Impact of sleep apnea on in-hospital outcomes after transcatheter aortic valve replacement: insight from National Inpatient Sample database 2011–2014
Introduction
Surgical aortic valve replacement and transcatheter aortic valve replacement (TAVR) are the only effective therapy for adult patients with symptomatic severe aortic stenosis to offer survival benefit and symptom relief (1). For patients with symptomatic severe aortic stenosis who are at high or prohibitive risk for surgical aortic valve replacement, TAVR is recommended as an alternative treatment based on the evidence from PARTNER (Placement of Aortic Transcatheter Valves) trial (1-7).
Sleep apnea has been shown to be associated with a wide range of cardiopulmonary diseases as well as increased postoperative complications (8-11). Approximately 25% of adult patients presenting for elective surgery might have sleep apnea (12). Accordingly, the American Society of Anesthesiologists recommends preoperative evaluation of obstructive sleep apnea and subsequent sleep study with treatment if necessary (13).
Given the rising prevalence of sleep apnea (14) and rapidly evolving TAVR with its exponentially increasing utilization (15), it is imperative to examine the impact of sleep apnea on postoperative outcomes of TAVR which may have implications for cost-effective preoperative screening and perioperative management of sleep apnea.
Methods
Data source and study population
Data were obtained from the Agency for Healthcare Research and Quality Healthcare Cost and Utilization Project, National Inpatient Sample (NIS) files between 2011 and 2014. NIS is the largest publicly available all-payer inpatient care data in the United States that allows national estimates of hospitalization in a given year. De-identified information for 146,032,189 discharges was contained in NIS during the study period. Institutional Review Board approval and informed consent were not required for this study given the administrative de-identified nature of the database. On the basis of International Classification of Diseases-9th edition-Clinical Modification (ICD-9-CM) codes, each patient data in the NIS has ≤25 diagnoses including one principal diagnosis as well as ≤15 procedures including one principal procedure performed during the same hospitalization. Individual patient’s data in NIS also includes Clinical Classification Software (CCS) codes which groups multiple ICD-9-CM codes into a lesser number of diagnoses and procedures categories to facilitate statistical analyses. We identified study population, patient comorbidities and procedures performed using a combination of ICD-9-CM and CCS codes. Patients (aged ≥18 years) who underwent TAVR from 2011 through 2014 were identified using ICD-9-CM procedure codes of 35.05 and 35.06 recorded in any of the 15 procedures fields. Patients with data missing mortality were excluded.
Study variables
NIS variables were used to examine patient’s age, gender, race, household income quartiles, primary payer, length of stay, in-hospital death and discharge location as well as hospital’s region, location and teaching status. Race was dichotomized into white and nonwhite. The severity of comorbidities was defined by using the Deyo modification of the Charlson Comorbidity Index where higher scores indicate greater burden of comorbidities. Sleep apnea was identified with ICD-9-CM codes of 327.20, 327.21, 327.23, 327.24, 327.26, 327.27, 780.51, 780.53, 780.57 and 786.03. Similar methodology has been previously used to identify patients with sleep apnea (16). Noninvasive ventilator use was captured using ICD-9-CM codes of 93.90 and 93.91 (17). As a postoperative in-hospital outcome measure, primary endpoint was defined as experiencing any complication of all-cause death, stroke (ICD 9 codes 997.00, 997.01, 997.02 and CCS code 109) and acute myocardial infarction (CCS code 100). Secondary endpoint was defined as the occurrence of one or more postoperative complications of acute respiratory failure (ICD 9 codes 518.81, 518.84, 799.1), pneumothorax (ICD 9 code 512.1), vascular complications (ICD 9 codes 900-904, 447, 868.04, 868.14, 998.2, 999.2, 997.7, e870.x, 39.31, 39.41, 39.49, 39.52, 39.53, 39.56, 39.57, 39.58, 39.59, 39.79), hemorrhage requiring transfusion (ICD 9 codes 998.11, 998.12, 285.1 combined with 99.0x), acute kidney injury requiring hemodialysis (ICD 9 codes 584.5, 584.6, 584.7, 584.8, 584.9 combined with 39.95 without principal diagnosis of end stage renal disease; 585.6) or permanent pacemaker implantation (ICD-9 codes 37.80, 37.81, 37.82, 37.83). Length of hospital stay was dichotomized at the 75th percentile of stay days whereby prolonged length of stay was defined as hospital stay exceeding the 75th percentile (16,18). Data for race, household income quartile and primary payer were missing in 7%, 1.5% and 0.2% of the study population, respectively while data for the rest of variables were available in 100% of patients.
Statistical analysis
For all analyses, we followed the recommendations from the Agency for Healthcare Research and Quality by using survey specific statements (e.g., SURVEYFREQ, SURVEYMEANS). Patient-specific and hospital-specific discharge weights were used for inference of national estimates. For subpopulation analyses, we used a domain analysis for accurate variance calculations. All analyses accounted for hospital level clustering of patients and the sampling design using CLUSTER and STRATA statements, respectively.
For descriptive analyses, we compared baseline patient and hospital characteristics between cohorts with and without sleep apnea. Continuous variables are presented as means or medians; categorical variables are showed as frequencies. For comparison of baseline characteristics, either survey specific linear regression or Mann-Whitney U test was used for continuous variables and Rao-Scott χ2 test was used for categorical variables.
To assess the association between sleep apnea and postoperative outcomes, multivariate logistic regression models were created for each outcome by forcing sleep apnea into a stepwise model selection procedure with candidate comorbidity variables using entry and stay criteria of a P value less than 0.25 and 0.1, respectively (19). Candidate variables were included in the model if the variable was significantly associated with outcome (P<0.25) in the univariate logistic model, which were from among age, gender, race, transapical access, smoking, hypertension, diabetes mellitus, dyslipidemia, coronary artery disease, previous PCI, previous CABG, pulmonary hypertension, congestive heart failure, malignancy, peripheral vascular disease, chronic kidney disease, chronic pulmonary disease, anemia, coagulopathy, previous stroke, fluid/electrolyte disorder, obesity, weight loss, Charlson/Deyo comorbidity index, primary payer, household income quartile, hospital region, hospital bed size and hospital location/teaching status. Use of noninvasive ventilation (NIV) is likely to be either a mediator on a causal pathway, if adjusted for, which would falsely obscure possible association between sleep apnea and postoperative outcomes or a collider, if controlled for, which would falsely create spurious association leading to a bias. Hence, we did not include the NIV in the main regression analyses for adjustment. We used a dummy variable adjustment method for missing data for race variable in order to preserve the full sample size (20). Multicollinearity was examined with VIF statement and all the possible two-way interactions were thoroughly tested. Regression model fit was assessed by area under the receiver operator characteristic curves and Hosmer-Lemeshow χ2 statistic.
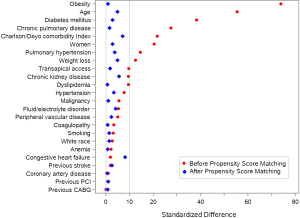
Sensitivity analysis was performed using propensity score method to examine the sensitivity of the primary results to different statistical approaches. To determine each patient’s propensity score of having sleep apnea, a non-parsimonious multivariate logistic regression model (c statistic =0.75) was used including all covariates used in the primary analysis. The propensity score was incorporated as an additional covariate in the primary multivariate logistic regression model to create Model 2. Furthermore, we performed 1:1 matching between cohorts with and without sleep apnea based on propensity score with a caliper width of 0.2 of the standard deviation of the logit of the propensity score using greedy algorithm (21). Standardized differences for all covariates before and after matching were computed to assess the accomplishment of matching where a standardized difference of <10% for each covariate after matching is suggestive of a successful matching (22). For matched group outcome comparisons, conditional logistic regression was used with exact test where appropriate. All tests were two-sided with P values <0.05 indicating statistical significance. SAS statistical software, version 9.4 (SAS institute, Cary, NC, USA) was used for all statistical analyses.
Results
Baseline patient characteristics
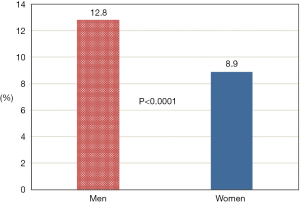
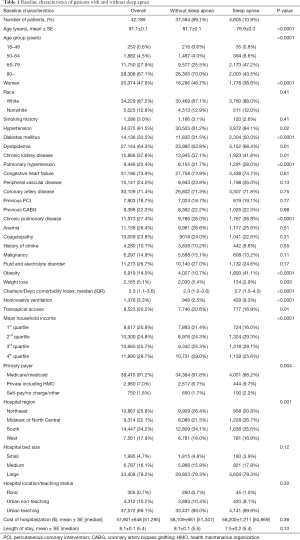
Of 42,189 TAVR patients, 4,605 (10.9%) had sleep apnea and those with obstructive sleep apnea accounted for 85.5% of the entire sleep apnea cohort. Prevalence of sleep apnea was higher in men than women (Figure 1). Patients with sleep apnea were younger, more likely to be male and had higher proportions of hypertension, diabetes, dyslipidemia, pulmonary hypertension, chronic pulmonary disease and obesity with greater Charlson/Deyo comorbidity index score who received transapical access less frequently than those without sleep apnea (Table 1). NIV was more often used in patients with than those without sleep apnea (9.3% vs. 2.5%, P<0.0001).
Full table
Postoperative outcomes stratified by sleep apnea
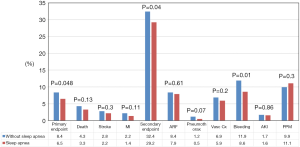
Figure 2 demonstrates observed in-hospital outcomes between cohorts with and without sleep apnea. Sleep apnea patients had lower incidences of primary endpoint, secondary endpoint, and bleeding requiring transfusion than the counterpart.
Association between sleep apnea and postoperative outcomes
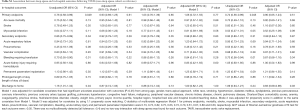
Table S1 presents the unadjusted and adjusted association between sleep apnea and in-hospital outcomes following TAVR. After controlling for covariates, a presence of sleep apnea was no longer statistically significantly associated with any of the examined in-hospital outcomes (Model 1). Multivariate logistic regression adjusting for an additional variable of propensity score showed grossly consistent results (Model 2). Propensity score matching analyses following successful matching (Figure 3) resulted in the similar findings (Model 3). Sleep apnea was independently associated with neither prolonged hospital stay nor discharge disposition. Controlling for the use of NIV rendered consistent results (data not shown). Subgroup analyses confined to obstructive sleep apnea showed grossly consistent findings with the main analyses except for a lower likelihood of discharge to home (Table S1).
Full table
Discussion
The main findings of our study are as follows: First, the prevalence of sleep apnea in patients undergoing TAVR was 10.9%. Second, sleep apnea was not independently associated with worse postoperative outcomes following TAVR. Third, perioperative provision of NIV in patients with sleep apnea was 9.3%.
The prevalence of sleep apnea in TAVR patients is similar to the national estimates in the United States (men: 12.8% vs. 14%, women: 8.9% vs. 5%) that has increased over the past two decades in parallel with rising level of obesity which is the strongest risk factor for sleep apnea (14,23-26). Gender gap of sleep apnea prevalence although still significant was smaller in our study than previous studies that reported the ratio of men to women with sleep apnea to be 2–3 to 1. It is noteworthy that sleep apnea is more prevalent in patients undergoing TAVR than those receiving orthopedic, spinal, general or vascular surgeries based on analyses of national data (16,27,28). Our findings compare to the known association between sleep apnea and multiple comorbidities including hypertension, diabetes mellitus, dyslipidemia, chronic kidney disease, pulmonary hypertension and obesity (26,29-33).
Patients with sleep apnea undergoing surgery may be at increased risk for postoperative complications since anesthesia or analgesia could cause pharyngeal relaxation leading to exacerbation of apnea. A growing body of literature suggests the potential link between sleep apnea and worse postoperative outcomes following cardiac as well as non-cardiac surgeries (9-11,16,27,34). Memtsoudis et al. found a significant independent association between sleep apnea and cardiopulmonary complications after both orthopedic and general surgeries (16,27). Kaw et al. reported an increased risk for postoperative complications in patients with sleep apnea undergoing open heart surgeries (9). Our findings focused on patients undergoing TAVR are in contrast to the aforementioned results from other surgeries. The observed incidences of primary endpoint and secondary endpoint including bleeding were lower, despite their higher burden of comorbidities, in patients with than those without sleep apnea. There are several plausible explanations for these observations. We speculate higher postoperative complication rates in patients without sleep apnea may have been partly contributed by greater utilization of transapical access for TAVR than the counterpart. In numerous studies, transapical access for TAVR was found to be associated with worse outcomes compared with transfemoral access (35-37). In addition, the higher proportion of women in the group without sleep apnea may explain the higher bleeding complications as female gender has been shown to be a predictor of bleeding complications after TAVR in previous studies (38-42). However, after adjusting for all potential confounding factors available in the study, the presence of sleep apnea no longer remained statistically significantly associated with any of the examined in-hospital postoperative outcomes of TAVR. This finding suggests that observed differences in postoperative outcomes between patients with and without sleep apnea were driven by confounders. It is reassuring that in-hospital outcomes are comparable in patients undergoing TAVR regardless of the presence of sleep apnea after adjusting for confounders.
Guidelines from the American Society of Anesthesiologists recommend that patients with sleep apnea on preoperative NIV continue the therapy after surgery (13). Previous studies demonstrated the low frequency of provision of CPAP in the hospital setting (17,43). In our study, utilization of NIV for patients with sleep apnea was only 9.3% although higher than patients without sleep apnea. The lower rate of NIV use would suggest possible room for quality improvement in perioperative management for patients with sleep apnea undergoing TAVR despite currently lacking evidence of the benefit of NIV use on postoperative outcomes.
This is the first study, of which we are aware, that examined the association between sleep apnea and in-hospital outcomes after TAVR with a large population. This study is based on a large real-world data which confers generalizability of the findings. Also, use of different statistical methodologies for the analyses would consolidate the internal validity of our study.
Several important factors need to be noted when interpreting the result of our study. First, the logistic EuroScore and Society of Thoracic Surgeons score were not available in NIS data for adjustment although multivariate regression and propensity score matching achieved adequate balance including Charlson/Deyo index between the two study cohorts. Second, data on types of anesthesia used for TAVR was not available. General anesthesia could potentially interact with sleep apnea on postoperative outcomes although the outcomes of both general anesthesia and local anesthesia were comparable after TAVR (44) that would preclude the type of anesthesia from biasing the association as a confounder. Third, potential misclassification of sleep apnea should be considered given a large proportion of sleep apnea remains undiagnosed when patients present to surgery. Preexisting undiagnosed sleep apnea was prevalent in more than 80% of surgical patients (12,45). This potential non-differential misclassification of sleep apnea could have biased the possible association between sleep apnea and postoperative outcomes toward the null. Nevertheless, the absence of the independent association between sleep apnea and TAVR outcomes in our study is still convincing given that previous studies with the even lower prevalence of sleep apnea still demonstrated worse outcomes after other surgeries in patients with sleep apnea (16,27). Fourth, no detailed clinical information such as post-TAVR aortic regurgitation, site of bleeding and postoperative hemodynamic performance of the valve were available for study. Fifth, the severity of sleep apnea was not accounted for in the absence of information on the apnea-hypopnea index in NIS data.
Conclusions
In patients undergoing TAVR for the treatment of symptomatic severe aortic stenosis, the prevalence of sleep apnea was 10.9%, and the presence of sleep apnea was not independently associated with postoperative in-hospital outcomes in the NIS data of the years from 2011 to 2014.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Institutional Review Board approval and informed consent were not required for this study given the administrative de-identified nature of the database.
References
- Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Thorac Cardiovasc Surg 2014;148:e1-e132. [Crossref] [PubMed]
- Leon MB, Smith CR, Mack M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 2010;363:1597-607. [Crossref] [PubMed]
- Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 2011;364:2187-98. [Crossref] [PubMed]
- Makkar RR, Fontana GP, Jilaihawi H, et al. Transcatheter aortic-valve replacement for inoperable severe aortic stenosis. N Engl J Med 2012;366:1696-704. [Crossref] [PubMed]
- Kodali SK, Williams MR, Smith CR, et al. Two-year outcomes after transcatheter or surgical aortic-valve replacement. N Engl J Med 2012;366:1686-95. [Crossref] [PubMed]
- Mack MJ, Leon MB, Smith CR, et al. 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patients with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet 2015;385:2477-84. [Crossref] [PubMed]
- Vahanian A, Alfieri O, Andreotti F, et al. Guidelines on the management of valvular heart disease (version 2012): the Joint Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Eur J Cardiothorac Surg 2012;42:S1-44. [Crossref] [PubMed]
- Blake DW, Chia PH, Donnan G, et al. Preoperative assessment for obstructive sleep apnoea and the prediction of postoperative respiratory obstruction and hypoxaemia. Anaesth Intensive Care 2008;36:379-84. [PubMed]
- Kaw R, Golish J, Ghamande S, et al. Incremental risk of obstructive sleep apnea on cardiac surgical outcomes. J Cardiovasc Surg (Torino) 2006;47:683-9. [PubMed]
- Gupta RM, Parvizi J, Hanssen AD, et al. Postoperative complications in patients with obstructive sleep apnea syndrome undergoing hip or knee replacement: a case-control study. Mayo Clin Proc 2001;76:897-905. [Crossref] [PubMed]
- Hwang D, Shakir N, Limann B, et al. Association of sleep-disordered breathing with postoperative complications. Chest 2008;133:1128-34. [Crossref] [PubMed]
- Finkel KJ, Searleman AC, Tymkew H, et al. Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic medical center. Sleep Med 2009;10:753-8. [Crossref] [PubMed]
- American Society of Anesthesiologists Task Force on Perioperative Management of patients with obstructive sleep apnea. Practice guidelines for the perioperative management of patients with obstructive sleep apnea: an updated report by the American Society of Anesthesiologists Task Force on Perioperative Management of patients with obstructive sleep apnea. Anesthesiology 2014;120:268-86. [Crossref] [PubMed]
- Peppard PE, Young T, Barnet JH, et al. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 2013;177:1006-14. [Crossref] [PubMed]
- Cribier AG. The Odyssey of TAVR from concept to clinical reality. Tex Heart Inst J 2014;41:125-30. [Crossref] [PubMed]
- Memtsoudis SG, Stundner O, Rasul R, et al. The impact of sleep apnea on postoperative utilization of resources and adverse outcomes. Anesth Analg 2014;118:407-18. [Crossref] [PubMed]
- Spurr KF, Graven MA, Gilbert RW. Prevalence of unspecified sleep apnea and the use of continuous positive airway pressure in hospitalized patients, 2004 National Hospital Discharge Survey. Sleep Breath 2008;12:229-34. [Crossref] [PubMed]
- Memtsoudis SG, Sun X, Chiu YL, et al. Perioperative comparative effectiveness of anesthetic technique in orthopedic patients. Anesthesiology 2013;118:1046-58. [Crossref] [PubMed]
- Greenland S, Mickey RM. Re: "The impact of confounder selection criteria on effect estimation. Am J Epidemiol 1989;130:1066. [Crossref] [PubMed]
- Cohen J, Cohen P, West SG, et al. Missing Variable. In: Riegert D. editor. Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences, 3rd Edition, Lawrence Erlbaum Associates, Inc., Mahwah, New Jersey, 2002:431-50.
- Rubin DB, Thomas N. Matching using estimated propensity scores: relating theory to practice. Biometrics 1996;52:249-64. [Crossref] [PubMed]
- Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 2009;28:3083-107. [Crossref] [PubMed]
- Apovian CM. The Obesity Epidemic--Understanding the Disease and the Treatment. N Engl J Med 2016;374:177-9. [Crossref] [PubMed]
- Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med 2007;357:370-9. [Crossref] [PubMed]
- Young T, Palta M, Dempsey J, et al. Burden of sleep apnea: rationale, design, and major findings of the Wisconsin Sleep Cohort study. WMJ 2009;108:246-9. [PubMed]
- Young T, Skatrud J, Peppard PE. Risk factors for obstructive sleep apnea in adults. JAMA 2004;291:2013-6. [Crossref] [PubMed]
- Memtsoudis S, Liu SS, Ma Y, et al. Perioperative pulmonary outcomes in patients with sleep apnea after noncardiac surgery. Anesth Analg 2011;112:113-21. [Crossref] [PubMed]
- Stundner O, Chiu YL, Sun X, et al. Sleep apnoea adversely affects the outcome in patients who undergo posterior lumbar fusion: a population-based study. Bone Joint J 2014;96-B:242-8. [Crossref] [PubMed]
- Peppard PE, Young T, Palta M, et al. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 2000;342:1378-84. [Crossref] [PubMed]
- Lindberg E, Theorell-Haglow J, Svensson M, et al. Sleep apnea and glucose metabolism: a long-term follow-up in a community-based sample. Chest 2012;142:935-42. [Crossref] [PubMed]
- Adedayo AM, Olafiranye O, Smith D, et al. Obstructive sleep apnea and dyslipidemia: evidence and underlying mechanism. Sleep Breath 2014;18:13-8. [Crossref] [PubMed]
- Nicholl DD, Ahmed SB, Loewen AH, et al. Declining kidney function increases the prevalence of sleep apnea and nocturnal hypoxia. Chest 2012;141:1422-30. [Crossref] [PubMed]
- Sanner BM, Doberauer C, Konermann M, et al. Pulmonary hypertension in patients with obstructive sleep apnea syndrome. Arch Intern Med 1997;157:2483-7. [Crossref] [PubMed]
- Liao P, Yegneswaran B, Vairavanathan S, et al. Postoperative complications in patients with obstructive sleep apnea: a retrospective matched cohort study. Can J Anaesth 2009;56:819-28. [Crossref] [PubMed]
- Li X, Kong M, Jiang D, et al. Comparison 30-day clinical complications between transfemoral versus transapical aortic valve replacement for aortic stenosis: a meta-analysis review. J Cardiothorac Surg 2013;8:168. [Crossref] [PubMed]
- Panchal HB, Ladia V, Amin P, et al. A meta-analysis of mortality and major adverse cardiovascular and cerebrovascular events in patients undergoing transfemoral versus transapical transcatheter aortic valve implantation using edwards valve for severe aortic stenosis. Am J Cardiol 2014;114:1882-90. [Crossref] [PubMed]
- Zhao A, Minhui H, Li X, et al. A meta-analysis of transfemoral versus transapical transcatheter aortic valve implantation on 30-day and 1-year outcomes. Heart Surg Forum 2015;18:E161-6. [Crossref] [PubMed]
- Bière L, Launay M, Pinaud F, et al. Influence of sex on mortality and perioperative outcomes in patients undergoing TAVR: insights from the FRANCE 2 registry. J Am Coll Cardiol 2015;65:755-7. [Crossref] [PubMed]
- O'Connor SA, Morice MC, Gilard M, et al. Revisiting Sex Equality With Transcatheter Aortic Valve Replacement Outcomes: A Collaborative, Patient-Level Meta-Analysis of 11,310 Patients. J Am Coll Cardiol 2015;66:221-8. [Crossref] [PubMed]
- Buchanan GL, Chieffo A, Montorfano M, et al. The role of sex on VARC outcomes following transcatheter aortic valve implantation with both Edwards SAPIEN and Medtronic CoreValve ReValving System(R) devices: the Milan registry. EuroIntervention 2011;7:556-63. [Crossref] [PubMed]
- Van Mieghem NM, Tchetche D, Chieffo A, et al. Incidence, predictors, and implications of access site complications with transfemoral transcatheter aortic valve implantation. Am J Cardiol 2012;110:1361-7. [Crossref] [PubMed]
- Tchetche D, Van der Boon RM, Dumonteil N, et al. Adverse impact of bleeding and transfusion on the outcome post-transcatheter aortic valve implantation: insights from the Pooled-RotterdAm-Milano-Toulouse In Collaboration Plus (PRAGMATIC Plus) initiative. Am Heart J 2012;164:402-9. [Crossref] [PubMed]
- Sorscher AJ, Caruso EM. Frequency of provision of CPAP in the inpatient setting: an observational study: "CPAP provision in the inpatient setting Sleep Breath 2012;16:1147-50. [Crossref] [PubMed]
- Brecker SJ, Bleiziffer S, Bosmans J, et al. Impact of Anesthesia Type on Outcomes of Transcatheter Aortic Valve Implantation (from the Multicenter ADVANCE Study). Am J Cardiol 2016;117:1332-8. [Crossref] [PubMed]
- Singh M, Liao P, Kobah S, et al. Proportion of surgical patients with undiagnosed obstructive sleep apnoea. Br J Anaesth 2013;110:629-36. [Crossref] [PubMed]


