Effects of patient positioning on respiratory mechanics in mechanically ventilated ICU patients
Introduction
Patients admitted to the ICU for acute respiratory failure frequently required intubation and invasive mechanical ventilation. In the early stage of management the invasive mechanical ventilation is commonly delivered in a semi-recumbent supine position under sedation with or without neuromuscular blockade. Changing position is important to break through the routine monotonic delivery of mechanical ventilation and to favor the clearance of respiratory secretions, the prevention of pressure sores and ventilator acquired pneumonia, and the improvement in lung volume and oxygenation. On top of that, in the acute respiratory distress syndrome (ARDS), the early and prolonged prone positioning has been found to increase survival in selected patients (1).
Changing position is extremely common during the daily life including nighttime sleep of normal humans. Investigating the effect of body position has always been a field of great interest for the respiratory physiologists and the physicians as well. As an example, Milic-Emili in the early ’60s of the previous century described the distribution of ventilation in humans in different positions (2). Anesthesiologists have studied for many years the effect of various positions (lateral, prone) during general anesthesia on respiratory mechanics, lung volume and gas exchange in different surgical settings (thoracic, abdominal, spine surgery) in subjects with normal lungs. In the critically ill patients the data are scarcer, probably because the expected changes were thought as being small or not relevant, or because investigating body position changes was sought as of secondary interest. Most of the studies about effects of positioning, furthermore, concentrated on oxygenation and a few on respiratory mechanics. Impairment in respiratory mechanics is associated with the severity and the nature of gas exchange abnormalities in acute respiratory failure. Respiratory mechanics assessment is, moreover, important to adjust the ventilator settings and follow the time course of the disease. The change in position can affect respiratory mechanics by changing resistance and/or compliance of the respiratory system and its lung and chest wall components, and by changing static lung volume and either its components and regional distribution. With new tools available at the bedside, like electrical impedance tomography (EIT), the regional distribution of lung ventilation can be easily measured at different body positions in the critically ill.
In this chapter we will briefly summarize the main findings regarding respiratory mechanics in normal humans in different body positions, then describe the effect of semi-recumbent, lateral and prone position on respiratory mechanics in ICU patients under invasive mechanical ventilation. We will also discuss about driving pressure and transpulmonary pressure, which are currently receiving a great attention, and on the effect of positive end expiratory pressure (PEEP) in the supine and the prone position in ARDS patients.
Respiratory mechanics in normal subjects in different positions
In the supine position, functional residual capacity (FRC) decreases from the sitting position in normal subjects breathing spontaneously. This was also found in healthy persons mechanically ventilated under general anesthesia, in whom FRC decreased from 2.91 to 2.10 L in sitting and supine positions, respectively (3).
In normal humans breathing spontaneously, from sitting to supine the pressure volume (PV) curve of the chest wall is going to change while that of the lungs does not that much. Therefore, the PV curve of the respiratory system follows that of the chest wall during the position change. The relaxation (or resting) volume of the chest wall goes down from 55% to 35% of the vital capacity (VC) and that of the respiratory system from 35% to 20% VC between upright and supine position (4). In patients breathing spontaneously, for any given volume above FRC the elastic pressures of chest wall and respiratory system are positive in the supine position as compared to the upright position and greater in the former than in the latter. The main determinant of the changes in chest wall elastic properties with change in position is the abdominal pressure. Between upright and supine, the abdominal pressure at residual volume (0% VC) is −20 and +1 cmH2O, respectively. This latter finding together with resting volumes change described above make that the compliance of the abdomen, and hence of the chest wall, is higher in supine than in upright position.
In normal young subjects breathing spontaneously, from seated to supine lung compliance decreased from 210 to 160 mL/cmH2O and airway resistance increased from 1.78 to 2.50 cmH2O/L/s. It should be mentioned that under those conditions the upper airways, including larynx and oropharynx, play a role in the measured airway resistance. In patients receiving invasive mechanical ventilation, these factors are obviously not implicated.
In the lateral position FRC averaged 2.44 L in normal subjects under general anesthesia, lung compliance 190 mL/cmH2O and airway resistance 2.50 cmH2O/L/s (3). The measurements being done at the airway opening do not reflect regional change in respiratory mechanics. In the lateral position it is expected that dependent lung EELV decreases, airway resistance and lung and chest wall elastance increase with opposite findings to the nondependent lung as compared to supine (Figure 1). As resistance and elastance depend on lung volume the above findings may be explained by change in lung volume in lateral position. In normal subjects under general anesthesia FRC is larger in the right than in the left lung in the left lateral position.
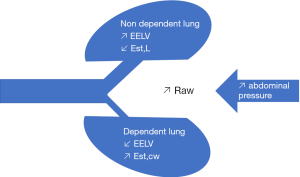
In the prone position FRC was 2.45 L on average in healthy persons under general anesthesia, i.e., similar as in the lateral position and higher than in the supine position. Prone position should allow a better fitting of the lung into the chest wall, reverts the gravity effect along the vertical gradient, and partly relieves the compression of the lungs due to the mediastinum and heart weight (5). In prone position the abdominal content is displaced and, depending on the abdominal compliance, the abdominal pressure increases, and part of it can be transmitted into the chest wall and may impair its elastic properties.
Effects of seated and upright position on lung volumes and respiratory mechanics in the critically ill
Lung volumes
Normal values of FRC in supine and sitting positions have been provided by Ibanez et al. many years ago (6). In ARDS patients, upright position (>45° trunk elevation and <45° legs down) can improve end-expiratory lung volume (EELV) in some patients (7). The improvement of EELV was associated with a better oxygenation (7). A prospective multicenter study investigated the effects of supine at 15° and 45° in 40 ARDS patients and found higher EELV (normalized for the predicted body weight) in supine 45° than in supine 15° (8).
The end-expiratory lung impedance (EELI) measured with EIT increased with the elevation of the head of the bed from 0° to 30° in mechanically ventilated patients after cardiac surgery under pressure support ventilation (9). This increase was mostly due to the dorsal lung regions. In the most anterior part of the lung, EELI did not change when sitting.
Respiratory mechanics
Sedated patients
Martinez et al. systematically investigated the effects of different inclinations in 35 adult patients sedated and mechanically ventilated in the ICU (10). Even though the precise characteristics of patients investigated were not so clear, they found that, as compared to 45° and 60° head inclinations, airway resistance was maximal at 0°, averaging 11.6 cmH2O/L/S at 0.67 L/s inflation flow. The 30° position was associated with the highest dynamic compliance (16.4 mL/cmH2O) (10). The static elastance of the respiratory system averaged 27.1 and 27.0 mL/cmH2O at 0° and 30° inclination, respectively (10).
ARDS patients
Richard et al. investigated the effects of bed maximal verticalization to reach a near erect position (>45° trunk elevation and <45° legs down) in 16 ARDS patients and found that the recruited volume increased as compared to the supine position in those who improved oxygenation while it did not in non-responders (7). In ARDS patients, upright position (head of the bed angle >45°) was associated with an improvement of oxygenation despite no change in respiratory system compliance (11). Respiratory system compliance decreased in supine 45° vs. supine 15° in 40 ARDS patients probably as a result of the increase in abdominal pressure (8). Lung and chest wall mechanics was not assessed in this study.
Weaning patients
The impact of semi recumbent (thorax inclination of 50°±5°, in the bed) and semi-seated (thorax inclination of 67°±5°, out of bed) has been investigated in 34 patients during the weaning process from mechanical ventilation (pressure support 11.5 cmH2O, PEEP 5.7 cmH2O) (12). Surprisingly, respiratory mechanics was not altered by the change of position, notably in terms of dynamic compliance, minute ventilation and respiratory rate to tidal volume ratio. In addition, blood gas was similar (12). On the contrary, in a population of difficult to wean patients during pressure support ventilation (pressure support 15 cmH2O, PEEP 5 cmH2O), a bed inclination of 45° was associated with a reduction of the work of breathing (0.43 vs. 0.50 J/L at 0° and 0.56 J/L at 90°) and of the pressure-time product of the respiratory muscles (102 vs. 114 cmH2O·sec/min at 0° and 116 cmH2O·sec/min at 90°) (13). However, airway resistance and mean airway pressure were similar in all positions (13).
Obese patients
In patients with a body mass index greater than 35 kg/m2, sitting position with an angulation of 70°, was associated with a reduction of the expiratory flow limitation at ZEEP (59% of the tidal volume vs. 0%), auto-PEEP (10 vs. 1.2 cmH2O) and plateau pressure (22 vs. 15.6 cmH2O) as compared to supine position (14). The impact of supine position was not clinically significant with the use of external PEEP except for plateau pressure (24 vs. 16.5 cmH2O) (14).
Effects of lateral position on lung volumes and respiratory mechanics in the critically ill
Critically ill patients can be manually turned laterally during the prone position maneuver for a few minutes, or left longer in lateral position for preventing pressure sores or treating atelectasis. Modern ICU beds propose an automatic rotation of the patients at a given inclination and more advanced devices provide with a continuous lateral rotation with steep lateral position.
Lung volumes
There is no data on lung volumes in the lateral position in ICU patients to our knowledge.
Respiratory mechanics
Transient lateral position
Thomas et al. (15) showed a decrease in respiratory compliance, independently of the presence of lung infiltrate. No change in oxygenation was found.
We recently reported our results of the continuous monitoring of the respiratory mechanics during the prone position maneuver in a series of ARDS patients (16). Respiratory mechanics was measured breath by breath by using the classic least square regression fitting on the signals of pressure and flow. This technique is highly accurate in patients under sedation and paralysis as those we studied. Lateral position was associated with an immediate rise in airway resistance by 2 cmH2O/L/s and in chest wall and lung elastance by 3 and 2 cmH2O/L, respectively. The changes were similar in left or right lateral position (16).
Automated rotation
In terms of respiratory mechanics one study found a significant reduction in respiratory system compliance at the time a steep lateral position was reached (17). The magnitude of the effect was the same at both right and left sides.
Effects of prone position on lung volumes and respiratory mechanics in ARDS
As prone position is an intervention that has been shown to improve survival (1,18) its effect on respiratory mechanics might be implicated in the patient outcome. We will see that these effects are complex and it is not so clear we can capture a scenario that would explain the better survival observed in trials from the change in respiratory mechanics in prone.
Lung volumes
A few studies measured EELV in supine and prone position in ARDS patients, by using the helium dilution technique. These studies consistently found higher values of EELV in prone as compared to supine position: 1,290±570 vs. 1,170±410 mL (P>0.05) (19), 1,570±720 vs. 1,400±640 mL (P<0.01) (20), and 1,480±130 vs. 1,030±90 mL (P<0.01) (21). As CT scan studies demonstrated that prone position induced lung recruitment and reduced lung overdistension (22), it is highly likely that the increase in EELV found in above studies reflected lung recruitment.
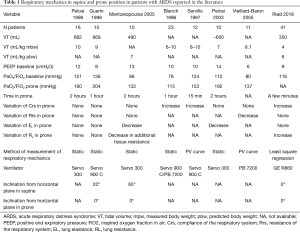
Respiratory mechanics
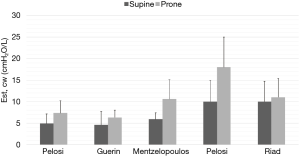
Chest wall elastance
As ARDS patients under invasive mechanical ventilation are proned there should be less compression of the lungs from the weight of mediastinum and heart and also from the heavy sponge-like ARDS lung (23). Furthermore, the anterior chest wall is now lying on the mattress and may receive part of the increase in abdominal pressure that stems from proning. All together these factors should result in higher chest wall elastance in prone as compared to supine position. Indeed, the increase in chest wall elastance in the prone position has been consistently found in ARDS patients in five studies done over the last 20 years (Figure 2). It should be noted that in the study by Mentzelopoulos et al. (21) the increase in prone was statistically significant from supine only for tidal volume greater than 0.6 L. Whilst chest wall elastance is not commonly measured, respiratory system elastance or compliance (=1/elastance) can be measured in routine in ARDS patients. The results regarding the change in respiratory system compliance in prone position in ARDS patients are not consistent across the eight studies reported over the last 20 years (16,19-21,24-27), some studies showing an increase and others no change or a decrease (Table 1). Assuming a systematic increase in chest wall elastance in prone, one would conclude that lung elastance would not change, increase or decrease if respiratory system elastance decreases by the same magnitude, decreases more than chest wall elastance or does not change, respectively. Pelosi et al. (19) showed that the variation in prone position of chest wall compliance was correlated to the variation of oxygenation (reflected by PaO2/FiO2), namely oxygenation increased in prone as much as chest wall compliance decreased.
Full table
In a recent study on the very short term effects of the prone position maneuver on respiratory mechanics we confirmed the increase of chest wall elastance between supine and prone position both at 0° inclination (16).
Driving pressure
It is the difference between plateau pressure and total PEEP. It is very attractive at this moment for two reasons. First, a very sophisticated statistical post-hoc analysis showed that driving pressure, computed as plateau pressure minus PEEP, was the strongest predictor of hospital mortality (28). Second, as driving pressure is the ratio of tidal volume to compliance, and as compliance is related to aerated lung mass, driving pressure could reflect lung strain (29). In our recent short term study the driving pressure of the respiratory system did not change significantly in prone position (16). It is worth notice that the accurate computation of driving pressure requires measuring PEEP at zero flow and is sensitive to the end-inspiratory plateau pressure time of measurement (30).
Trans-pulmonary pressure
In the prone position, as discussed above, the respiratory driving pressure may be less precise than in the supine position because the chest wall elastance changes, and hence the plateau pressure may include a chest wall component. Therefore, the measurement of the trans-pulmonary driving pressure is more relevant. Mentzelopoulos et al. demonstrated in ARDS patients that transpulmonary driving pressure (defined as the difference between end-inspiratory and end-expiratory transpulmonary pressure at zero flow) was reduced with prone position with 0° inclination (as compared to sitting position), which should indicate a reduction in lung strain (21). In a canine model of acute lung injury induced by hypervolemia that mostly resulted in increased abdominal pressure, Mutoh et al. (31) showed a reduction of pleural pressure in the dependent part of the lungs and a homogenization in pleural pressure gradient throughout the lungs. Assuming a constant airway opening pressure this result should indicate an increase of transpulmonary pressure in the dependent lung regions, a more homogeneous distribution of transpulmonary pressure and the reopening of lung units in the dependent part of the lungs in prone position. With the rapid growing interest in the esophageal pressure in the critically ill (32) more studies should be done in the field.
Effect of PEEP on respiratory mechanics in prone position
The interaction between PEEP and prone position remains of the utmost interest in ARDS patients but data are surprisingly limited. As in supine position, the “ideal” PEEP, which simply does not exist, has not been found in prone position. In pigs whose lungs were injured with oleic acid the nadir of the gain in oxygenation after a recruitment maneuver was maintained in prone position at PEEP 15 cmH2O but neither in prone PEEP 8 nor in supine PEEP 15 (33). Therefore, it has been concluded that prone position would act as a PEEP of 7 cmH2O in terms of oxygenation effects (33). However, in humans with ARDS PEEP and prone position had additive (and not synergistic) effects. Indeed, Gainnier et al. (34) demonstrated that the interaction of PEEP and prone position did not alter significantly oxygenation. The oxygenation, assessed from PaO2/FiO2, was systematically better in prone than in supine at any level of PEEP but the difference in PaO2/FiO2 between both positions was similar across the PEEP levels (34). The effect of PEEP in either position was significant for diffuse ARDS but not for focal ARDS (34). In this study PaO2/FiO2 ratio was on average always lower than 150 mmHg in supine position at any PEEP whilst in prone position it was systematically greater than 150 mmHg from PEEP 5 cmH2O (34). This indicates that oxygenation can be easily improved at low PEEP in prone position. Vieillard-Baron et al. (27) confirmed the additive effect of PEEP and prone position on oxygenation at PEEP of 6 cmH2O. They also found that prone position was able to reintegrate lung units with long-time constants into the ventilation.
A new concept recently came out which consisted of setting the PEEP in order to reach a positive trans-pulmonary end expiratory pressure (35). This would reflect the reopening of some lung units in particular these in the dependent parts of the lungs. Data with this strategy in prone position are ongoing (36).
The issue of oxygenation in ARDS is currently much less important as compared to the prevention of ventilator-induced lung injury. This latter is, however, beyond the scope of this chapter. However, as discussed above the driving pressure is an indirect marker of strain.
In patients under general anesthesia for scheduled surgery (37), rising PEEP from 6 to 12 cmH2O in the prone position was associated with a reduction of derecruitment or overdistension (evaluated on compliance-volume curve).
To sum up
Table 2 summarizes the impact of positions on the respiratory system mechanics.
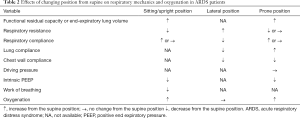
Full table
Supine position (lying flat) or lateral position do not seem beneficial for critically ill patients in terms of respiratory mechanics. The sitting position (with thorax angulation >30° from the horizontal plane) is associated with improvement of FRC, oxygenation and reduction of work of breathing. There is a critical angle of inclination in the seated position above which the increase in abdominal pressure contributes to increase chest wall elastance and offset the increase in FRC.
The nature and magnitude of the effects of prone position on respiratory mechanics should not explain per se the effects of proning on mortality in severe ARDS patients. Two reasons may explain this hypothesis. The first is that the resolution of the methods to measure respiratory mechanics may miss important regional effects, like stress and strain homogenization, that is major contributor of ventilator-induced lung injury prevention and hence patient outcome. It is also worth of notice that studies on the effects of prone position on respiratory mechanics were done more than a decade ago, with tidal volume greater than 6 mL/kg predicted body weight for most of them, inclination in both supine and prone position not defined, and small number of patients (less than 20 most of the time). The second is that other factors than respiratory mechanics can result from proning with beneficial impact on patient outcome like hemodynamics effects. The impact of prone position on respiratory mechanics is complex. The increase in chest wall elastance is a central mechanism of the impact of prone position on respiratory mechanics. Angulation may have an important role by modulating the effect of the abdominal content on the chest wall mechanics.
Perspectives
Clearly additional studies are needed regarding the effects of prone position on respiratory mechanics to take into account limitations previously discussed.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Guerin C, Reignier J, Richard JC, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 2013;368:2159-68. [Crossref] [PubMed]
- Milic-Emili J, Henderson JA, Dolovich MB, et al. Regional distribution of inspired gas in the lung. J Appl Physiol 1966;21:749-59. [Crossref] [PubMed]
- Lumb AB, Nunn JF. Respiratory function and ribcage contribution to ventilation in body positions commonly used during anesthesia. Anesth Analg 1991;73:422-6. [Crossref] [PubMed]
- Agostoni E, Hyatt R. Static behavior of the respiratory system. In: Fishman AP, Macklem PT, Mead J, et al. editors. Handbook of physiology. The respiratory system. Bethesda: Williams, Wilkins, 1986:113-30.
- Albert RK, Hubmayr RD. The prone position eliminates compression of the lungs by the heart. Am J Respir Crit Care Med 2000;161:1660-5. [Crossref] [PubMed]
- Ibanez J, Raurich JM, Moris SG. A simple method for measuring the effect of PEEP on functional residual capacity during mechanical ventilation. Crit Care Med 1982;10:332-4. [Crossref] [PubMed]
- Richard JC, Maggiore SM, Mancebo J, et al. Effects of vertical positioning on gas exchange and lung volumes in acute respiratory distress syndrome. Intensive Care Med 2006;32:1623-6. [Crossref] [PubMed]
- Dellamonica J, Lerolle N, Sargentini C, et al. Effect of different seated positions on lung volume and oxygenation in acute respiratory distress syndrome. Intensive Care Med 2013;39:1121-7. [Crossref] [PubMed]
- Spooner AJ, Corley A, Sharpe NA, et al. Head-of-bed elevation improves end-expiratory lung volumes in mechanically ventilated subjects: a prospective observational study. Respir Care 2014;59:1583-9. [Crossref] [PubMed]
- Martinez BP, Marques TI, Santos DR, et al. Influence of different degrees of head elevation on respiratory mechanics in mechanically ventilated patients. Rev Bras Ter Intensiva 2015;27:347-52. [Crossref] [PubMed]
- Hoste EA, Roosens CD, Bracke S, et al. Acute effects of upright position on gas exchange in patients with acute respiratory distress syndrome. J Intensive Care Med 2005;20:43-9. [Crossref] [PubMed]
- Thomas P, Paratz J, Lipman J. Seated and semi-recumbent positioning of the ventilated intensive care patient - effect on gas exchange, respiratory mechanics and hemodynamics. Heart Lung 2014;43:105-11. [Crossref] [PubMed]
- Deye N, Lellouche F, Maggiore SM, et al. The semi-seated position slightly reduces the effort to breathe during difficult weaning. Intensive Care Med 2013;39:85-92. [Crossref] [PubMed]
- Lemyze M, Mallat J, Duhamel A, et al. Effects of sitting position and applied positive end-expiratory pressure on respiratory mechanics of critically ill obese patients receiving mechanical ventilation*. Crit Care Med 2013;41:2592-9. [Crossref] [PubMed]
- Thomas PJ, Paratz JD, Lipman J, et al. Lateral positioning of ventilated intensive care patients: a study of oxygenation, respiratory mechanics, hemodynamics, and adverse events. Heart Lung 2007;36:277-86. [Crossref] [PubMed]
- Riad Z, Mezidi M, Subtil F, et al. Short-term Effects of the Prone Positioning Manoeuver on Lung and Chest Wall Mechanics in ARDS Patients. Am J Respir Crit Care Med 2018;197:1355-8. [Crossref] [PubMed]
- Schellongowski P, Losert H, Locker GJ, et al. Prolonged lateral steep position impairs respiratory mechanics during continuous lateral rotation therapy in respiratory failure. Intensive Care Med 2007;33:625-31. [Crossref] [PubMed]
- Gattinoni L, Carlesso E, Taccone P, et al. Prone positioning improves survival in severe ARDS: a pathophysiologic review and individual patient meta-analysis. Minerva Anestesiol 2010;76:448-54. [PubMed]
- Pelosi P, Tubiolo D, Mascheroni D, et al. Effects of the prone position on respiratory mechanics and gas exchange during acute lung injury. Am J Respir Crit Care Med 1998;157:387-93. [Crossref] [PubMed]
- Pelosi P, Bottino N, Chiumello D, et al. Sigh in supine and prone position during acute respiratory distress syndrome. Am J Respir Crit Care Med 2003;167:521-7. [Crossref] [PubMed]
- Mentzelopoulos SD, Roussos C, Zakynthinos SG. Prone position reduces lung stress and strain in severe acute respiratory distress syndrome. Eur Respir J 2005;25:534-44. [Crossref] [PubMed]
- Cornejo RA, Diaz JC, Tobar EA, et al. Effects of prone positioning on lung protection in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 2013;188:440-8. [Crossref] [PubMed]
- Gattinoni L, Pesenti A, Carlesso E. Body position changes redistribute lung computed-tomographic density in patients with acute respiratory failure: impact and clinical fallout through the following 20 years. Intensive Care Med 2013;39:1909-15. [Crossref] [PubMed]
- Guerin C, Badet M, Rosselli S, et al. Effects of prone position on alveolar recruitment and oxygenation in acute lung injury. Intensive Care Med 1999;25:1222-30. [Crossref] [PubMed]
- Blanch L, Mancebo J, Perez M, et al. Short-term effects of prone position in critically ill patients with acute respiratory distress syndrome. Intensive Care Med 1997;23:1033-9. [Crossref] [PubMed]
- Servillo G, Roupie E, De Robertis E, et al. Effects of ventilation in ventral decubitus position on respiratory mechanics in adult respiratory distress syndrome. Intensive Care Med 1997;23:1219-24. [Crossref] [PubMed]
- Vieillard-Baron A, Rabiller A, Chergui K, et al. Prone position improves mechanics and alveolar ventilation in acute respiratory distress syndrome. Intensive Care Med 2005;31:220-6. [Crossref] [PubMed]
- Amato MB, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 2015;372:747-55. [Crossref] [PubMed]
- Chiumello D, Carlesso E, Cadringher P, et al. Lung stress and strain during mechanical ventilation for acute respiratory distress syndrome. Am J Respir Crit Care Med 2008;178:346-55. [Crossref] [PubMed]
- Mezidi M, Yonis H, Aublanc M, et al. Effect of end-inspiratory plateau pressure duration on driving pressure. Intensive Care Med 2017;43:587-9. [Crossref] [PubMed]
- Mutoh T, Guest RJ, Lamm WJ, et al. Prone position alters the effect of volume overload on regional pleural pressures and improves hypoxemia in pigs in vivo. Am Rev Respir Dis 1992;146:300-6. [Crossref] [PubMed]
- Akoumianaki E, Maggiore SM, Valenza F, et al. The application of esophageal pressure measurement in patients with respiratory failure. Am J Respir Crit Care Med 2014;189:520-31. [Crossref] [PubMed]
- Cakar N, der Kloot TV, Youngblood M, et al. Oxygenation response to a recruitment maneuver during supine and prone positions in an oleic acid-induced lung injury model. Am J Respir Crit Care Med 2000;161:1949-56. [Crossref] [PubMed]
- Gainnier M, Michelet P, Thirion X, et al. Prone position and positive end-expiratory pressure in acute respiratory distress syndrome. Crit Care Med 2003;31:2719-26. [Crossref] [PubMed]
- Talmor D, Sarge T, Malhotra A, et al. Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med 2008;359:2095-104. [Crossref] [PubMed]
- Mezidi M, Aublanc M, Perinel-Ragey S, et al. Impact of PEEP and body inclination in the supine and prone positions on esophageal pressure in ARDS patients. Ann Intensive Care 2017;7:O33.
- Spaeth J, Daume K, Goebel U, et al. Increasing positive end-expiratory pressure (re-)improves intraoperative respiratory mechanics and lung ventilation after prone positioning. Br J Anaesth 2016;116:838-46. [Crossref] [PubMed]


