Primary repair of a massive pressure ulcer on the hip: report of one case
Introduction
Pressure ulcer is the leading complication in bedridden patients (1) and typically requires multiple surgeries for debridement and vaccum sealing drainage (VSD); after the deep sinus is cleaned, a second surgery can be performed to close the wound (2). In this article we describe our successful primary repair of a massive pressure ulcer on the hip.
Case presentation
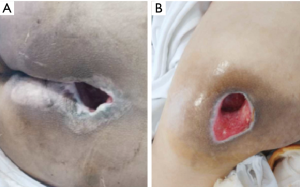
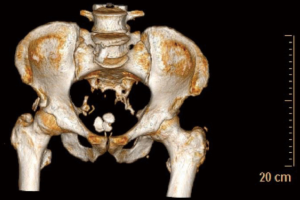
A 47-year-old male patient was diagnosed with systemic lupus erythematosus, paraplegia, and steroid-induced diabetes two years ago. After long-term oral prednisone tablets 10 mg bid for systemic lupus erythematosus and pre-meal administration of oral voglibose dispersible tablets 0.2 mg tid for diabetes, his fasting blood glucose was between 11 and 14.6 mmol/L. One year ago, the patient developed pressure sores on sacrum (Figure 1A) and left hip due to prolonged bed rest. The external opening of the pressure ulcer on left hip was 6 cm × 3.5 cm, and the deep cavity was 20 cm × 15 cm in area (Figure 1B). The greater trochanter was exposed, along with massive yellow-white secretions in deep area (Figure 2).
The nutritional status was poor. Routine blood test showed that C-reactive protein was 177.63 mg/L, absolute red blood cell (RBC) count was 3.13×1012/L, hemoglobin was 79 g/L, and absolute white blood cell (WBC) count was 5.96×109/L. Biochemical tests showed that urea nitrogen was 2.67 mmol/L, creatinine was 53.9 µmol/L, calcium was 1.95 mmol/L, albumin/globulin was 0.5, albumin was 21.7 g/L, prealbumin was 40 mg/L, and aspartate aminotransferase was 24.3 U/L. Wound drainage culture suggested the presence of Morganella morganii and proteus infections.
The blood glucose control was poor before surgery, and the 2h-postprandial plasma glucose (2hPPG) fluctuated between 11.6 and 14.9 mmol/L. Intensive treatment of diabetes was performed with insulin aspart 30 injection (8 IU before breakfast and 6 IU before dinner). Other treatments included antimicrobial therapy (with piperacillin sodium tazobactam injection 3.75 g bid combined with meropenem injection 1.0 g q8h), nutritional support, and wound debridement and drainage (drugs were changed repeatedly on a daily basis). After two weeks of treatment, the systemic and local conditions were improved. Since the pressure on the surgical area must be avoided, the pressure ulcer on the left hip was repaired firstly, so that the patient could alternately be on a supine position or a right lateral position. After the pressure ulcer on the left hip was healed, the one on the sacrum was surgically treated.
Surgical procedure
The patient was asked to take a right lateral position. Since his lower limb sensation had lost, no anesthesia was applied. As seen during the surgery, the pressure ulcer on left hip was oval in shape, with an external opening of 6 cm × 3.5 cm. The greater trochanter of left femur could be palpable directly under the ulcer. The intraoperative exploration was centered on the greater trochanter. A large cavity about 20 cm × 15 cm in area was found under the deep fascia of the adjacent skin. It extended in a lateral direction obliquely downwards the anus, about 10 cm to the most distal end; it extended in a medial direction obliquely downwards the scrotum, about 8 cm to the most distal end; and it extended upwards heart, alongside the gap between tensor fasciae latae and gluteus medius, about 13 cm to the most distal end. Intradermal injection around the wound was performed with 1:500,000 adrenaline saline, and then the skin, subcutaneous tissue, and fascia layer were cut open upwards longitudinally along the median plane to adequately expose the upper edge of the cavity. Meanwhile, transverse resection was performed inwards to fully expose the inner edge of the cavity. The walls of the cavity were found to be old inflammatory granulation tissue and hyperplastic fibrous tissue. The sinus cavity and its walls were injected again with adrenaline saline, and the old inflammatory tissues in the sinus, the inner wall of the cavity, and the surface of the greater trochanter were completely removed (Figure 3A). After complete hemostasis, the topical hydrogen peroxide, physiological saline, iodophor, and physiological saline were applied for washing and disinfection, and the towel was re-applied.
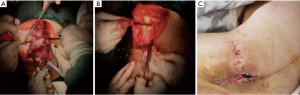
The distal sinus and dead space were then closed tightly from deep to shallow with Vicryl Plus suture (VCP945H). On the upper left side of the greater trochanter, a 10 cm × 8 cm inverted triangular tensor fasciae latae composite tissue flap was designed and harvested, which covered most of the greater trochanter and then fixed (Figure 3B).
A fascia flap of 3 cm × 3 cm was separated from the left lower side of the greater trochanter to cover the lower left edge of the greater trochanter. Then, the lower edge of the wound was cut by the “V” shape to form a 3 cm × 3 cm fascial tissue flap, which was overturned to cover the lower edge of the greater trochanter. The incision was then sutured layer by layer. Subcutaneous exploration showed there were still a small number of shallow cavities, and VSD was installed for negative pressure drainage. After three weeks, most part of the pressure ulcer on left hip was healed, and there was a residual skin defect of 1.5 cm × 0.8 cm (Figure 3C).
Discussion
Pressure ulcer is the leading complication in bed-ridden patients and must be carefully prevented (1). Cerebrovascular events, fractures, and trauma may cause patients to face prolonged bed rest. If the pressure ulcer is not treated timely, the already undernourished and debilitated patients are likely to die due to serious infections (2-4). Patients with large pressure ulcers are often accompanied by severe systemic diseases, severe malnutrition, local and systemic complex infections, and sepsis (5). Debridement combined with VSD is usually required. After the deep sinus is cleaned, a second operation is performed to close the wound. The deep gap was drained after the surgery. Typically, the treatment has long duration and high cost. After the surgery, the dead spaces can easily occur among deep soft tissues or on bone surface, which can be filled with blood and fluid, leading to surgical failure (6).
In our current case, the intraoperative injection of diluted adrenaline saline layer-by-layer helped to maintain a clear surgical field, via which the old inflammatory tissues in the sinus, the inner wall of the cavity, and the surface of the greater trochanter were completely removed, followed by the rinsing and disinfection. During the operation, the layers were tightly sutured to close the sinus and dead space. During the operation, the inverted triangular tensor fasciae latae composite tissue flap was harvested from the left upper corner of the greater trochanter, the fascial flap from left lower side, and the inferior fascial tissue flap from the lower edge of the incision. The flaps were covered on the left upper side, lateral side, and lower edge of the greater trochanter, and then the wound was sutured layer by layer. By doing so we can eliminate the dead spaces, increase local anti-infective ability, and reduce the probability of local friction and recurrence. When necessary, a plurality of tissue flaps are used to fill the cavity. When the cortical bone is eroded, the tissue flap is directly fixed to the exposed bone, followed by tight closure of the wound layer by layer to completely eliminate the dead spaces. Postoperative VSD helps to achieve local fixation, reducing oozing and seepage in local deep tissues. Postoperative subcutaneous exploration still showed a small amount of shallow cavities. Therefore, VSD was performed. After three weeks, the pressure ulcer was well healed and the patient was discharged.
Complex deep pressure ulcer usually requires multiple debridement and drainage, and wound can be surgically closed after its surface becomes clean. Therefore, primary repair can also achieve good clinical effectiveness in some patients with massive complex pressure ulcers.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Health Quality Ontario. Management of chronic pressure ulcers: an evidence-based analysis. Ont Health Technol Assess Ser 2009;9:1-203. [PubMed]
- Dinh A, Bouchand F, Davido B, et al. Management of established pressure ulcer infections in spinal cord injury patients. Med Mal Infect 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Kumar U, Jain P. Infragluteal fasciocutaneous flap for management of recurrent ischial pressure sore. Indian J Plast Surg 2018;51:70-6. [Crossref] [PubMed]
- Zhao Z, Zhang B, Liu Y, et al. Repair of bedsore over greater trochanter in paraplegic patients with rectus femoris island myocutaneous flap. Zhonghua Shao Shang Za Zhi 2014;30:227-30. [PubMed]
- Saino Y, Wakabayashi H, Maeda K, et al. Rehabilitation nutrition in pressure ulcer management with type 2 diabetes: a case report. Asia Pac J Clin Nutr 2018;27:728-34. [PubMed]
- Health Quality Ontario. Negative pressure wound therapy: an evidence-based analysis. Ont Health Technol Assess Ser 2006;6:1-38. [PubMed]


