk factor for deep venous thrombosis in children? Case study. Clin Med (Lond) 2003;3:593-4. [Crossref] [PubMed]
- Lee H. A new case of fatal pulmonary thromboembolism associated with prolonged sitting at computer in Korea. Yonsei Med J 2004;45:349-51. [Crossref] [PubMed]
- Chew HC. Shortness of breath in a computer gamer. Am J Emerg Med 2006;24:892-4. [Crossref] [PubMed]
- Kim H, Choe KH, Lee KM, et al. A Case of Massive Pulmonary Thromboembolism in a Young Man Attribute to Computer Gaming. Tuberc Respir Dis 2009;66:211-5. [Crossref]
- Elikowski W, Małek M, Zytkiewicz M, et al. "eThrombosis" - venous thromboembolism provoked by prolonged sitting position by a computer. A case series report of six patients. Kardiol Pol 2011;69:377-81; discussion 382. [PubMed]
- Chung MH, Kuo EY, Wu CM, et al. Cerebral “eThrombosis”: Cerebral Venous Sinus Thrombosis Associated with Prolonged Sitting in Front of a Computer. Hong Kong J Emerg Med 2013;21:111-4. [Crossref]
- Chang HC, Burbridge H, Wong C. Extensive deep vein thrombosis following prolonged gaming ('gamer's thrombosis'): a case report. J Med Case Rep 2013;7:235. [Crossref] [PubMed]
- Braithwaite I, Maxwell G, Sparks S, et al. A man who collapsed after using the internet. JRSM Open 2014;5. [Crossref] [PubMed]
- Doctor N, Seth P. When Computers Can Kill—Two Unusual Cases of “E-Thrombosis”. Int J Clin Med 2018;9:335-40. [Crossref]
- Braithwaite I, Shirtcliffe P, Jurevics R, et al. Gaming: a 21st century variant of seated immobility thromboembolism. N Z Med J 2018;131:66-8. [PubMed]
- Kohorst MA, Warad DM, Nageswara Rao AA, et al. Obesity, sedentary lifestyle, and video games: The new thrombophilia cocktail in adolescents. Pediatr Blood Cancer 2018;65. [Crossref] [PubMed]
- Phipps C, Ng HJ. Upper limb deep vein thrombosis and portable computer games. Am J Med 2008;121. [Crossref] [PubMed]
- West J, Perrin K, Aldington S, et al. A case-control study of seated immobility at work as a risk factor for venous thromboembolism. J R Soc Med 2008;101:237-43. [Crossref] [PubMed]
- Aldington S, Pritchard A, Perrin K, et al. Prolonged seated immobility at work is a common risk factor for venous thromboembolism leading to hospital admission. Intern Med J 2008;38:133-5. [Crossref] [PubMed]
- Healy B, Levin E, Perrin K, et al. Prolonged work- and computer-related seated immobility and risk of venous thromboembolism. J R Soc Med 2010;103:447-54. [Crossref] [PubMed]
- Suadicani P, Hannerz H, Bach E, et al. Jobs encompassing prolonged sitting in cramped positions and risk of venous thromboembolism: cohort study. JRSM Short Rep 2012;3:8. [Crossref] [PubMed]
- Braithwaite I, Healy B, Cameron L, et al. Venous thromboembolism risk associated with protracted work- and computer-related seated immobility: A case-control study. JRSM Open 2016;7. [Crossref] [PubMed]
- Virchow R. Phlogose und Thrombose im Gefa¨ßsystem; Gesammelte Abhandlungen zur Wissenschaftlichen Medizin. Frankfurt, Germany: Staatsdruckerei, 1856.
- Lippi G, Favaloro EJ. Venous and Arterial Thromboses: Two Sides of the Same Coin? Semin Thromb Hemost 2018;44:239-48. [Crossref] [PubMed]
- Crous-Bou M, Harrington LB, Kabrhel C. Environmental and Genetic Risk Factors Associated with Venous Thromboembolism. Semin Thromb Hemost 2016;42:808-20. [Crossref] [PubMed]
- Lippi G, Franchini M, Favaloro EJ. Unsuspected triggers of venous thromboembolism--trivial or not so trivial? Semin Thromb Hemost 2009;35:597-604. [Crossref] [PubMed]
- Levin E, Macintosh D, Baker T, et al. Effect of sitting in ergonomic chairs on lower limb venous blood flow. Occup Ergon 2009;8:125-32.
- Hitos K, Cannon M, Cannon S, et al. Effect of leg exercises on popliteal venous blood flow during prolonged immobility of seated subjects: implications for prevention of travel-related deep vein thrombosis. J Thromb Haemost 2007;5:1890-5. [Crossref] [PubMed]
- Schobersberger W, Mittermayr M, Innerhofer P, et al. Coagulation changes and edema formation during long-distance bus travel. Blood Coagul Fibrinolysis 2004;15:419-25. [Crossref] [PubMed]
- Howard BJ, Fraser SF, Sethi P, et al. Impact on hemostatic parameters of interrupting sitting with intermittent activity. Med Sci Sports Exerc 2013;45:1285-91. [Crossref] [PubMed]
- Lippi G, Salvagno GL, Lima-Oliveira G, et al. Influence of posture on routine hemostasis testing. Blood Coagul Fibrinolysis 2015;26:716-9. [Crossref] [PubMed]
- Kabrhel C, Mark Courtney D, Camargo CA Jr, et al. Factors associated with positive D-dimer results in patients evaluated for pulmonary embolism. Acad Emerg Med 2010;17:589-97. [Crossref] [PubMed]
- Thosar SS, Johnson BD, Johnston JD, et al. Sitting and endothelial dysfunction: the role of shear stress. Med Sci Monit 2012;18:RA173-80. [Crossref] [PubMed]
- Restaino RM, Walsh LK, Morishima T, et al. Endothelial dysfunction following prolonged sitting is mediated by a reduction in shear stress. Am J Physiol Heart Circ Physiol 2016;310:H648-53. [Crossref] [PubMed]
- Morishima T, Restaino RM, Walsh LK, et al. Prolonged sitting-induced leg endothelial dysfunction is prevented by fidgeting. Am J Physiol Heart Circ Physiol 2016;311:H177-82. [Crossref] [PubMed]
- Thosar SS, Bielko SL, Mather KJ, et al. Effect of prolonged sitting and breaks in sitting time on endothelial function. Med Sci Sports Exerc 2015;47:843-9. [Crossref] [PubMed]
- Lippi G, Franchini M, Favaloro EJ. Holiday thrombosis. Semin Thromb Hemost 2011;37:869-74. [Crossref] [PubMed]
- Lippi G, Favaloro EJ. Car Travel-Related Thrombosis: Fact or Fiction? Semin Thromb Hemost 2018;44:327-33. [Crossref] [PubMed]
- Siniarski A, Wypasek E, Fijorek K, et al. Association between thrombophilia and seated immobility venous thromboembolism. Blood Coagul Fibrinolysis 2014;25:135-41. [Crossref] [PubMed]
- Danese E, Lippi G. Rare and orphan disorders: an emerging challenge? Ann Transl Med 2018;6:329.
- Statista. Personal computers (PCs). Last accessed, 25 August, 2018. Available online: https://www.statista.com/study/10871/global-pc-market-statista-dossier/
- Statista. Shipment forecast of laptops, desktop PCs and tablets worldwide from 2010 to 2022. Last accessed, 25 August, 2018. Available online: https://www.statista.com/statistics/272595/global-shipments-forecast-for-tablets-laptops-and-desktop-pcs/
- Gerard PS, Gerczuk P, Mattern M. "eThrombosis": are radiologists at risk? AJR Am J Roentgenol 2007;188:W491. [Crossref] [PubMed]
- Gavish I, Brenner B. Air travel and the risk of thromboembolism. Intern Emerg Med 2011;6:113-6. [Crossref] [PubMed]
- Sherman C, Hedge A. Test of a Dynamic Footrest on Leg Swelling in Sedentary Computer Workers. Proc Hum Factors Ergon Soc Annu Meet 2003;47:942-6. [Crossref]
- Lippi G, Favaloro EJ, Cervellin G. Prevention of venous thromboembolism: focus on mechanical prophylaxis. Semin Thromb Hemost 2011;37:237-51. [Crossref] [PubMed]
- Favaloro EJ, Lippi G. Translational aspects of developmental hemostasis: infants and children are not miniature adults and even adults may be different. Ann Transl Med 2017;5:212. [Crossref] [PubMed]
- Biss TT. Challenges in adolescent venous thromboembolism. Lancet Haematol 2016;3:e264-6. [Crossref] [PubMed]
(English Language Editor: Jeremy Dean Chapnick, AME Publishing Company)