Outerbridge grade IV cartilage lesions in the hip identified at arthroscopy
Hip arthroscopy and chondral lesions
The utilization of hip arthroscopy continues to increase in both volume and scope within clinical practice (1) and can be used as a diagnostic or therapeutic intervention. Established indications for hip arthroscopy include but are not limited to diagnosis or treatment of; acetabular labral injuries, femoroacetabular impingement (FAI), chondral lesions, synovial pathologies including rheumatoid arthritis and synovial chondromatosis, removal of loose bodies, ligamentum teres tears and extra-articular pathologies such as trochanteric bursitis, gluteus medius/minimus tears and psoas tendinopathy (2). Importantly the evidence base to guide many if not all of these indications remains to be elucidated.
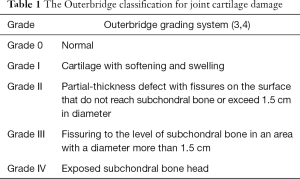
Chondral lesions/defects are typically described using the Outerbridge grading system (3) (Table 1). Grade I–II are often termed mild to moderate and grades III–IV severe (4). But equally can be described as being acute, chronic or degenerative and full or partial thickness in the literature. They are considered to originate from both traumatic and atraumatic pathologies. Pathologies associated with chondral injuries include FAI, traumatic hip dislocation/instability, lateral hip impact injury, slipped-capital femoral epiphysis, loose body formation in perthes and other chondrodysplasias, hip dysplasia and degenerative joint disease (2,5).
Full table
In particular, FAI has been shown in several studies to be associated with predictable patterns of chondral injury Ganz (6-8) described FAI as being cam, pincer or mixed type. Cam impingement is thought to be due to increased shear forces created when an abnormally shaped femoral head-neck junction is brought into contact with a normal acetabulum as the hip flexes and internally rotates. This typically causes an anterosuperior acetabular grade IV chondral delamination, often with a concomitant labral tear. Pincer impingement involves either local anterior, or generalized acetabular over-coverage of a normal femoral head. Repeated impingement between femoral head-neck junction and acetabulum result in degenerative changes including ossification of the affected labrum. This leads to an anterior acetabular chondral defect of less depth but with increased circumference and a contre-coup posterior lesion as the head is levered or subluxated against the posterior acetabular wall (5,6).
While chondral lesions will often be encountered concomitantly in the investigation of alternative pathologies presenting as a painful hip, in isolation they can be challenging to identify clinically. Common symptoms include progressive intermittent groin pain and mechanical locking, catching or clicking, with athletic activities, prolonged sitting or with hip flexion (6). Examination findings include pain on flexion, internal rotation and adduction (6). These findings are typical of FAI though and may not be specific to an isolated chondral injury, which can cause groin pain through synovial irritation alone, or be completely asymptomatic. Investigation includes standard imaging, including the AP pelvis and lateral hip X-ray. This may guide the physician to the potential of chondral injury through findings consistent with FAI or other associated hip pathologies, but it is not sensitive enough to show isolated intra-articular chondral pathology. Magnetic resonance imaging (MRI) arthrography has been shown to be relatively specific, but much less sensitive and with a low negative predictive value for identifying chondral lesions when compared to hip arthroscopy (9). Future use of gadolinium enhancement may improve this, but currently there is no adequate alternative to arthroscopy to reliably exclude chondral lesions, particularly if they are small (10).
Given the heterogeneity in the causes of chondral lesions of the hip, their variable symptomatology and unreliable non-surgical investigative identifiability, it is not surprising that their natural history has not been convincingly established in the literature (11). Current common treatments for chondral lesions of the hip include chondroplasty, microfracture and newer experimental autologous chondrocyte implantation techniques. Typically chondroplasty involves debridement of lower grade chondral lesions. Microfracture is a marrow stimulating technique applicable to focal, full thickness lesions usually between 1–4 cm in diameter (12). These techniques can be carried out either arthroscopically or as part of an open procedure and in isolation, or more commonly in addition to surgical management of separate or causative pathologies such as FAI correction, loose body removal or labral repair.
Outerbridge grade IV cartilage lesions in the hip identified at arthroscopy
In May 2016 Bhatia et al. (13) published the results of a level IV retrospective prognostic case series study with the aim of determining the pre-operative risk factors associated with grade IV cartilage defects in the hip, in patients undergoing hip arthroscopy with joint pain. They hypothesized that a larger alpha angle, increased body mass index (BMI), longer duration of symptoms, older age and decreased joint space would correlate with grade IV chondral lesions identified during hip arthroscopy. Surgery was performed between June 2006–2010 by a single surgeon at a single site specialist orthopaedic centre in Colorado, USA. Inclusion criteria included all patients undergoing primary hip arthroscopy aged older than seventeen years while exclusion criteria included prior hip surgery and incomplete data on chondral damage (size, location or grade). Of 1,693 hip arthroscopies carried out during the study period 596 were excluded; 307 had prior hip surgery, 204 were carried out in patients under eighteen years and 85 had incomplete data. This resulted in 1,097 hip arthroscopies meting study inclusion. Pre-operative demographic characteristics (age, gender & BMI), measurements from standard AP pelvic, lateral hip and false profile radiographs (alpha angle, centre edge angle and joint space) and length of symptoms characterized as greater or less than 30 months were recorded. The location and Outerbridge grade of chondral lesions when present were then recorded in each case. Multivariate analysis using a binary logistic regression model was performed using the presence or absence of a grade IV chondral defect as the dependent variable. The relative risk of these various factors was then calculated.
The study identified grade IV lesions in 28% and non-grade IV lesions in 72%. Of these non-grade IV lesions 15% had no lesion identified. The average size of grade IV lesions was 158 mm (2). Of patients with a grade IV lesions 80% had a lesion on one articular surface only, of which 76% were acetabular and 95% of these anterosuperior with chondrolabral junctional pathology. Femoral lesions were more variable in distribution. Following regression analysis, they identified that: <2 mm joint space (RR =8, P=0.0001), age >45 years (RR =2.6, P=0.0001), male sex (RR =2.6, P= 0.001), Alpha angle >55° (RR =1.9, P=0.022) and symptom duration >30 months (RR =1.4, P=0.047) were factors associated with a higher relative risk of identifying a grade IV chondral lesion during hip arthroscopy.
Where does this fit in?
One of the key strengths of this study is its large sample size and comprehensive pre and intra-operative data-collection. While the pre-operative assessment and referral of patients was made by different observers, the performance and recording of intra-operative data by an experienced single surgeon is likely to result in the reliable classification of the site and grade of chondral lesions (14). As they have acknowledged weaknesses of this study include the potential inherent bias in patient selection and the lack of MRI data for analysis.
Their findings characterizing the prevalence, anatomical distribution and relative grade of chondral lesion are broadly consistent with and supportive of the current literature. Of note, the confirmation of chondral lesions being a common phenomenon in the painful hip, around 25% being grade IV, acetabular lesions being more common than femoral and predominantly anterosuperior and the combined presence of chondrolabral dysfunction (15). Additionally their findings, support a previous study involving Philipon et al., where they found grade IV chondral lesions identifies during arthroscopy to be associated with patients with larger alpha angles on pre-operative X-rays (16).
Furthermore, rather than look at outcomes relative to either pre-operative or intra-operative findings, this study has utilized pre-operative demographics. The usefulness of their findings therefore hinges on the current understanding that patients with intra-operative evidence of grade III–IV chondral lesions have worse outcomes following hip arthroscopy (16). In that respect it supports established evidence, summarized in the systematic review by Ng et al. (17) that suggests patients with a pre-operative joint space <2 mm, age over 50 and increased alpha angle size all have worse outcomes. Where they differ in their results from the current field, as they themselves identify, is that they found BMI not to be associated with grade IV lesions.
In summary, Bhatia et al. (13) have produced a large and informative study. It will give the assessing clinician more knowledge and power to predict intra-operative findings, that would hopefully translate to improved surgical outcomes. Given there is already good evidence for most if not all of the factors they have identified being relatively reliable markers for predicting patient outcomes, the impact on the field is limited and currently will be partly academic. It may continue to grow in importance however as arthroscopic treatment options grow and outcomes improve, particularly in relation to patients with non-grade IV lesions. The field would benefit in the future, from large, high quality randomized controlled trials comparing treatment options and with lengthy follow up. This would help establish patients that would gain the most benefit out of preservative arthroscopic hip surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Montgomery SR, Ngo SS, Hobson T, et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy 2013;29:661-5. [Crossref] [PubMed]
- Shetty VD, Villar RN. Hip arthroscopy: current concepts and review of literature. Br J Sports Med 2007;41:64-8; discussion 68. [Crossref] [PubMed]
- Outerbridge RE, Dunlop JA. The problem of chondromalacia patellae. Clin Orthop Relat Res 1975.177-96. [Crossref] [PubMed]
- Femoroacetabular impingement syndrome. Available online: http://www.aaos.org/govern/federal/issues/UHCFemoroacetabularImpingementSyndrome.pdf
- Yen YM, Kocher MS. Chondral lesions of the hip: microfracture and chondroplasty. Sports Med Arthrosc 2010;18:83-9. [Crossref] [PubMed]
- Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003.112-20. [PubMed]
- Tannast M, Goricki D, Beck M, et al. Hip damage occurs at the zone of femoroacetabular impingement. Clin Orthop Relat Res 2008;466:273-80. [Crossref] [PubMed]
- McCarthy JC, Lee JA. Acetabular dysplasia: a paradigm of arthroscopic examination of chondral injuries. Clin Orthop Relat Res 2002.122-8. [Crossref] [PubMed]
- McCarthy JC, Glassner PJ. Correlation of magnetic resonance arthrography with revision hip arthroscopy. Clin Orthop Relat Res 2013;471:4006-11. [Crossref] [PubMed]
- Naraghi A, White LM. MRI of Labral and Chondral Lesions of the Hip. AJR Am J Roentgenol 2015;205:479-90. [Crossref] [PubMed]
- Kuhns BD, Weber AE, Levy DM, et al. The Natural History of Femoroacetabular Impingement. Front Surg 2015;2:58. [Crossref] [PubMed]
- Sampson TG. Arthroscopic treatment for chondral lesions of the hip. Clin Sports Med 2011;30:331-48. [Crossref] [PubMed]
- Bhatia S, Nowak DD, Briggs KK, et al. Outerbridge Grade IV Cartilage Lesions in the Hip Identified at Arthroscopy. Arthroscopy 2016;32:814-9. [Crossref] [PubMed]
- Ilizaliturri VM Jr, Byrd JW, Sampson TG, et al. A geographic zone method to describe intra-articular pathology in hip arthroscopy: cadaveric study and preliminary report. Arthroscopy 2008;24:534-9. [Crossref] [PubMed]
- McGill KC, Bush-Joseph CA, Nho SJ. Hip Microfracture: Indications, Technique, and Outcomes. Cartilage 2010;1:127-36. [Crossref] [PubMed]
- Johnston TL, Schenker ML, Briggs KK, et al. Relationship between offset angle alpha and hip chondral injury in femoroacetabular impingement. Arthroscopy 2008;24:669-75. [Crossref] [PubMed]
- Ng VY, Arora N, Best TM, et al. Efficacy of surgery for femoroacetabular impingement: a systematic review. Am J Sports Med 2010;38:2337-45. [Crossref] [PubMed]


