Short-term outcomes for total knee arthroplasty patients with active extension lag
Introduction
Total knee arthroplasty (TKA) is the most effective procedure for patients who suffer from end-stage debilitating knee arthritis, demonstrating excellent outcomes and pain reduction (1,2). Despite these positive outcomes, quadriceps strength can often fail to recover to levels of healthy, age-matched cohorts years after surgery (3). This can lead to profound functional consequences such as impairments with balance (4), walking speed (5), stair climbing (6), and increased fall risk (7). Additionally, nearly 50% of patients report impairments in physical function 1 year after TKA (8). Amongst this group, quadriceps weakness can manifest as a limitation in active extension [quadriceps lag (Q-lag)]. This is defined as patient inability to actively move a joint to its passive limit (8), which is in contrast to a flexion contracture in which patients exhibit pathological limitations in active and passive knee extension. More specifically, Q-lag can be defined as an inability to achieve the final 15 degrees of active knee extension (9). This cut-off was based on a study demonstrating a required 60% increase in force of quadriceps contraction from −15 to 0 degrees of extension, and as such is most sensitive for quadriceps weakness (10).
Active extension lag may originate pre-operatively in patients suffering from severe knee arthritis. In a study constituting 348 women who underwent radiographic imaging and quadriceps strength testing, Palmieri-Smith et al. (11) demonstrated that mean quadriceps strength was 22% greater in patients without radiographic evidence of osteoarthritis than with patients who had osteoarthritis (P<0.05). This finding was also corroborated in an observational study conducted by Petterson et al. (12). In that study, consisting of 132 individuals with ipsilateral osteoarthritis, the authors discovered that quadriceps volitional muscle activation in the osteoarthritic limb (0.76±0.21) was 8% lower than that of the contralateral limb with no osteoarthritis (0.83±0.16) (P<0.001). Additional disruption of quadriceps function may also occur intra-operatively and during the immediate post-operative period after a TKA. This is due to soft tissue damage that occurs during knee replacement (13), which may incite muscle inhibition secondary to recruitment failure of muscle motor units (14) thus contributing to poor quadriceps strength recovery.
Currently there is a paucity of studies evaluating midterm outcomes of TKA patients with persistent Q-lag after discharge from physical therapy (PT). Therefore, the purpose of this study was to assess short-term outcomes of patients who underwent TKA and were discharged from PT with Q-lag. More specifically, we compared: (I) numeric 1–10 scaled pain scores; and (II) rates of readmission to PT in TKA patients who had 15 degrees or more of active extension lag after discharge from PT to patients who presented with no Q-lag.
Methods
Patient selection
Institutional Board Review exempt approval was obtained for the retrospective review of 168 continuous patients who underwent primary total knee replacement at our institution between the years of 2013 and 2015. Inclusion criteria comprised of patients who were between the age of 50 and 85 years of age and underwent a unilateral primary TKA with a minimum of 12 months follow-up. Patients who had a diagnosis of inflammatory arthritis (n=6), chronic pain syndromes (n=3), history of opiate or illicit drug abuse (n=3), underwent revision TKA and/or bilateral TKA (n=3), or recently (within 1 year) underwent total hip arthroplasty were excluded from analysis (n=3). These patients were excluded to mitigate cofounding variables that would influence results. A total of 18 patients were excluded leaving 150 for analysis (112 women and 38 men) with a mean age of 63.0 years (range, 50.0–85.0 years) and a mean follow-up of 30.7 months (range, 18.0–47.0 months) (Table 1).
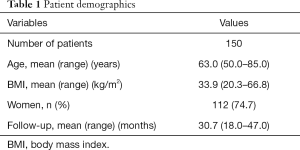
Full table
Surgical procedure
All surgeries underwent standard medial para-patellar approach. Bone cuts were made perpendicular to the mechanical axis with the help of an intramedullary alignment system. The proximal tibia was also cut perpendicular to the mechanical axis of the tibia with the help of extramedullary guides. All patellas were resurfaced. A spinal anesthetic was used for all patients. All knees were closed in flexion. Tourniquet was not used. All patients underwent the same post-operative pathway. Patients were discharged to home after demonstrating adequate pain control, and functional ability. All study patients were discharged to outpatient therapy within a week of surgery. Following surgery each patient was given a prescription for oxycodone 5 mg q4-6 PRN pain for 4 weeks with 0 refills. None of the study population requested nor received prescription refills past the original prescription.
Outpatient PT protocol
The timeline of a postoperative rehabilitation course after a total knee replacement is as follows: (I) acute inpatient PT lasts 1 to 3 days; (II) outpatient PT lasting 1 to 6 weeks focusing on passive range of motion (ROM), normal ambulation, and improving quadriceps strength; (III) returning to normal, everyday activity in 4 to 8 weeks (14). The modalities used for each patient were previously published as the multimodal approach (15). Discharge from PT occurs when the therapist determines the patient has reached maximum medical improvement, where there is no longer a benefit of continued PT, or has returned to an everyday functional level of activity.
Outcome measure classifications
Pain levels were measured on a numerical rating scale of 0–10 with 0 being no pain present and 10 being “worst pain imaginable”. A minimum difference of 2 was designated as the threshold for minimal clinically important difference (MCID) (16-18). Patients who were included for readmission to PT were done so if the treating Orthopedic surgeon wrote an additional prescription following the initial course of treatment following TKA. Typically, some of the patient reasons for readmission could include increased pain, decreased ROM, or instability.
Statistical analysis
Q-lag was defined as a loss of 15 degrees or more of active knee extension from baseline patient-specific extension. All patient data were assessed via patient charts prior to surgery and at presentation to PT. Baseline active extension was calculated as the mean of patient recorded active extension at each clinic visit and prior to surgery. All data points were assessed for normality via visual inspection of Normal Q-Q plot and of their histograms (16). The harmonic mean was used due to its robustness to significant outliers. An independent sample t-test was conducted to compare means of dependent variables. The Levene’s test was conducted post-hoc to assess homogeneity of variance in which a P value >0.05 was required to accept the null hypothesis that there was no difference in variance between the two groups. In assessing the means, a two-tailed P value <0.05 was considered the threshold for statistical significance. All analyses were conducted using SPSS version 24 (IBM corporation, Armonk, New York, USA).
Results
Initial analysis of group demographics demonstrated no significant difference in patient age (62.7 vs. 63.4 years; P=0.579), body mass index (BMI) (32.86 vs. 33.21 kg/m2; P=0.915) and gender composition (72.5% women and 27.5% men vs. 76.3% women and 23.7% men; P=0.618) between the two groups (Table 2). Evaluation of active extension lag demonstrated a mean Q-lag of 17.1 degrees (range, 15.0–30.0 degrees) amongst the cohort with Q-lag of 5.7 degrees (range, 0.0–10.0 degrees) amongst the cohort with no Q-lag. While there were no significant differences in pre-operative active ROM (107.5 vs. 109.8 degrees; P=0.321), there was a demonstrable difference in pre-operative passive ROM between the two groups (114.1 vs. 117.6 degrees; P=0.046).
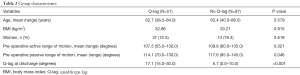
Full table
Chi square analysis demonstrated no significant difference in rates of PT readmission between TKA patients who presented with Q-lag, and patients who did not have Q-lag (23.5% vs. 13.4%; P=0.118) (Table 3). Analysis of mean pain scores between the groups demonstrated a MCID and statistically significant different mean pain scores at dates of last follow-up (1.9 vs. 3.9; P=0.043).

Full table
Discussion
Despite the effectiveness of TKA, patients may fail to achieve full pre-surgical active ROM post-operatively. Predisposition to this phenomenon has been well described in the literature and has been attributed to the progressive degenerative changes present in progressive knee arthritis. Additionally, soft tissue and bone damage sustained during a TKA procedure plays a role in the development of active extension lag (Q-lag) through pain inhibition of active muscle motor units. While the underlying etiology of Q-lag associated with knee arthritis and TKA has been described, there is an absence of literature comparing mid-term outcomes of TKA patients with and without Q-lag. This study compares the readmission rates, and pain scores of 150 consecutive TKA patients (mean follow-up of 30.7 months) who were discharged from PT with Q-lag of 15 degrees or more. Our results demonstrate no difference in readmission rates; however, did show a clinically statistical difference in pain at date of last follow-up.
There were some limitations that existed in this study. This study is retrospective in nature and is thus limited in its ability to control for hidden confounders. These confounders include patient motivation and pre-operative patient recovery expectation (19) . Fortunately, patient pre-operative ROM did not play a role in outcomes. This is evidenced by the fact that there was no significant difference between in pre-operative ROM between the two groups. Additionally, pain is multifactorial in origin and while validated measures such as the Visual Analog Scale exist (20), these measures do not account for psychosocial factors that may influence perception of pain. We therefore encourage future investigators to assess factors influencing perception of pain as it pertains to TKA patients. Despite the study limitations, this study is the first of its kind and may be used to guide orthopaedic care for post-operative TKA patients with Q-lag.
While the literature is scarce on the evaluation of Q-lag after TKA, there are studies which assessed factors associated with reduced quadriceps strength and activation. Ishii et al. (21) preformed a randomized control trial evaluating long-term quadriceps strength in bilateral TKA patients who received cruciate-retaining (CR) implants on one side and posterior stabilizing (PS) design mobile-bearing implants on the other. A cohort of 68 knees (34 patients) were compared to a cohort of 70 knees (35 patients) age matched controls assessing for mean quadriceps strength using a dynamometer. The results demonstrated significantly lower mean muscle strength to body weight ratio (MS/BW) for CR and PS knees, when compared to age matched controls (3.3 vs. 3.4 vs. 4.6; P=0.0032). The study in conjunction with our current research demonstrates the continued need to improve quadriceps strength following TKA.
Thomas et al. (22) assessed quadriceps strength and activation following TKA. A cohort of ten TKA patients was compared to ten control subjects. Their results revealed that quadriceps strength was greater in controls compared to patients at pre-operative (surgical limb vs. control, P<0.001; nonsurgical limb vs. control, P=0.021), 1-month (surgical limb vs. control, P<0.001; nonsurgical limb vs. control, P=0.008), and 6-month time periods (surgical limb vs. control, P<0.001; nonsurgical limb vs. control, P=0.027). Mizner et al. (14) measured pre-and-post operative quadriceps strength and voluntary muscle activation in 20 TKA patients. The authors reported a 62% and 17% mean decrease in quadriceps strength and voluntary activation respectively (P<0.01). Furthermore, the authors revealed that failure of voluntary muscle activation and significant muscle atrophy explained 85% of the loss in quadriceps strength.
It is also important to understand the economic importance of our findings. In recent years there have growing efforts to systematically reduce care costs related to arthroplasty (23-28). A frequent target for these efforts has been to minimize post-acute care costs (29) (i.e., PT) manifested as increasingly shorter duration of care provider directed PT (30). As such, many patients may be fitted towards a PT regimen that falls short of their expected functional outcomes. While our study demonstrated no difference in readmission rates, the difference in pain, albeit small, is of clinical significance and may warrant discussion on models best aimed at reducing costs while optimizing patient outcome during the post-acute period.
Conclusions
This study compared short-term outcomes of patients with and without 15 degrees of Q-lag. This study reveals no statistical significant difference in readmission rates between the two groups; however, clinically significant increased pain levels were found. As such, it is paramount for arthroplasty surgeons and physical therapists to focus patients on restoring quadriceps strength in order to optimize outcomes and reduce patient pain (31). Larger prospective studies are necessary to validate our findings.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Chen PQ, Cheng CK, Shang HC, et al. Gait analysis after total knee replacement for degenerative arthritis. J Formos Med Assoc 1991;90:160-6. [PubMed]
- König A, Walther M, Kirschner S, et al. Balance sheets of knee and functional scores 5 years after total knee arthroplasty for osteoarthritis: a source for patient information. J Arthroplasty 2000;15:289-94. [Crossref] [PubMed]
- Thomas AC, Stevens-Lapsley JE. Importance of attenuating quadriceps activation deficits after total knee arthroplasty. Exerc Sport Sci Rev 2012;40:95-101. [Crossref] [PubMed]
- Moxley Scarborough D, Krebs DE, Harris BA. Quadriceps muscle strength and dynamic stability in elderly persons. Gait Posture 1999;10:10-20. [Crossref] [PubMed]
- Brown M, Sinacore DR, Host HH. The relationship of strength to function in the older adult. J Gerontol A Biol Sci Med Sci 1995;50:55-9. [PubMed]
- Mizner RL, Petterson SC, Snyder-Mackler L. Quadriceps strength and the time course of functional recovery after total knee arthroplasty. J Orthop Sports Phys Ther 2005;35:424-36. [Crossref] [PubMed]
- Moreland JD, Richardson JA, Goldsmith CH, et al. Muscle weakness and falls in older adults: a systematic review and meta-analysis. J Am Geriatr Soc 2004;52:1121-9. [Crossref] [PubMed]
- Noble PC, Gordon MJ, Weiss JM, et al. Does total knee replacement restore normal knee function? Clin Orthop Relat Res 2005.157-65. [Crossref] [PubMed]
- Lieb FJ, Perry J. Quadriceps function. An anatomical and mechanical study using amputated limbs. J Bone Joint Surg Am 1968;50:1535-48. [Crossref] [PubMed]
- Stillman BC. Physiological quadriceps lag: its nature and clinical significance. Aust J Physiother 2004;50:237-41. [Crossref] [PubMed]
- Palmieri-Smith RM, Thomas AC, Karvonen-Gutierrez C, et al. Isometric quadriceps strength in women with mild, moderate, and severe knee osteoarthritis. Am J Phys Med Rehabil 2010;89:541-8. [Crossref] [PubMed]
- Petterson SC, Barrance P, Buchanan T, et al. Mechanisms underlying quadriceps weakness in knee osteoarthritis. Med Sci Sports Exerc 2008;40:422-7. [Crossref] [PubMed]
- Tai TW, Chang CW, Lai KA, et al. Effects of tourniquet use on blood loss and soft-tissue damage in total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am 2012;94:2209-15. [Crossref] [PubMed]
- Mizner RL, Petterson SC, Stevens JE, et al. Early quadriceps strength loss after total knee arthroplasty. The contributions of muscle atrophy and failure of voluntary muscle activation. J Bone Joint Surg Am 2005;87:1047-53. [Crossref] [PubMed]
- McGinn T, Chughtai M, Khlopas A, et al. Early Outpatient Physical Therapy May Improve Range-of-Motion in Primary Total Knee Arthroplasty. J Knee Surg 2017;30:618-21. [Crossref] [PubMed]
- Childs JD, Piva SR, Fritz JM. Responsiveness of the numeric pain rating scale in patients with low back pain. Spine (Phila Pa 1976) 2005;30:1331-4. [Crossref] [PubMed]
- Farrar JT, Young JP, LaMoreaux L, et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 2001;94:149-58. [Crossref] [PubMed]
- Ostelo RW, de Vet HC. Clinically important outcomes in low back pain. Best Pract Res Clin Rheumatol 2005;19:593-607. [Crossref] [PubMed]
- Mahomed NN, Liang MH, Cook EF, et al. The importance of patient expectations in predicting functional outcomes after total joint arthroplasty. J Rheumatol 2002;29:1273-9. [PubMed]
- Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analog scale for measurement of acute pain. Acad Emerg Med 2001;8:1153-7. [Crossref] [PubMed]
- Ishii Y, Noguchi H, Sato J, et al. Quadriceps strength impairment in the mid- to long-term follow-up period after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2017;25:3372-7. [Crossref] [PubMed]
- Thomas AC, Judd DL, Davidson BS, et al. Quadriceps/hamstrings co-activation increases early after total knee arthroplasty. Knee 2014;21:1115-9. [Crossref] [PubMed]
- Siddiqi A, White PB, Mistry JB, et al. Effect of Bundled Payments and Health Care Reform as Alternative Payment Models in Total Joint Arthroplasty: A Clinical Review. J Arthroplasty 2017;32:2590-7. [Crossref] [PubMed]
- Delanois RE, Gwam CU, Mistry JB, et al. Does gender influence how patients rate their patient experience after total hip arthroplasty? Hip Int 2018;28:40-43. [Crossref] [PubMed]
- Gwam C, Mistry J, Delanois R, et al. Does Patient Perception of Pain Influence How Patients Rate Their Experience after Total Knee Arthroplasty? J Knee Surg 2017;30:622-6. [Crossref] [PubMed]
- G Gwam CU, Mistry JB, Mohamed N, et al. Does Age Influence How Patients Rate Their Experience of Care after Total Knee Arthroplasty? J Knee Surg 2017;30:647-51. [Crossref] [PubMed]
- Chughtai M, Patel NK, Gwam CU, et al. Do Press Ganey Scores Correlate With Total Knee Arthroplasty-Specific Outcome Questionnaires in Postsurgical Patients? J Arthroplasty 2017;32:S109-12. [Crossref] [PubMed]
- Etcheson JI, Gwam CU, George NE, et al. Opioids Consumed in the Immediate Post-Operative Period Do Not Influence How Patients Rate Their Experience of Care After Total Hip Arthroplasty. J Arthroplasty 2018;33:1008-11. [Crossref] [PubMed]
- Burwell SM. Setting Value-Based Payment Goals — HHS Efforts to Improve U.S. Health Care. N Engl J Med 2015;372:897-9. [Crossref] [PubMed]
- For Bundled Payments to Work, Doctors Need to Think Different. Available online: https://catalyst.nejm.org/bundled-payments-work-think-different/
- Fishbain DA, Gao J, Lewis JE, et al. At Completion of a Multidisciplinary Treatment Program, Are Psychophysical Variables Associated with a VAS Improvement of 30% or More, a Minimal Clinically Important Difference, or an Absolute VAS Score Improvement of 1.5 cm or More? Pain Med 2016;17:781-9. [PubMed]


