Preclinical atherosclerosis in patients with inflammatory bowel diseases: a case-control study
Introduction
Atherosclerosis is the main condition predisposing to the onset of cardiovascular (CV) events (1). There are some well-recognized risk factors for atherosclerosis development, including hypertension, hypercholesterolemia, diabetes mellitus, current smoking, and obesity (2). Besides these traditional risk factors, a role for chronic inflammation itself has been suggested in the last decade, particularly in patients with rheumatic and inflammatory bowel diseases (IBD) (3,4). This a clinically relevant issue, since immune-mediated mechanisms could early cause atherosclerosis in these patients, even in absence of other CV risk factors (5). However, data are still contentious, particularly for IBD patients. Indeed, a meta-analysis of 11 studies showed no role for chronic inflammation in increasing the CV risk in these patients (6), whilst another by including data of nine studies found an increased risk (7). Therefore, further studies are needed to clarify such a field.
Preclinical arterial wall atherosclerotic damage has been shown to be a reliable surrogate to estimate the CV risk. In detail, carotid artery intima-media thickness (CIMT) may be accurately measured by ultrasound (8), and it is now widely used as an early marker for atherosclerosis (9,10). Indeed, IMT values are predictive of CV events and stroke in individuals without a clinically evident disease (9). We therefore designed this case-control study to assess the CIMT values in patients with IBD without traditional CV risk factors.
Methods
Patients
This was a case-control study involving consecutive patients with an established IBD diagnosis, present for more than 2 years prior to the study, without extra-intestinal manifestations, who were receiving a biologic therapy in our center. Age and sex matched controls were consecutively selected among hospital personnel in the same period. Those patients and controls with a presence of any traditional CV risk factor, including hypertension, hypercholesterolemia, diabetes mellitus, current smoking, and obesity (BMI >30), were excluded.
Carotid artery ultrasound
Doppler ultrasonography was performed, in a quiet semi-dark room, with subjects lying supine with their necks slightly hyper-extended, and rotated away from the imaging transducer. Both carotid arteries were scanned. The right common carotid artery proximal to the bulb was imaged in multiple longitudinal planes for the best resolution of the CIMT of the far wall. CIMT was defined as the distance between the leading edge of the lumen intimal interface and the leading edge of the media adventitia interface of the far wall, measured in end diastole, 1 cm proximal to the bifurcation (8). All examinations were performed by the same experienced investigator (intraobserver variability: r =0.979). CIMT was measured, and values were grouped in the following three classes: normal (CIMT ≤0.9 mm), moderate thickness (CIMT: >0.9 and ≤1.2 mm), and pre-clinical atherosclerosis (CIMT >1.2 mm) (11). The investigator was blinded to the subjects (case or control).
Statistical analysis
Data between groups were compared using the Student’s t-test and Fisher’s exact test, as appropriate. The ORs with their 95% confidence intervals were also calculated, when appropriate. By considering a mean difference of 0.5 mm in the CIMT value between IBD patients (1.1 mm) and controls (0.6 mm) as suggested elsewhere (12), the enrolment of 22 cases for each group allows to detect a significant difference with power of 80% and alfa-error of 5%.
Results
The study enrolled 23 consecutive patients and 20 controls matched for age (mean age: 49.4±10.9 vs. 51±12.4) and sex (male/female: 17/6 vs. 10/10) distribution, meeting the inclusion criteria. IBD group included 16 patients with Ulcerative Colitis and 7 with Crohn’s disease, all in ongoing treatment with biologics, including Infliximab (N=15) and Adalimumab (N=8). The mean of disease duration was 11.7±1.3 years, and the median of biologic therapy was 5 (range, 2–8) years.
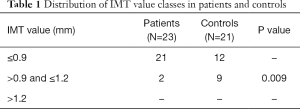
The mean of CIMT values was not statistically different between patients and controls (0.68±0.21 vs. 0.82±0.2 mm; P=0.4). When performing the analysis of distribution, the prevalence of moderate CIMT thickness was significantly lower in cases than in controls (8.7% vs. 42.8%; P=0.01; OR: 0.15, 95% CI: 0.03–0.85). No cases of pre-clinical atherosclerosis (CIMT values >1.2 mm) were observed in both IBD cases and controls (Table 1).
Full table
The mean of CIMT values did not significantly differ between patients with Crohn’s and those with Ulcerative Colitis, although the values tended to be lower in the latter group (0.83±0.22 vs. 0.64±0.19 mm; P=0.07).
Discussion
Atherosclerosis is involved in the onset of both ischemic heart events and strokes, with relevant—and potentially life-threatening—consequences (1,2). Besides the well-established risk factors, a chronic systemic inflammation has been proposed as an essential CV risk factor (13). Indeed, the inflammatory status could contribute to atherosclerosis development through endothelial dysfunction caused by different pro-inflammatory cytokines [tumor necrosis factor (TNF), IL-1, IL-6, etc.] (10). In addition, an important role has been attributed to the high levels of C-reactive protein (CRP), which is involved in the overexpression of adhesion molecules and rupture of the atherosclerotic plaque (14).
There are some data suggesting an independent role of chronic inflammation in the atherosclerotic process in patients with rheumatic diseases, but others failed to confirm the association (15,16). Likewise, the heterogeneity depends on the fact that classical risk factors for atherosclerosis were not taken into account in several studies (14). Similarly, the existence of an accelerated atherosclerosis in IBD patients, purely due to the chronic inflammation, remains controversial based on data of two meta-analysis (6,7). A more recent meta-analysis, including 16 studies, found that IBD patients had a significantly higher CIMT mean values (standardized mean difference: 0.534 mm; 95% CI: 0.230–0.838; P=0.001) as compared to controls (12). However, a very high heterogeneity (I2=87.6%) was present among the studies, which undermines the weight of the results. Moreover, the difference remained statistically significant only for ulcerative colitis, but not for Crohn’s disease patients (12).
To accurately assess whether chronic inflammation itself could play a role in pre-clinical atherosclerosis development, in this study we enrolled only IBD patients without any well-known risk factor for atherosclerosis. Moreover, we considered only patients with a more aggressive disease receiving a biologic therapy. To assess pre-clinical atherosclerosis, we used the CIMT measurement, which is a non-invasive and highly accurate method (11). In detail, it has been shown that a 0.1 mm increment of CIMT corresponds to 10–15% and 13–18% increased risk for acute myocardial infarction and stroke, respectively (17).
Our data failed to find an increase in the CIMT values in such a homogeneous group of IBD patients without CV risk factors. Therefore, the atherosclerotic process in IBD without CV risk factors did not appear to be earlier or more accelerate than other subjects. Moreover, a recent study found that both CRP and erythrocyte sedimentation rate (ESR) did not correlate with either CMIT values or endothelial function of brachial artery in IBD patients (18). Of note, we found that CIMT mean tended to be even lower in patients than in controls (0.68 vs. 0.82 mm), particularly in those with Ulcerative Colitis (0.64 mm). Our data are in keeping with the results of a cross-sectional study performed on a database including 148,229 IBD patients where an even lower risk for heart diseases was observed. In detail, both Ulcerative Colitis (OR: 0.56; 95% CI: 0.49–0.63) and Crohn’s Disease (OR: 0.62; 95% CI: 0.56–0.68) patients resulted to be protect towards heart diseases when data were adjusted for the CV risk factors (19). The reason for which IBD patients should have a reduced risk for atherosclerosis remains unclear. A potential role for reduced visceral obesity in IBD patients has been suggested, since leptin—which is produced in the adipose tissue—exerts a pro-inflammatory action (20).
In conclusion, this case-control study found that the atherosclerotic process is not earlier in IBD patients without traditional risk factors.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: In this study, no experimental drugs or procedures were performed and patients voluntarily participated, so the ethical approval was reputed not mandatory.
References
- Pathan F, Negishi K. Prediction of cardiovascular outcomes by imaging coronary atherosclerosis. Cardiovasc Diagn Ther 2016;6:322-39. [Crossref] [PubMed]
- Spence JD. Recent advances in pathogenesis, assessment, and treatment of atherosclerosis. F1000Res 2016;5. pii: F1000 Faculty Rev-1880.
- Shoenfeld Y, Gerli R, Doria A, et al. Accelerated atherosclerosis in autoimmune rheumatic diseases. Circulation 2005;112:3337-47. [Crossref] [PubMed]
- Aggarwal A, Atreja A, Kapadia S, et al. Conventional risk factors and cardiovascular outcomes of patients with inflammatory bowel disease with confirmed coronary artery disease. Inflamm Bowel Dis 2014;20:1593-601. [Crossref] [PubMed]
- Libby P, Ridker PM, Hansson GK. Inflammation in atherosclerosis: from pathophisiology to practice. J Am Coll Cardiol 2009;54:2129-38. [Crossref] [PubMed]
- Dorn SD, Sandler RS. Inflammatory bowel disease is not a risk factor for cardiovascular disease mortality: results from a systematic review and meta-analysis. Am J Gastroenterol 2007;102:662-7. [Crossref] [PubMed]
- Singh S, Singh H, Loftus EV, et al. Risk of cerebrovascular accidents and ischemic heart disease in patients with inflammatory bowel disease: A systematic review and meta-analysis. Clin Gastroenterol Hepatol 2014;12:382-93. [Crossref] [PubMed]
- Stein JH, Korcarz CE, Hurst RT, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force Endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr 2008;21:93-111. [Crossref] [PubMed]
- O’Leary DH, Polak JF, Kronmal RA, et al. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. N Engl J Med 1999;340:14-22. [Crossref] [PubMed]
- Principi M, Mastrolonardo M, Scicchitano P, et al. Endothelial function and cardiovascular risk in active inflammatory bowel diseases. J Crohns Colitis 2013;7:e427-33. [Crossref] [PubMed]
- Crouse JR, Raichlen JS, Riley WA, et al. Effect of rosuvastatin on progression of carotid intima-media thickness in low-risk individuals with subclinical atherosclerosis: the METEOR trial. JAMA 2007;297:1344-53. [Crossref] [PubMed]
- Wu GC, Leng RX, Lu Q, et al. Subclinical atherosclerosis in patients with inflammatory bowel diseases: a systematic review and meta-analysis. Angiology 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Gandhi S, Narula N, Marshall JK, et al. Are patients with inflammatory bowel disease at increased risk of coronary artery disease? Am J Med 2012;125:956-62. [Crossref] [PubMed]
- Molenaar ET, Voskuyl AE, Familian A, et al. Complement activation in patients with rheumatoid arthritis mediated in part by C-reactive protein. Arthritis Rheum 2001;44:997-1002. [Crossref] [PubMed]
- Bruzzese V, Marrese C, Zullo A, et al. Carotid artery intima-media thickness in patients with autoimmune connective tissue diseases: a case-control study. Intern Emerg Med 2013;8:713-6. [Crossref] [PubMed]
- Bruzzese V, Hassan C, Ridola L, et al. Rheumatoid arthritis and cardiovascular risk: between lights and shadows. Curr Rheumatol Rev 2013;9:100-4. [Crossref] [PubMed]
- Lorenz MW, Markus HS, Bots ML, et al. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation 2007;115:459-67. [Crossref] [PubMed]
- Principi M, Montenegro L, Losurdo G, et al. Endothelial function and cardiovascular risk in patients with inflammatory bowel disease in remission phase. Scand J Gastroenterol 2016;51:253-5. [Crossref] [PubMed]
- Sridhar AR, Parasa S, Navaneethan U, et al. Comprehensive study of cardiovascular morbidity in hospitalized inflammatory bowel disease patients. J Crohns Colitis 2011;5:287-94. [Crossref] [PubMed]
- Fan F, Galvin A, Fang L, et al. Comparison of inflammation, arterial stiffness and traditional cardiovascular risk factors between rheumatoid arthritis and inflammatory bowel disease. J Inflamm (Lond) 2014;11:29. [Crossref] [PubMed]


