Should we titrate mechanical ventilation based on driving pressure?—yes
Introduction
Respiratory system driving pressure or distending pressure is a crucial respiratory mechanical concept that represents how much pressure is transmitted in the respiratory system during the tidal ventilation. During volume controlled mechanical ventilation without inspiratory efforts of the patient it will be represented by plateau inspiratory pressure minus the final end-expiratory pressure while in the same condition under pressure controlled ventilation the driving pressure will be the plateau inspiratory pressure in zero inspiratory flow condition after the lungs filling by tidal volume minus the final end-expiratory pressure. This total driving pressure measured in the patient’s airway will be transmitted across the respiratory system structures depending on the homogeneity or heterogeneity of the lungs parenchyma and the abdominal pressure. However, in the presence of inspiratory efforts of the patient the driving pressure will be the sum of the inspiratory efforts plus the difference between the plateau inspiratory pressure with zero inspiratory flow and the final end-expiratory pressure. In situations of assisted ventilation the driving pressure transmission across the respiratory system structures will depend of the intensity of the patient’s inspiratory effort, the synchrony between the patient and the ventilator and the difference between the plateau inspiratory pressure with zero inspiratory flow and the final end-expiratory pressure. The recent reports that lower respiratory driving pressure is associated with better ARDS patients survival during invasive mechanical ventilation and less pulmonary complications in surgical patients and at risk patients without ARDS, makes the best understanding of this subject primordial for the future application of mechanical ventilatory support (1-3).
Driving pressure in patients undergoing invasive mechanical ventilation
Individual data from 3,562 patients with ARDS enrolled in nine reported randomized clinical trials of mechanical ventilation was analyzed by Amato and colleagues (4) using a multilevel mediation analysis. They observed a significant association between driving pressure and ARDS survival even during lung protective ventilation (RR of death: 1.36, 95% CI, 1.17–1.58, P<0.001). These observations suggest that tidal volume might be adjusted to the resultant airway driving pressure in addition to the adjustment to the predicted body weight. They also observed that airway driving pressures higher than 15 cmH2O were associated with increasing rates of mortality in ARDS patients. Recently, Villar and colleagues (5) analyzed the data from two observational studies enclosing 778 patients with moderate and severe ARDS. They divided their patients on quantiles of tidal volume, positive end-expiratory pressure, plateau inspiratory pressure and airway driving pressure evaluated 24 hours after ARDS diagnosis during lung protective ventilation and assessed the risk of hospital death. The authors verified that positive end expiratory pressure and tidal volume that were set according to a protective lung ventilation strategy, had no impact on mortality while a plateau pressure higher than 29 cmH2O and a driving pressure higher than 19 cmH2O were associated with a higher Hospital mortality.
Thus, according to these data the maintenance of a lower driving pressure (preferably below 15 cmH2O) is recommended as part of a protective ventilatory strategy in ARDS aiming at a decrease in hospital mortality in these severe critically ill patients.
Recently, a large prospective, multicenter and controlled trial (ART trial) (6) that compared recruitment maneuver and best-compliance PEEP titration in 501 ARDS patients with 509 ARDS patients ventilated with low PEEP showed an increased 6-month mortality in both groups, but higher in the recruitment and PEEP titration group (65.3% vs. 59.9%, respectively, P=0.04). However, in our opinion, the recruitment maneuver tested in ART trial was abrupt and short (started at 25 cmH2O PEEP, duration of 1 second and not imaging monitored) what could have contributed to the higher levels of observed barotrauma and mortality (7).
Airway driving pressure or transpulmonary driving pressure in ARDS during mechanical ventilation
As respiratory system driving pressure does not account for variable chest wall compliance or different degrees of intra-abdominal pressures or even more to the presence of inspiratory efforts or asynchrony, esophageal manometry can be used to measure transpulmonary pressure that represents the lungs parenchyma stress during tidal volume ventilation. Recently, Baedorf and colleagues (8) analyzed the association between transpulmonary and respiratory system driving pressure measured at baseline, 5 minutes and 24 hours after PEEP titration and 28-day mortality in 56 ARDS patients. They observed that PEEP titration to target positive end-expiratory transpulmonary pressures resulted in improved elastance, improved driving pressures and 28-day mortality.
However, future studies regarding the evaluation of transpulmonary and respiratory system driving pressure in ARDS patients with normal and increased abdominal pressure and various degrees of respiratory system compliance is still needed in order to established the value of both as a bedside ventilator target as well as a prognosticator of evolution and mortality of those patients.
Another study worth mentioning is the ACURASYS study (9) that compared prospectively and randomized patients with ARDS who received cisatracurium continuously in the first 48 hours of mechanical ventilation with patients who received curare only if necessary. The observation that the more severe ARDS patients (PaO2/FiO2 less than 120) who received cisatracurium continuously presented a lower mortality suggested that possible inspiratory efforts and patient-ventilator asynchrony could increase transpulmonary driving pressure and increase ventilator induced lung injury and barotrauma (the patients presented more pneumothorax) resulting in an increase mortality of these ARDS patients.
Transpulmonary driving pressure in spontaneous ventilating acute hypoxemic respiratory failure patients
Recently, Frat and colleagues (10) reported the randomly comparison standard oxygen therapy, high flow nasal oxygen therapy and noninvasive mechanical ventilation in 310 acute hypoxemic respiratory failure patients. They observed no significant differences in intubation ratio in all patients. When they analyzed the patients with PaO2/FiO2 less than 200 they observed that the intubation rate and the 90-day mortality was significantly decreased in high-flow-oxygen group than in non-invasive ventilation and standard oxygen group. When the authors analyzed the predictors of intubation in these patients (11) they observed that the respiratory frequency was a predictor of intubation while using oxygen mask and not while using noninvasive ventilation or high flow oxygen therapy. A PaO2/FiO2 less than 200 and a high tidal volume greater than 9 mL/kg were the two strong predictors of intubation under noninvasive ventilation. As the patients that were intubated or not, during noninvasive ventilation, received 8 cmH2O of pressure support ventilation, the hypothesis that the patients that were intubated and mechanically ventilated presented a more intense inspiratory effort and consequently a higher tidal volume and a higher transpulmonary pressure, reinforces the fact that higher transpulmonary pressures during assisted mechanical ventilation might be associated with a higher mortality
Driving pressures during general anesthesia and post-operative complications
Neto and colleagues (12) analyzed the association of driving pressure, tidal volume and level of PEEP during intraoperative ventilation with the occurrence of postoperative pulmonary complications. A meta-analysis of individual patient data from 17 controlled and randomized clinical trials, including 2,250 patients using protective ventilation during general anesthesia for surgery published was performed. The main outcome was occurrence of postoperative pulmonary complications, including pulmonary infection, barotrauma and postoperative lung injury. Multivariate analysis suggested that driving pressure was associated with the occurrence of postoperative pulmonary complications (OR for each unit increment of driving pressure 1.16, 95% CI, 1.13–1.19; P<0.0001), whereas no association with tidal volume was observed (1.05, 0.98–1.13; P=0.179). They observed that in patients that had been submitted to surgery, intraoperative high driving pressure and changes in the level of PEEP that result in an increment of driving pressure were associated with more postoperative pulmonary complications.
Recently, Fuller and colleagues (13) reported that in patients without ARDS submitted to invasive mechanical ventilation, driving pressure, inspiratory plateau pressure and mechanical power were risk factors for mortality and ARDS, and provide similar information. Mechanical power was also a risk factor for ARDS. They analyzed data from 1,705 mechanically ventilated patients enrolled in a clinical study that analyzed outcomes associated with the early introduction of lung-protective ventilation. The primary and secondary outcomes were respectively mortality and the incidence of ARDS. They observed a mortality rate for the entire cohort of 26.0%. When they compared survivors to non-survivors, the last ones had significantly higher driving pressure [15.9 (5.4) vs. 14.9 (4.4), P=0.005] and plateau pressures [21.4 (5.7) vs. 20.4 (4.6), P=0.001]. Driving inspiratory pressure was independently associated with mortality [adjusted OR, 1.04 (1.01–1.07)] as well plateau inspiratory pressures. There were 152 patients who progressed to ARDS (8.9%). Besides driving pressure and plateau pressure, mechanical power [adjusted OR, 1.03 (1.00–1.06)] was also independently associated with ARDS development.
On the other hand, Schmidt and colleagues (14) retrospectively studied 622 adult patients without ARDS submitted to invasive mechanical ventilation on day 1 in five ICUs in a tertiary center in the United States. The primary outcome was hospital mortality. ARDS was determined using the minimum daily PaO2/FiO2 ratio and an automated text search of chest-X-ray reports. The authors observed that these patients without ARDS, respiratory system driving pressure was not independently associated with hospital mortality (OR, 1.01; 95% CI, 0.97–1.05).
Patient-ventilator asynchrony and lung injury
The asynchrony between the patient’s inspiratory effort and the ventilator can worsen lung injury (15). The occurrence of two consecutive inspirations after a single respiratory effort or “double triggering”, can be injurious because the delivered total tidal volume will be the sum of the two consecutive tidal volumes. In heavily sedated patients reverse triggering (entrainment) can occur, in which the diaphragm is “triggered” by ventilator-driven inspiration. Although the mechanism of initiation is unclear, the phenomenon is identified by a slight decrease in airway pressure and esophageal pressure (corresponding to increased transpulmonary driving pressure), and an increase in delivered tidal volume that can be potentially harmful (15).
Local transpulmonary pressures versus transpulmonary driving pressure and lung injury
The respiratory system driving pressure can be transmitted heterogeneously across the lungs parenchyma in cases of heterogeneous lung diseases as ARDS or Pneumonia or in the case of very intense inspiratory efforts in severe cases of ARDS with increased areas of atelectasis in dependent lung regions. In these situations, the transpulmonary driving pressures measured through an esophageal catheter can not accurately reflects the local transpulmonary pressures (14). Assuming correct calibration, expiratory transpulmonary pressure derived from esophageal pressures reflects transpulmonary pressure in dependent to middle lung where atelectasis usually predominates; inspiratory transpulmonary pressure estimated from elastance ratio may indicate the highest level of lung stress in non-dependent lung (16).
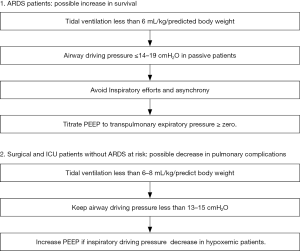
A summary for the titration of invasive mechanical ventilation by inspiratory driving pressure is suggested in Figure 1.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Mauri T, Lazzeri M, Bellani G, et al. Respiratory mechanics to understand ARDS and guide mechanical ventilation. Physiol Meas 2017;38:R280-H303. [Crossref] [PubMed]
- Tonetti T, Vasques F, Rapetti F, et al. Driving pressure and mechanical power: new targets for VILI prevention. Ann Transl Med 2017;5:286. [Crossref] [PubMed]
- Grieco DL, Chen L, Brochard L. Transpulmonary pressure: importance and limits. Ann Transl Med 2017;5:285. [Crossref] [PubMed]
- Amato MB, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 2015;372:747-55. [Crossref] [PubMed]
- Villar J, Martín-Rodríguez C, Domínguez-Berrot AM, et al. A Quantile Analysis of Plateau and Driving Pressures: Effects on Mortality in Patients With Acute Respiratory Distress Syndrome Receiving Lung-Protective Ventilation. Crit Care Med 2017;45:843-50. [Crossref] [PubMed]
- Writing Group for the Alveolar Recruitment for Acute Respiratory Distress Syndrome Trial (ART) Investigators, Cavalcanti AB, Suzumura ÉA, et al. Effect of Lung Recruitment and Titrated Positive End-Expiratory Pressure (PEEP) vs Low PEEP on Mortality in Patients With Acute Respiratory Distress Syndrome: A Randomized Clinical Trial. JAMA 2017;318:1335-45. [Crossref] [PubMed]
- Barbas CSV, Nemer SN. Lung Recruitment and Positive End-Expiratory Pressure Titration in Patients With Acute Respiratory Distress Syndrome. JAMA 2018;319:933. [Crossref] [PubMed]
- Baedorf Kassis E, Loring SH, Talmor D. Mortality and pulmonary mechanics in relation to respiratory system and transpulmonary driving pressures in ARDS. Intensive Care Med 2016;42:1206-13. [Crossref] [PubMed]
- Papazian L, Forel JM, Gacouin A, et al. Neuromuscular blockers in early acute respiratory distress syndrome. N Engl J Med 2010;363:1107-16. [Crossref] [PubMed]
- Frat JP, Thille AW, Mercat A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med 2015;372:2185-96. [Crossref] [PubMed]
- Frat JP, Ragot S, Coudroy R, et al. Predictors of Intubation in Patients With Acute Hypoxemic Respiratory Failure Treated With a Noninvasive Oxygenation Strategy. Crit Care Med 2018;46:208-15. [Crossref] [PubMed]
- Neto AS, Hemmes SN, Barbas CS, et al. Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for general anaesthesia: a meta-analysis of individual patient data. Lancet Respir Med 2016;4:272-80. [Crossref] [PubMed]
- Fuller BM, Page D, Stephens RJ, et al. Pulmonary Mechanics and Mortality in Mechanically Ventilated Patients Without Acute Respiratory Distress Syndrome: A Cohort Study. Shock 2018;49:311-6. [Crossref] [PubMed]
- Schmidt MFS, Amaral ACKB, Fan E, et al. Driving Pressure and Hospital Mortality in Patients Without ARDS: A Cohort Study. Chest 2018;153:46-54. [Crossref] [PubMed]
- Yoshida T, Fujino Y, Amato MB, et al. Fifty Years of Research in ARDS. Spontaneous Breathing during Mechanical Ventilation. Risks, Mechanisms, and Management. Am J Respir Crit Care Med 2017;195:985-92. [Crossref] [PubMed]
- Yoshida T, Brochard L. Ten tips to facilitate understanding and clinical use of esophageal pressure manometry. Intensive Care Med 2018;44:220-2. [Crossref] [PubMed]