Benign tracheal stenosis a case report and up to date management
Introduction
The narrowing of the trachea after intubation, is an iatrogenic complication in patients undergoing mechanical ventilation and it is the most common cause of benign tracheal stenosis. The potentially fatal complication that can be avoided by implementing simple and clear preventive measures. Surgical resection of the narrowed part of the trachea with a terminal by terminal anastomosis remains the treatment of choice, although it applies only in well-selected cases and in centers with large surgical experience as it is associated with serious complications and significant failure rates (1). The endoscopic treatment performed by the attending pulmonologist displays advantages over the classical surgery and can be applied either as final treatment or as initial treatment pending definitive surgical correction or even as a palliative treatment of heavy unresectable cases. Mechanical dilatation with rigid bronchoscope, the ablation laser and placement of endotracheal stents (stents) have provided new options in the treatment of these patients. The new discipline of interventional pulmonology allowing pulmonologists to play a central role in decision making for the therapeutic treatment of such incidents (2).
Alteration of the cricoid cartilage is observed in some cases resulting in healing with tissue shrinkage and characteristic triangular (A-like) stenosis. In contrast, the balloon of the endotracheal tube causes mucosal erosion circular, circular healing leads to a circular constriction (aperture-like) (3).
There are three types of bottlenecks.
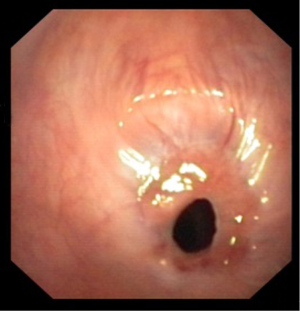
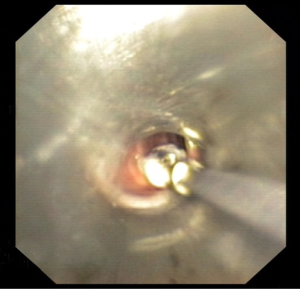
- Short constrictions (<1 cm) forming the diaphragm as a result of cyclic mucosal shrinking scar. The wall of the trachea and the cartilaginous rings are not (or very little) destroyed, and generally remain functional (Figure 1);
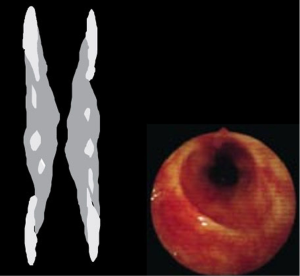
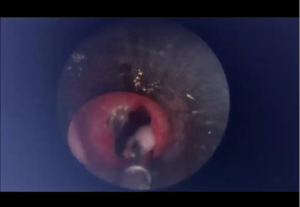
- “Complex” stenoses. These are usually longest (>1 cm) with irregular edge and often include a degree tracheomalacias which cannot be assessed until after the opening of the stenosis. These lesions are related to the entire wall of the trachea and particularly the cartilaginous rings (Figure 2);
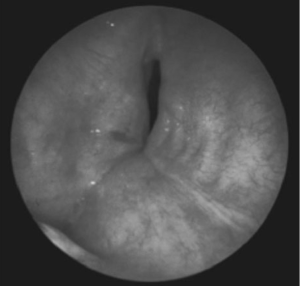
- The “pseudoglottic” strictures or stenosis due to rupture or fracture of the cartilage rings of the trachea, usually after tracheostomy and behave as a localized tracheomalacia at the scar (Figure 3).
When a stenosis of the trachea begins to give symptoms usually has already exceeded 75% of the airway diameter and the part that remains compatible is no more than 5 mm. However, the appearance of clinical signs and symptoms depends besides the degree of stenosis and the speed of air flow in the air duct. A moderate stenosis for example may be asymptomatic at rest conditions but becomes clinically when the patient cuts and increases the inspiratory flows (check by spirometry).
Thirty years after the acquisition and presentation of this knowledge, the (iatrogenic) stenosis of the trachea still, albeit less frequently, to occur and cause severe disability in patients undergoing mechanical support their breathing. The main indication or tracheal resection recovery remains today after intubation tracheal stenosis (4). The operation as it will be discussed below, is neither easy nor risk-free, and is extremely difficult when the stenosis is about more than 2 or 3 semirings.
The Tracheal tubes “low” pressure is made of limited diastolic plastic rather than latex, as originally proposed. This means that such a balloon can be easily converted to high pressure if beyond the indicated volume of air is injected. Therefore, only the truly great attention to volume “cuff” whenever inflated and deflated it would enable the mucosal injury avoidance of high pressure regime inside the inner tube. Similarly, the tube support and the tracheostomy fittings as not to exert forces and irritating to the walls, allowing to avoid erosion of the coamings and the subsequent expansion
Patient and methods
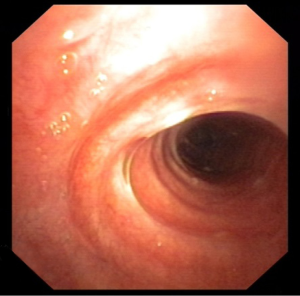
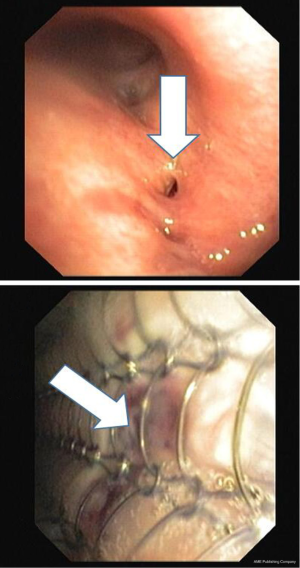
In our case we present a 65-year-old man who developed a fibrotic tracheal stenosis after urgent intubation due to arterial aneurism. The patient came with severe stridor which was developed within 6 months after extubation. The stridor was developed gradually however the patient did not pay proper attention to this symptom until he observed severe bronchoconstriction after bathing with hot water. Up admission he had FEV1 65% and bronchoscopy was performed and in Figure 1 the lesion is presented. The patient was intubated within a rigid STORZ bronchoscope 12 mm with a working channel of 11 mm and semi-rigid technique was applied with a flexible cryoprobe, rigid electrocautery, flexible electroknife and balloon dilation. The different equipment was applied according to the users choice with 15–30 seconds of application. Finally with rigid forceps mitomycin C was applied. Immediately the stridor was disappeared after extubation and spirometry after 5 days was FEV1 95%. A re-evaluation of the patient after three months as presented in Figures 4,5 as observed there was no recreation of the fibrotic tissue (Figures 4 and5).
Discussion
Treatment options
Surgery
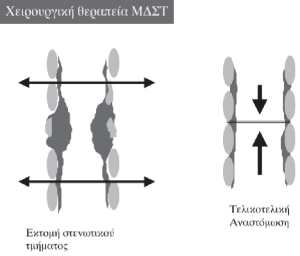
Treatment of choice and method of final treatment of tracheal stenosis remains even today surgical resection of the stenotic segment of the airway with a terminal by terminal anastomosis (sleeve resection). To perform the anastomosis we mobilize downwards the larynx or in cases of long stenosis we prepare and mobilize up the tracheobronchial bifurcation. The operation is performed in well selected patients after accurate preoperative evaluation and following prior expansions or laser sessions for the opening of the stenotic area. In cases of recurring or initially considered inoperable because of extensive lesions or presence of serious underlying disease (cardiopulmonary failure, etc.), the proposed surgical procedure is the placement of endotracheal type Montgomery T-shaped, permanent tracheostomy (5) (Figure 6).
Based on the assumption that 50% of MDST patients diagnosed with the urgency procedure and are in respiratory distress or poor general condition and therefore a contraindication (at least temporarily) for surgery, the “conservative” endoscopic treatment seems to have significant advantages.
Non-surgical techniques such as expansion to the bronchoscope or a special balloon (similar to the balloon angioplasty), by laser drilling and fitting of special prefixes (stents) have all been proposed and are already used. Even incomplete, the opening of the stenosis with the rigid bronchoscope is always immediate and spectacular results are confirmed by spirometry (6) (Figure 7).

In the remaining patients after expansion to relapse but cannot be operated because they have a contraindication, the only alternative is to bypass the bottleneck by placing a tube Montgomery T-shaped or even better a specially designed endotracheal stent (Stent) Dumon type (Figure 8).
These prefixes are made of silicone and are available in different sizes and bores. The effectiveness and very good tolerability, has extensively been confirmed. The stent is placed by the endoscopist pneumonologist through rigid bronchoscope in the area of the stenosis after dilatation of the trachea. The patient is under general anesthesia and ventilation is achieved through the bronchoscope to jet ventilation device.
An interesting observation is that the narrowed wall of the trachea that has received the prefix, often “matured” and cured with time, allowing in some cases the removal of the prefix. The withdrawal of the stent after some time (usually 12–18 months) does not present particular technical difficulties and afterwards a surgery is possible. In fact 80% of patients were considered cured and it became possible to remove the stent after 18 months, without displaying the disease relapse. Complications associated with the use of stents, which were all readily treatable were: moving (17.5%), blocked (6.3%) and developing granulomas on the lips of the prefix (6.3%). One of the main drawbacks of this type of silicone prefix is the inhibition of expectoration and normal movement of the tracheobronchial secretions may lead to acute occlusion of the prefix. However there are dynamic stent trachea in which the surface that contacts the soft segment portion of the trachea (at 6) consists of soft material which pallets with coughing and thus expectorants are more closely secretions from other silicone stent (7) (Figure 9).

The alternative of self-expandable metallic stents which allow the growth of normal mucosa and therefore mucociliary clearance above the surface of the stent must be made with extreme caution. Their removal is very difficult if not impossible and if it is a benign disease, it is generally not preferred. The occurrence of complications endotracheally is acute and requires immediate treatment. Today, in all centers applying such treatments, it is now standard supply patients with specific identity-tab. In this state the type, size and position of the stent (in case you require urgent intubation) and clinical signs and symptoms that should guide the patient and the attending physician in the respective complications.
In any case it is clear that a multifactorial structured treatment needed to ensure the cooperation of all neighboring disciplines and will be guided by the interests of patient safety (8).
Prospective techniques
Important advantages of endoscopic (non-surgical) treatment of benign strictures of the trachea and a series of other diseases of the airways, have led to internationally considerable development and application of these methods. Particularly important is the fact that they offer alternative and remarkable quality of life in inoperable cases, research directed at finding ever simpler invasive techniques capable implemented easily by pulmonologists-endoscope: Jet ventilation techniques for ensuring comfortable bronchoscopic session with the rigid, simple methods of positioning stent without the use of special devices, better and firmer stents that have fewer complications, better tools and bronchoscopes, optical fibers and videotaped enabling excellent display and recording of the whole operation (9). Alternative in the process of opening used as appropriate argon plasma system, cryotherapy, diathermy dagger flexible, rigid and diathermy balloon dilatation (Figure 10).
Finally lips touching opening gauze soaked in mitomycin C a cytostatic drug which will keep us long term results (Figure 11).
Stenosis after tracheal intubation, is an iatrogenic complication that we have to avoid the application of simple and clear preventive measures. If presented, we must promptly diagnose and treat it effectively taking under account the severity of stenosis and general condition of the patient. Endoscopic treatment displays significant advantages over classical surgical and can be applied either as final treatment or as initial treatment pending definitive surgical correction or even as a palliative treatment of heavy unresectable cases (10). The new discipline of interventional pulmonology allowing pulmonologists to play a central role in decision making for dealing with such incidents. Endoprosthesis (stent) and malignancy can be used to maintain the patency of the airway, or even to close a communication between the trachea and esophagus or between trachea and mediastinum (Figure 12).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Sehgal IS, Dhooria S, Bal A, et al. Obstructive Fibrinous Tracheal Pseudomembrane After Endotracheal Intubation. Respir Care 2016;61:1260-6. [Crossref] [PubMed]
- Elsayed H, Mostafa AM, Soliman S, et al. First-line tracheal resection and primary anastomosis for postintubation tracheal stenosis. Ann R Coll Surg Engl 2016;98:425-30. [Crossref] [PubMed]
- Hu T, Zhu X, Lei W. Complications associated with silicone T-tube placement in the treatment of cicatricial subglottic and tracheal stenosis. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2015;29:2166-9. [PubMed]
- Kirschbaum A, Teymoortash A, Suárez C, et al. Treatment of large tracheal defects after resection: Laryngotracheal release and tracheal replacement. Auris Nasus Larynx 2016;43:602-8. [Crossref] [PubMed]
- Auchincloss HG, Wright CD. Complications after tracheal resection and reconstruction: prevention and treatment. J Thorac Dis 2016;8:S160-7. [PubMed]
- D'Andrilli A, Venuta F, Rendina EA. Subglottic tracheal stenosis. J Thorac Dis 2016;8:S140-7. [PubMed]
- Dalar L, Karasulu L, Abul Y, et al. Bronchoscopic Treatment in the Management of Benign Tracheal Stenosis: Choices for Simple and Complex Tracheal Stenosis. Ann Thorac Surg 2016;101:1310-7. [Crossref] [PubMed]
- Huuskonen A, Mäkitie A, Sihvo E. Treatment of adult tracheal stenosis. Duodecim 2015;131:1793-801. [PubMed]
- Hohenforst-Schmidt W, Linsmeier B, Zarogoulidis P, et al. Transtracheal single-point stent fixation in posttracheotomy tracheomalacia under cone-beam computer tomography guidance by transmural suturing with the Berci needle - a perspective on a new tool to avoid stent migration of Dumon stents. Ther Clin Risk Manag 2015;11:837-50. [PubMed]
- Liu J, Zhang CP, Li Y, et al. Post-intubation tracheal stenosis after management of complicated aortic dissection: a case series. J Cardiothorac Surg 2015;10:148. [Crossref] [PubMed]