Non-invasive ventilation in cardiogenic pulmonary edema
Introduction
Non-invasive ventilation (NIV) refers to the provision of mechanical respiratory support using techniques that do not bypass the upper airway. NIV is now the recommended first-line method of ventilator support in selected patients with acute respiratory failure (ARF) of various origins, including hypercapnic patients with exacerbations of chronic obstructive pulmonary disease (COPD), cardiogenic pulmonary edema (CPE), or immunosuppression, and it has also been suggested as a tool to prevent post-extubation ARF in selected cohorts of critically ill patients (1). The proliferation of NIV over the last decades has been driven by the desire to prevent the complications associated with endotracheal intubation (ETI) and invasive ventilation, including trauma to the upper airway, infections of the respiratory tract, cardiovascular disorders, aspiration of gastric content, and inability to communicate verbally (2-4). In some patient populations with ARF, NIV have been demonstrated to decrease invasive mechanical ventilation rates, shorten hospital stay and improve survival. NIV is generally delivered by using a combination of pressure support ventilation (PSV) plus positive end-expiratory pressure (PEEP). Unlike NIV, continuous positive airway pressure (CPAP) does not deliver ventilation per se because it does not assist inspiration. CPE is one of the most common causes of ARF in the acute care setting and often requires ventilatory assistance. The following sections deal with the pathophysiology of ARF in patients with CPE and the cardiovascular effects of positive airway pressure in these patients. Currently available equipment and techniques used to deliver NIV or CPAP are also described.
Background
In the past, non-invasive modes of mechanical ventilation have been accomplished through various devices including negative and positive pressure ventilators. Negative pressure ventilation was the main strategy for delivering mechanical ventilation outside the operating room during the first half of the 20th century. However, negative pressure ventilation showed a number of disadvantages, including patient discomfort, lack of airway protection, restrictions on positioning, and problems with portability. Accordingly, negative pressure ventilators have seen diminishing use in favor of positive pressure assistance modes since the early 1960s.
It was in 1912 that Bunnell (5) firstly applied a non-invasive treatment of positive airway pressure. He could maintain lung expansion in a patient during thoracic surgery by means of a face mask. The first reports of non-invasive application of positive pressure to treat respiratory failure caused by cardiac impairment dates to the 1930s (6). Several studies conducted by Barach et al. (7,8) over the 1930s showed that CPAP, delivered through a face mask, could be useful in the treatment of CPE and other forms of respiratory failure. Noninvasive positive airway pressure administered through a mouthpiece was first described by Motley (9) in the 1940s and was used widely either for aerosol delivery in patients with COPD and asthma or as a means of ventilatory assistance until the early 1980s, after which its use declined sharply.
The expansion of NIV occurred during the 1980s, after the introduction of mask ventilation in the treatment of patients with obstructive sleep apnea, neuromuscular diseases and chest wall deformities (10-12). Later on, the great success achieved in the management of ARF by using NIV over the 1990s’ (13-16) encouraged investigation on various applications of this technique in the acute care setting. In the last decades, the possibility to avoid complications related to ETI and invasive mechanical ventilation in patients threatened by severe impairment in gas exchange, has represented the most relevant driving force for the increased use of NIV, both in the clinical and research setting.
Utilization rate of NIV
In their 28-day international study undertaken in 2002 on patients admitted to 361 intensive care units (ICUs) who received mechanical ventilation for more than 12 hours, Esteban et al. (17) found that NIV through a facial mask was used in 4.9% of overall patients and in 16.9% of those ventilated because of COPD exacerbation. Similarly, in a prospective 3-week survey of 70 French ICUs in 2002, Demoule et al. (18) showed that 23% of patients requiring ventilatory assistance received NIV as a first-line treatment, a significant increase compared to 1997 (16%) (19). Even the incidence of NIV for patients admitted to the ICU without tracheal intubation was strongly implemented.
Currently, the rate of NIV use in the clinical scenario appears various, mainly due to heterogeneity in physician expertise, respiratory therapist training, and equipment availability (20). In a large observational study conducted on the trends in NIV use among ICU patients with ARF over a 15-year period, Schnell et al. (21) reported that NIV use increased steadily and regarded up to 42% of patients in 2011, and that first-line treatment with NIV was associated with improved survival and reduced ICU-acquired infections, as compared to first-line invasive mechanical ventilation. Other data on NIV use in Francophone countries (22) confirmed an increased NIV use over time, showing however a decline in its application among the subgroup of patients affected by de novo ARF. Importantly, last decades witnessed increasing NIV success rates with progressively lower mortality. Indeed, NIV failure remains more common in patients with de novo ARF, but it appears no longer associated with increased mortality, as in previous years. This may suggest that the greater expertise gained by physicians on NIV physiology, harms and benefits enables better selection of patients, finally allowing tailored treatments yielding improved clinical outcomes.
Benefit of positive airway pressure in CPE: pathophysiology
The pathophysiology of respiratory failure during CPE includes an increase in extravascular lung water, a reduction in lung volume and in respiratory system compliance, and an increase in airway resistance (23). That results in increased work of breathing and oxygen cost of breathing, with the potential for an imbalance between oxygen consumption and oxygen delivery (24,25).
Positive airway pressure provided as CPAP restores functional residual capacity by means of alveolar recruitment, thereby mitigating right-to-left intrapulmonary shunt and improving oxygenation and lung mechanics (26). In COPD patients, CPAP may reduce the work of breathing and relieves dyspnea, mostly by counterbalancing the inspiratory load caused by dynamic hyperinflation with intrinsic PEEP (27).
Effects on hemodynamics during non-invasive airway pressure in patients with left heart failure have been amply described. By lowering left ventricular (LV) transmural pressure in these patients, CPAP may reduce LV afterload without compromising cardiac index (28,29). This is aided by the decreased negative pressure swings produced by the respiratory system.
Also in patients presenting CPE resulting from diastolic dysfunction, the use of positive airway pressure on LV function have been investigated. In patients admitted to the ICU with hypoxemic CPE, Bendjelid et al. (30) suggested that in those patients with preserved LV contractility, the hemodynamic benefit of CPAP on CPE resulted from a decrease in LV end-diastolic volume (preload) following a reduced venous return.
There is considerable evidence that positive airway pressure reduces cardiac output by decreasing venous return (30-33). Total venous return results from a driving pressure gradient and the resistance to venous return. According to Guyton’s theory (34-36), the driving force is the difference between mean systemic filling pressure (Pms) and right atrial pressure (Pra). The Pms, i.e., the equilibrium pressure in the systemic vessels under the condition of no flow, depends on the total volume of blood inside the venous vasculature and the intrinsic compliance of the circulatory system. The blood volume required to fill the vascular bed without any increase in transmural pressure is generally defined as unstressed intravascular volume. Any volume above this level is the stressed volume, which generates an increasing degree of pressure on the venous system. The greater the stressed volume, the greater Pms.
For several years, it has been suggested that positive airway pressure, by increasing Pra, reduces venous return by decreasing the pressure gradient between Pms and Pra (37,38). However, experimental (39) and human (40) studies reported that positive airway pressure equally increased Pra and Pms and altered venous return with no impact on the pressure gradient (Pms − Pra). Accordingly, a decrease in blood flow resulting from the use of positive airway pressure was ascribed to an increased resistance to venous return. This concept was supported by experimental results reported by Brienza et al. (41) who suggested that application of PEEP would decrease blood flow not only by an increase in the liver venous back pressure to flow, but also by an increase in venous resistance caused by a compression of the liver by the diaphragm.
NIV in CPE: evidence base
The largest multicenter trial on the use of NIV in patients with ARF due to CPE was published in 2008 by Gray et al. (42) who randomized 1069 patients from 26 emergency departments in the United Kingdom to receive standard oxygen therapy, CPAP (5–15 cmH2O), or NIV (inspiratory pressure, 8–20 cmH2O; expiratory pressure, 4–10 cmH2O). In that study, non-invasive ventilatory support delivered by either CPAP or NIV showed earlier resolution of dyspnea, respiratory distress, and metabolic alterations than did conventional oxygen therapy, even though these effects did not result in improved rates of survival. Subsequently, five systematic reviews (43-47) concluded that NIV decreases the need for intubation and hospital mortality, and that NIV and CPAP have similar effects on the main outcomes. Additionally, although an early trial suggested greater risk of myocardial infarction with NIV than with CPAP (48), none of the subsequent trials confirmed that finding.
Over time, a lot of literature has accumulated on the use of CPAP or bilevel NIV to prevent deterioration in patients with ARF due to CPE in the pre-hospital setting (49-51). However, although some studies demonstrated that NIV improved physiological variables and symptoms and decreased ETI incidence and in-hospital mortality compared with usual medical therapy, these effects were inconsistent. Indeed, favorable results varied among studies, suggesting potential differences in experience of the personnel on ambulances or patients’ severity. That prevents a firm recommendation on the use of NIV for CPE prior to hospitalization.
Finally, NIV has been proposed as a prophylactic tool to facilitate weaning from invasive mechanical ventilation (preventive NIV) and as rescue treatment before re-intubation during acute hypoxemic failure after extubation (rescue NIV). Some authors showed increased mortality in unselected cohorts of patients receiving NIV during ARF after extubation, possibly due to delayed re-intubation as compared to standard oxygen therapy (52,53). By contrast, among hypoxemic patients with higher likelihood of weaning failure due to cardiac insufficiency, early application of NIV immediately after extubation appears effective in preventing post-extubation ARF (54,55). In patients undergoing invasive mechanical ventilation because of CPE and who are at high risk of developing ARF after extubation, use of non-invasive positive pressure techniques as a preventive strategy to avoid reintubation may help maintaining positive airway pressure after removal of the endotracheal tube, thus facilitating ventilator weaning process.
NIV: practical tips
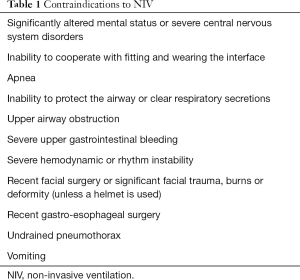
In the acute setting, treatment with NIV should be started as soon as clinical parameters indicate upcoming respiratory failure: clinical parameters driving treatment initiation include gas exchange abnormalities associated to dyspnea, tachypnea, accessory muscles use and/or paradoxical abdominal breathing. Contraindications to NIV are summarized in Table 1.
Full table
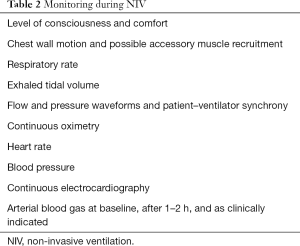
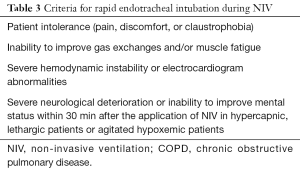
Performing a close monitoring (Table 2) in an appropriate location is of primary importance for NIV success. Monitoring of patients receiving NIV helps the clinician determine whether NIV is being applied safely and effectively. Devices and personnel for ETI should be readily available in case of NIV failure. Criteria for discontinuing NIV and initiating invasive mechanical ventilation are shown in Table 3.
Full table
Full table
Interfaces
Interfaces for NIV enable sealed connection of the ventilator circuit to patients airways, thereby allowing delivery of pressure/flow into the lung. Choice of the proper interface is amongst the most relevant issues to ensure NIV success. Alternating available interfaces may represent an effective approach to optimize comfort and tolerance, especially in patients undergoing prolonged treatments.
The nasal mask (Figure 1) is a triangular or cone-shaped clear plastic device that fits over the nose by a soft cushion or flange. Because of the pressure exerted over the bridge of the nose, the mask may generate skin irritation, redness and, eventually, ulceration. Several types of strap systems are available to hold the mask in place. Depending on the interface, straps attach at two or as many as five points on the mask and may be provided with Velcro fasteners. A nasogastric tube may be passed through a seal connector in the dome of the mask to prevent gastric distension.
Oronasal or face masks (Figure 2) cover both the mouth and the nose. Oronasal masks can be suggested when air leaks exist during nasal NIV. Importantly, most acutely ill patients require NIV due to dyspnea and high respiratory demand and are mouth breathers, predisposing to greater air leakage during nasal mask NIV. The “full face” mask represents an evolution of the oronasal interface (Figure 3); it is made of clear plastic and uses a soft silicone flange that seals around the perimeter of the face, permitting the avoidance of applying direct pressure to the most delicate facial structures.
The standard helmet (Figure 4) is a transparent hood covering the patient’s whole head. Positive pressure in the system makes a soft collar seal comfortable to neck and shoulders, finally limiting air leakage, especially when higher pressure is set and delivered. The whole apparatus is connected to a mechanical ventilator by a standard respiratory circuit. Two ports in the helmet act as inlet and outlet for inspiratory and expiratory limbs of the circuit, and a specific connector placed in the plastic ring allows passage of nasogastric tubes. With this interface, the patient interacts with the environment, is able to cough and can drink through a straw or be fed by liquid diet. The main advantages of the helmet include: possible delivery of higher PEEP/CPAP without air leaks, good tolerability and comfort, lower risk of dermal lesions and easier applicability to any patient regardless of the face contour.
NIV modes and CPAP
NIV is generally delivered by using a combination of PSV and PEEP. PSV is a pressure-targeted, flow-cycled mode of ventilation that assists spontaneous breathing by delivering a preset inspiratory pressure. A sensitive trigger causes the delivery of inspiratory pressure support throughout inspiration, and a reduction in inspiratory flow drives the machine to cycle into expiration. Therefore, the patient can control either inspiratory duration or breathing rate.
Other ventilator modes may be used to deliver NIV. In bilevel positive airway pressure (BiPAP), a valve sets two pressure levels, the expiratory positive airway pressure (EPAP) level, and the inspiratory positive airway pressure (IPAP) level so that ventilation is produced by the cyclic delta pressure between IPAP and EPAP.
In the mandatory controlled mechanical ventilation (CMV) mode, no patient effort is required, as full ventilatory support is provided. In this mode, ventilator settings include inflation pressure or tidal volume, frequency, and the timing of each breath. In assist/control (A/C) ventilation, the machine delivers a tidal volume either when triggered by the patient (assist) or when the patient’s inspiratory effort does not occur within a given period (control). In A/C ventilation, volume-cycled and pressure-targeted modes are available.
In neurally adjusted ventilatory assist (NAVA), the ventilator adjusts mechanical assistance to the electrical activity of the diaphragm (EAdi), which can estimate the respiratory drive and trigger on and cycle off the delivery of ventilator assistance (56).
Unlike NIV, CPAP does not deliver ventilation per se because it does not assist inspiration, but rather delivers a constant pressure by means of constant flow throughout the entire respiratory cycles. Because spontaneous breathing is not supported, this technique requires effective respiratory drive and maintained alveolar ventilation. CPAP can be applied by various devices, namely low gas flow generators with reservoir, high-flow jet venturi circuits, and bilevel and critical care ventilators.
Low levels of airway pressure (generally <4 cmH2O) may also be achieved during treatments with high-flow nasal cannula. These levels are proportional to gas flow and are enhanced during preferential nose breathing (57,58).
Selecting the ventilation mode
Each ventilation mode has theoretical advantages and limitations. In the absence of evidence suggesting a proper ventilatory mode for each patient category, the choice of the ventilatory strategy should be driven by caregiver and patient related factors: these include personal experience, treatment setting, etiology, and pathophysiology of the respiratory failure. As a rule of thumb, assisted modes, particularly PSV, are usually well tolerated and can be safely and effectively performed. Similarly to invasive mechanical ventilation, in COPD patients, external PEEP counterbalances the effects of dynamic hyperinflation and limits the degree of isometric work of breathing due to intrinsic PEEP. During disease exacerbation, NIV allows respiratory muscle unloading, lowers arterial partial pressure of carbon dioxide (PaCO2) and significantly improves clinical outcome (59). Volume-control ventilation can be useful in patients with severe chest wall deformity or obesity, in whom higher inflation pressure may be required. During assisted ventilation, flow-based inspiratory triggering reduces breathing effort as compared to pressure triggering, enabling improved patient-ventilator interaction (60).
Spontaneously breathing patients with respiratory failure of different origins may benefit from non-invasive CPAP or PSV to correct hypoxemia. In a physiological study on hypoxemic patients with ARF, when compared to low-flow oxygen therapy, non-invasive PSV with PEEP was demonstrated to improve oxygenation and relieve dyspnea, finally lowering respiratory drive and inspiratory effort (61). In these patients, CPAP used alone improved oxygenation but was unable to provide any respiratory muscles unloading.
In patients with acute CPE, a growing body of evidence supports the use of non-invasive respiratory assistance as a first line intervention. Bilevel NIV has the potential advantage over CPAP of assisting the patient during inspiration, with relief of dyspnea and improvement of vital signs (48). However, these physiological benefits were not translated into primary outcomes in clinical studies, which did not report significant differences between CPAP and bilevel NIV in terms of ETI or survival (1). In this context, the potential differences in hemodynamic changes resulting from the application of CPAP or bilevel NIV have not been investigated.
CPAP might be considered the preferred intervention, as it is easy-to-use, cheap and simple to set up, also in clinical settings different from the ICU. However, the actual importance of these advantages of CPAP over bilevel NIV in patients with ARF due to CPE has not been confirmed.
Ventilator setting
In pressure-targeted ventilation, low pressure should be initially delivered to enhance patient’s tolerance (appropriate initial pressures are with CPAP of 3–5 cmH2O and inspiratory pressure of 8–12 cmH2O above CPAP). Afterwards, if necessary, these can be gradually increased, as tolerated, to deliver adequate tidal volumes [between 6 and 8 mL/kg predicted body weight (PBW)], relieve dyspnea, reduce respiratory rate and ensure good patient-ventilator interaction. Commonly, administered CPAP levels in hypoxemic ARF patients range from 5 to 12 cmH2O and oxygen supplementation is titrated to an oxygen saturation between 92% and 98%, or between 88% and 92% in patients at risk of hypercapnia (i.e., exacerbation of chronic respiratory failure).
How to deal with carbon dioxide rebreathing and patient-ventilator asynchrony
When CPAP is delivered by helmet, the inspired partial pressure of CO2 is independent from CPAP level, rather being inversely correlated to the amount of delivered fresh gas flow (62). Fresh gas flow exceeding 35–40 L/min makes CO2 rebreathing clinically irrelevant during helmet CPAP. Compared to CPAP, helmet-delivered PSV NIV provides more efficient CO2 washout, due to a higher inspiratory flow during such ventilatory mode and the assistance of patient’s inspiration. Of note, CO2 rebreathing during helmet-delivered PSV is not limited by increasing the level of inspiratory assistance (63).
During NIV, patient-ventilator asynchrony includes ineffective triggering, double-triggering, auto-triggering, premature cycling, and delayed cycling. Asynchronies result in increased work of breathing, patient discomfort and intolerance (64). When PSV is delivered, some forms of patient-ventilator asynchrony may occur, causing breathing discomfort. Possible air leaks during non-invasive PSV may impede the adequate reduction in inspiratory flow required to activate the expiratory trigger, thus prolonging the delivery of inspiratory flow. In these circumstances, air leaks should be minimized by optimizing the interface, or even switching to another type of interface. To reduce air leaks and ineffective triggering related to dynamic hyperinflation, it may also be helpful to decrease ventilator pressure, if it is compatible with clinical conditions. In case of air leaks, an option to obtain a better patient-ventilator interaction is to select pressure-targeted, time-cycled modes, or even PSV mode with a maximal inspiratory time. Furthermore, when provided by the ventilator, raising the cycling off airflow threshold of expiratory trigger can activate an earlier switchover to expiration, thus avoiding prolonged insufflations. Modern NIV algorithms can measure and compensate air leaks in order to improve patient-machine synchrony.
In selecting the optimal ventilator setting, the caregiver should take into account the type of interface used to deliver NIV with a view to facilitating patient-ventilator interaction. When the helmet is used, the pressure administrated by the machine is partially spent to pressurize the inner volume of the interface, resulting in a lower level of mechanical assistance in the initial phase of the inspiratory effort. In addition, given the technical characteristics of the helmet, also expiratory trigger efficiency may be unfavorably affected, thus worsening patient-ventilator asynchronies. Accordingly, during helmet ventilation, use of higher flows and higher pressures may reduce the compliance of the helmet, thus lessening asynchronies. It has been suggested that the highest PEEP and PS levels clinically indicated and tolerated by the patient along with the highest pressurization rate should be used when NIV is applied with the helmet, with the aim to increase the elastance of the system and enhance the trigger sensitivity (65,66). In patients receiving helmet NIV for postextubation hypoxemic ARF, NAVA has been shown to improve patient-ventilator interaction and reduce asynchronies compared with PSV (67).
Predictors of failure of NIV
Predictors of NIV failure observed in hypoxemic patients with ARF are the following:
- High severity score [Simplified Acute Physiology Score (SAPS) II ≥35 (68)/SAPS II >34 (69)/higher SAPS II (70)];
- Older age (>40 years) (68);
- Presence of ARDS or CAP (68,70,71);
- Failure to improve oxygenation after 1 hour of treatment [ratio of partial pressure arterial oxygen (PaO2) and fraction of inspired oxygen (FiO2) ≤146 mmHg (68)/PaO2:FiO2 ≤175 mmHg (69)];
- Higher respiratory rate under NIV (71);
- Need for vasopressors (71);
- Need for renal replacement therapy (71);
- Expired tidal volume above 9.5 mL/kg predicted body weight (PBW) in patients with PaO2/FiO2 ≤200 mmHg (72).
Humidification during NIV
Despite early physiological findings supporting the use of heated humidifiers (HHs) over heat and moisture exchangers (HMEs) in reducing the work of breathing and enhancing CO2 clearance in patients undergoing NIV (73,74), a multicenter RCT found no differences between HHs and HMEs in terms of NIV duration, ICU and hospital length of stay, or ICU mortality (75).
Conclusions
NIV or CPAP should be considered as a first-line strategy in the management of patients with CPE because both techniques have been proven to decrease the need for ETI and hospital mortality in these patients. The pathophysiological rationale is strong, as they decrease the systemic venous return and the LV afterload, thus reducing LV filling pressure and limiting pulmonary edema. In the management of CPE patients with respiratory failure, CPAP and NIV may be used interchangeably, as they have shown similar effects on the main outcomes.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Rochwerg B, Brochard L, Elliott MW, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J 2017;50. [Crossref] [PubMed]
- Zwillich CW, Pierson DJ, Creagh CE, et al. Complications of assisted ventilation. Am J Med 1974;57:161-70. [Crossref] [PubMed]
- Stauffer JL, Olson DE, Petty TL. Complications and consequences of endotracheal intubation. Am J Med 1981;70:65-76. [Crossref] [PubMed]
- Pingleton SK. Complications of acute respiratory failure. Am Rev Respir Dis 1988;137:1463-93. [Crossref] [PubMed]
- Bunnell S. The use of nitrous oxide and oxygen to maintain anesthesia and positive pressure for thoracic surgery. Cal State J Med 1910;8:11-4. [PubMed]
- Poulton EP, Oxon DM. Left-sided heart failure with pulmonary oedema: Its treatment with the “pulmonary plus pressure machine.” Lancet 1936;231:981-3. [Crossref]
- Barach AL, Martin J, Eckman M. Positive-pressure respiration and its application for the treatment of acute pulmonary edema and respiratory obstruction. Proc Am Soc Clin Invest 1937;16:664-80.
- Barach AL, Swenson P. Effect of breathing gases under positive pressure on lumens of small and medium-sized bronchi. Arch Int Med 1939;63:946-8. [Crossref]
- Motley HL, Lang LP, Gordon B. Use of intermittent positive pressure breathing combined with nebulization in pulmonary disease. Am J Med 1948;5:853-6. [Crossref] [PubMed]
- Sullivan CE, Issa FG, Berthon-Jones M, et al. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet 1981;1:862-5. [Crossref] [PubMed]
- Ellis ER, Bye PT, Bruderer JW, et al. Treatment of respiratory failure during sleep in patients with neuromuscular disease: positive-pressure ventilation through a nose mask. Am Rev Respir Dis 1987;135:148-52. [PubMed]
- Bach JR, Alba AS. Management of chronic alveolar hypoventilation by nasal ventilation. Chest 1990;97:52-7. [Crossref] [PubMed]
- Brochard L, Isabey D, Piquet J, et al. Reversal of acute exacerbations of chronic obstructive lung disease by inspiratory assistance with a face mask. N Engl J Med 1990;323:1523-30. [Crossref] [PubMed]
- Bersten AD, Holt AW, Vedig AE, et al. Treatment of severe cardiogenic pulmonary edema with continuous positive airway pressure delivered by face mask. N Engl J Med 1991;325:1825-30. [Crossref] [PubMed]
- Antonelli M, Conti G, Rocco M, et al. A comparison of noninvasive positive-pressure ventilation and conventional mechanical ventilation in patients with acute respiratory failure. N Engl J Med 1998;339:429-35. [Crossref] [PubMed]
- Antonelli M, Conti G, Bufi M, et al. Noninvasive ventilation for treatment of acute respiratory failure in patients undergoing solid organ transplantation. JAMA 2000;283:235-41. [Crossref] [PubMed]
- Esteban A, Anzueto A, Frutos F, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA 2002;287:345-55. [Crossref] [PubMed]
- Demoule A, Girou E, Richard JC, et al. Increased use of noninvasive ventilation in French intensive care units. Intensive Care Med 2006;32:1747-55. [Crossref] [PubMed]
- Carlucci A, Richard JC, Wysocki M, et al. Noninvasive versus conventional mechanical ventilation. An epidemiologic survey. Am J Respir Crit Care Med 2001;163:874-80. [Crossref] [PubMed]
- Maheshwari V, Paioli D, Rothaar R, et al. Utilization of noninvasive ventilation in acute care hospitals: a regional survey. Chest 2006;129:1226-33. [Crossref] [PubMed]
- Schnell D, Timsit JF, Darmon M, et al. Noninvasive mechanical ventilation in acute respiratory failure: trends in use and outcomes. Intensive Care Med 2014;40:582-91. [Crossref] [PubMed]
- Demoule A, Chevret S, Carlucci A, et al. Changing use of noninvasive ventilation in critically ill patients: trends over 15 years in francophone countries. Intensive Care Med 2016;42:82-92. [Crossref] [PubMed]
- Sharp JT, Griffith GT, Bunnell IL, et al. Ventilatory mechanics in pulmonary edema in man. J Clin Invest 1958;37:111-7. [Crossref] [PubMed]
- Aubier M, Trippenbach T, Roussos C. Respiratory muscle fatigue during cardiogenic shock. J Appl Physiol 1981;51:499-508. [Crossref] [PubMed]
- Field S, Kelly SM, Macklem PT. The oxygen cost of breathing in patients with cardiorespiratory disease. Am Rev Respir Dis 1982;126:9-13. [PubMed]
- Katz JA, Marks JD. Inspiratory work with and without continuous positive airway pressure in patients with acute respiratory failure. Anesthesiology 1985;63:598-607. [Crossref] [PubMed]
- Petrof BJ, Legere M, Goldberg P, et al. Continuous positive airway pressure reduced work of breathing and dyspnea during weaning from mechanical ventilation in severe chronic obstructive pulmonary disease. Am Rev Respir Dis 1990;141:281-9. [Crossref] [PubMed]
- Räsänen J, Heikkilä J, Downs J, et al. Continuous positive airway pressure by face mask in acute cardiogenic pulmonary edema. Am J Cardiol 1985;55:296-300. [Crossref] [PubMed]
- Naughton MT, Rahman MA, Hara K, et al. Effect of continuous positive airway pressure on intrathoracic and left ventricular transmural pressures in patients with congestive heart failure. Circulation 1995;91:1725-31. [Crossref] [PubMed]
- Bendjelid K, Schütz N, Suter PM, et al. Does continuous positive airway pressure by face mask improve patients with acute cardiogenic pulmonary edema due to left ventricular diastolic dysfunction? Chest 2005;127:1053-8. [Crossref] [PubMed]
- Dhainaut JF, Devaux JY, Monsallier JF, et al. Mechanisms of decreased left ventricular preload during continuous positive pressure ventilation in ARDS. Chest 1986;90:74-80. [Crossref] [PubMed]
- Schuster S, Erbel R, Weilemann LS, et al. Hemodynamics during PEEP ventilation in patients with severe left ventricular failure studied by transesophageal echocardiography. Chest 1990;97:1181-9. [Crossref] [PubMed]
- Leithner C, Podolsky A, Globits S, et al. Magnetic resonance imaging of the heart during positive end-expiratory pressure ventilation in normal subjects. Crit Care Med 1994;22:426-32. [Crossref] [PubMed]
- Guyton AC. Determination of cardiac output by equating venous return curves with cardiac response curves. Physiol Rev 1955;35:123-9. [Crossref] [PubMed]
- Guyton AC, Lindsey AW, Abernathy B, et al. Venous return at various right atrial pressures and the normal venous return curve. Am J Physiol 1957;189:609-15. [Crossref] [PubMed]
- Magder S. Volume and its relationship to cardiac output and venous return. Crit Care 2016;20:271. [Crossref] [PubMed]
- Cournand A, Motley HL, Werkio L, et al. Physiological studies of the effects of intermittent positive pressure breathing on cardiac output in man. Am J Physiol 1948;152:162-74. [Crossref] [PubMed]
- Braunwald E, Binion JT, Morgan WL, et al. Alterations in central blood volume and cardiac output induced by positive pressure breathing counteracted by metaraminol (Aramine). Circ Res 1957;5:670-5. [Crossref] [PubMed]
- Fessler HE, Brower RG, Wise RA, et al. Effects of positive end-expiratory pressure on the gradient for venous return. Am Rev Respir Dis 1991;143:19-24. [Crossref] [PubMed]
- Nanas S, Magder S. Adaptations of the peripheral circulation to PEEP. Am Rev Respir Dis 1992;146:688-93. [Crossref] [PubMed]
- Brienza N, Revelly JP, Ayuse T, et al. Effects of PEEP on liver arterial and venous blood flows. Am J Respir Crit Care Med 1995;152:504-10. [Crossref] [PubMed]
- Gray A, Goodacre S, Newby DE, et al. Noninvasive ventilation in acute cardiogenic pulmonary edema. N Engl J Med 2008;359:142-51. [Crossref] [PubMed]
- Potts JM. Noninvasive positive pressure ventilation: effect on mortality in acute cardiogenic pulmonary edema: a pragmatic meta-analysis. Pol Arch Med Wewn 2009;119:349-53. [PubMed]
- Weng CL, Zhao YT, Liu QH, et al. Meta-analysis: noninvasive ventilation in acute cardiogenic pulmonary edema. Ann Intern Med 2010;152:590-600. [Crossref] [PubMed]
- Mariani J, Macchia A, Belziti C, et al. Noninvasive ventilation in acute cardiogenic pulmonary edema: a meta-analysis of randomized controlled trials. J Card Fail 2011;17:850-9. [Crossref] [PubMed]
- Vital FM, Ladeira MT, Atallah AN. Non-invasive positive pressure ventilation (CPAP or bilevel NPPV) for cardiogenic pulmonary oedema. Cochrane Database Syst Rev 2013;5. [PubMed]
- Cabrini L, Landoni G, Oriani A, et al. Noninvasive ventilation and survival in acute care settings: a comprehensive systematic review and metaanalysis of randomized controlled trials. Crit Care Med 2015;43:880-8. [Crossref] [PubMed]
- Mehta S, Jay GD, Woolard RH, et al. Randomized, prospective trial of bilevel versus continuous positive airway pressure in acute pulmonary edema. Crit Care Med 1997;25:620-8. [Crossref] [PubMed]
- Plaisance P, Pirracchio R, Berton C, et al. A randomized study of out-of-hospital continuous positive airway pressure for acute cardiogenic pulmonary oedema: physiological and clinical effects. Eur Heart J 2007;28:2895-901. [Crossref] [PubMed]
- Thompson J, Petrie DA, Ackroyd-Stolarz S, et al. Out-of-hospital continuous positive airway pressure ventilation versus usual care in acute respiratory failure: a randomized controlled trial. Ann Emerg Med 2008;52:232-41. [Crossref] [PubMed]
- Roessler MS, Schmid DS, Michels P, et al. Early out-of-hospital non-invasive ventilation is superior to standard medical treatment in patients with acute respiratory failure: a pilot study. Emerg Med J 2012;29:409-14. [Crossref] [PubMed]
- Keenan SP, Powers C, McCormack DG, et al. Noninvasive positive-pressure ventilation for postextubation respiratory distress: a randomized controlled trial. JAMA 2002;287:3238-44. [Crossref] [PubMed]
- Esteban A, Frutos-Vivar F, Ferguson ND, et al. Noninvasive positive-pressure ventilation for respiratory failure after extubation. N Engl J Med 2004;350:2452-60. [Crossref] [PubMed]
- Nava S, Gregoretti C, Fanfulla F, et al. Noninvasive ventilation to prevent respiratory failure after extubation in high-risk patients. Crit Care Med 2005;33:2465-70. [Crossref] [PubMed]
- Ferrer M, Valencia M, Nicolas JM, et al. Early noninvasive ventilation averts extubation failure in patients at risk: a randomized trial. Am J Respir Crit Care Med 2006;173:164-70. [Crossref] [PubMed]
- Sinderby C, Navalesi P, Beck J, et al. Neural control of mechanical ventilation in respiratory failure. Nat Med. 1999;5:1433-6. [Crossref] [PubMed]
- Parke RL, McGuinness SP. Pressures delivered by nasal high flow oxygen during all phases of the respiratory cycle. Respir Care 2013;58:1621-4. [Crossref] [PubMed]
- Chanques G, Riboulet F, Molinari N, et al. Comparison of three high flow oxygen therapy delivery devices: a clinical physiological cross-over study. Minerva Anestesiol 2013;79:1344-55. [PubMed]
- Vitacca M, Rubini F, Foglio K, et al. Non-invasive modalities of positive pressure ventilation improve the outcome of acute exacerbations in COLD patients. Intensive Care Med 1993;19:450-5. [Crossref] [PubMed]
- Nava S, Ambrosino N, Bruschi C, et al. Physiological effects of flow and pressure triggering during non invasive mechanical ventilation in patients with chronic obstructive pulmonary disease. Thorax 1997;52:249-54. [Crossref] [PubMed]
- L’Her E, Deye N, Lellouche F, et al. Physiologic effects of noninvasive ventilation during acute lung injury. Am J Respir Crit Care Med 2005;172:1112-8. [Crossref] [PubMed]
- Patroniti N, Foti G, Manfio A, et al. Head helmet versus face mask for non-invasive continuous positive airway pressure: a physiological study. Intensive Care Med 2003;29:1680-7. [Crossref] [PubMed]
- Costa R, Navalesi P, Antonelli M, et al. Physiologic evaluation of different levels of assistance during noninvasive ventilation delivered through a helmet. Chest 2005;128:2984-90. [Crossref] [PubMed]
- Kondili E, Prinianakis G, Georgopoulos D. Patient-ventilator interaction. Br J Anaesth 2003;91:106-19. [Crossref] [PubMed]
- Moerer O, Fischer S, Hartelt M, et al. Influence of two different interfaces for noninvasive ventilation compared to invasive ventilation on the mechanical properties and performance of a respiratory system: a lung model study. Chest 2006;129:1424-31. [Crossref] [PubMed]
- Vargas F, Thille A, Lyazidi A, et al. Helmet with specific settings versus facemask for noninvasive ventilation. Crit Care Med 2009;37:1921-8. [Crossref] [PubMed]
- Cammarota G, Olivieri C, Costa R, et al. Noninvasive ventilation through a helmet in postextubation hypoxemic patients: physiologic comparison between neurally adjusted ventilatory assist and pressure support ventilation. Intensive Care Med 2011;37:1943-50. [Crossref] [PubMed]
- Antonelli M, Conti G, Moro ML, et al. Predictors of failure of noninvasive positive pressure ventilation in patients with acute hypoxemic respiratory failure: a multi-center study. Intensive Care Med 2001;27:1718-28. [Crossref] [PubMed]
- Antonelli M, Conti G, Esquinas A, et al. A multiple-center survey on the use in clinical practice of noninvasive ventilation as a first-line intervention for acute respiratory distress syndrome. Crit Care Med 2007;35:18-25. [Crossref] [PubMed]
- Gristina GR, Antonelli M, Conti G, et al. Noninvasive versus invasive ventilation for acute respiratory failure in patients with hematologic malignancies: a 5-year multicenter observational survey. Crit Care Med 2011;39:2232-9. [Crossref] [PubMed]
- Adda M, Coquet I, Darmon M, et al. Predictors of noninvasive ventilation failure in patients with hematologic malignancy and acute respiratory failure. Crit Care Med 2008;36:2766-72. [Crossref] [PubMed]
- Carteaux G, Millán-Guilarte T, De Prost N, et al. Failure of Noninvasive Ventilation for De Novo Acute Hypoxemic Respiratory Failure: Role of Tidal Volume. Crit Care Med 2016;44:282-90. [Crossref] [PubMed]
- Lellouche F, Maggiore SM, Deye N, et al. Effect of the humidification device on the work of breathing during noninvasive ventilation. Intensive Care Med 2002;28:1582-9. [Crossref] [PubMed]
- Jaber S, Chanques G, Matecki S, et al. Comparison of the effects of heat and moisture exchangers and heated humidifiers on ventilation and gas exchange during noninvasive ventilation. Intensive Care Med 2002;28:1590-4. [Crossref] [PubMed]
- Lellouche F, L'Her E, Abroug F, et al. Impact of the humidification device on intubation rate during noninvasive ventilation with ICU ventilators: results of a multicenter randomized controlled trial. Intensive Care Med 2014;40:211-9. [Crossref] [PubMed]






