Posterior reversible encephalopathy syndrome associated with left horizontal gaze palsy
Case presentation
A 72-year-old female presented to the emergency department with a one-day history of recurrent falls and lethargy. She attributed her falls to tripping on things she didn’t see. Her complaints were associated with constant, severe headache that was unresponsive to analgesia. No other significant symptoms were reported. She had a past medical history of coronary artery disease, peripheral artery disease, hypertension, and dyslipidemia.
Her vital signs showed a blood pressure of 230/80 mmHg, heart rate 76/min, oxygen saturation of 99%, and temperature of 97.4. On examination, she was confused with slowed responses and oriented only to person. She had impaired remote memory and concentration. Her neurological examination was significant for left horizontal gaze palsy with intact vestibulo-ocular reflex, and right lower limb weakness with brisk right lower limb reflexes. No other focal neurological deficits were seen. The rest of her examination was unremarkable.
Blood workup including blood count, electrolytes, renal function, thyroid function, and rheumatological markers were insignificant. Brain computed tomography (CT) scan didn’t show any acute pathology. The blood pressure was slowly lowered in the emergency department, and she was admitted for further workup and evaluation.
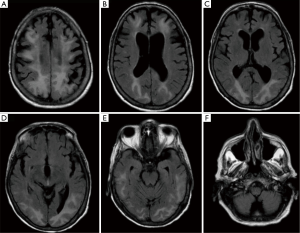
On the night of her admission, the patient developed a simple partial seizure with left upper limb tonic-clonic movements. Three doses of lorazepam, and fosphenytoin failed to control the seizures, which lasted for more than 20 minutes, and the patient required intubation. Repeat brain CT scan showed low density in the subcortical white matter in the parietal and occipital lobes (Figure 1). Subsequent magnetic resonance imaging (MRI) of the brain showed severe edema throughout the subcortical white matter, and increased signal in the posterior parietal and occipital lobes with lesser involvement of the frontal lobes and lateral temporal lobes (Figure 2).
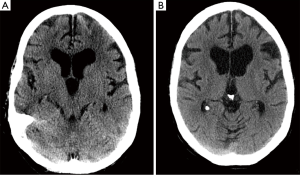
She was successfully extubated on the following day. During her hospital stay, the lateral gaze resolved and her mental status continued to improve. Follow up head CT scan showed near complete resolution of the previously described changes (Figure 1B). She was discharged after 7 days of her admission with complete resolution of her neurological symptoms without any complications.
Discussion
Posterior reversible encephalopathy syndrome (PRES) is a clinical-neuroradiological entity characterized by headache, seizures, altered consciousness, and visual disturbance as well as radiologic findings of focal reversible vasogenic edema, best seen on MRI of the brain (1-3). It is most commonly seen in association with severe hypertension, preeclampsia or eclampsia, renal disease, sepsis, collagen vascular disease and exposure to immunosuppressants (4,5).
The underlying pathophysiology of PRES remains unclear. Several theories have been proposed, the most widely accepted of which that is rapidly developing hypertension leads to disruption of cerebral autoregulation, particularly in the posterior brain. Subsequent hyperperfusion leads to protein and fluid extravasation, producing focal vasogenic edema. The dominance of posterior involvement is thought to be the result of the relative lack of sympathetic innervation in the posterior circulation in contrast to the anterior cerebral circulation (3-5).
The patient in our case presented with the clinical manifestations typically seen in PRES, including severe headache, altered consciousness, visual disturbances and seizures. Her symptoms occurred in the setting of severe hypertension with radiological findings of vasogenic edema that resolved few days after her presentation.
Blurred vision is frequently seen in patients with PRES; however, horizontal gaze palsy was not previously reported. In our case, the patient developed supranuclear horizontal gaze palsy given the intact vestibulo-ocular reflex. This palsy was mostly due to an impairment of the cortical gaze center in the frontal lobe (6-8).
The pathway for horizontal eye movement control is composed of many neurons, and passes near the internal capsule and basal ganglia to the midbrain. The pathway crosses at the junction of the midbrain and upper pons to terminate in the contralateral pontine paramedian reticular formation. In our case, the patient had left horizontal gaze palsy, which indicates that the mechanism of her gaze palsy was due to supranuclear impairment (6-8).
Early recognition and treatment of this syndrome is important to prevent permanent neurological sequelae. Symptomatic treatment should be started immediately, in addition to rapid withdrawal of the causative factors. The symptoms and radiologic features usually resolve within days to weeks.
The clinical features of PRES can resemble other neurological conditions, such as cerebral infarction, demyelinating disorder, and encephalitis. Brain MRI is very useful in differentiating between these conditions, nevertheless, in some instances such differentiation can be difficult.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this Case report and any accompanying images.
References
- Bartynski WS. Posterior reversible encephalopathy syndrome, part 1: fundamental imaging and clinical features. AJNR Am J Neuroradiol 2008;29:1036-42. [Crossref] [PubMed]
- Hinchey J, Chaves C, Appignani B, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med 1996;334:494-500. [Crossref] [PubMed]
- Fugate JE, Claassen DO, Cloft HJ, et al. Posterior reversible encephalopathy syndrome: associated clinical and radiologic findings. Mayo Clin Proc 2010;85:427-32. [Crossref] [PubMed]
- Bartynski WS. Posterior reversible encephalopathy syndrome, part 2: controversies surrounding pathophysiology of vasogenic edema. AJNR Am J Neuroradiol 2008;29:1043-9. [Crossref] [PubMed]
- Staykov D, Schwab S. Posterior reversible encephalopathy syndrome. J Intensive Care Med 2012;27:11-24. [Crossref] [PubMed]
- Cruz-Flores S, de Assis Aquino Gondim F, Leira EC. Brainstem involvement in hypertensive encephalopathy: clinical and radiological findings. Neurology 2004;62:1417-9. [Crossref] [PubMed]
- Doi Y, Kimura F, Fujiyama T, et al. Hypertensive brainstem encephalopathy without parieto-occipital lesion--two case reports. Neurol Med Chir (Tokyo) 2006;46:75-9. [Crossref] [PubMed]
- Hata M, Oishi A, Kurimoto Y, et al. A Case of Posterior Reversible Encephalopathy Syndrome Presenting with Isolated Diplopia. J Clinic Experiment Ophthalmol 2011;2:155. [Crossref]


