Obstruction of the right stem bronchus due to ovarian local metastasis: a 5-year follow-up
Introduction
Metastatic involvement to female genital tract by lung cancer is rare. Ovarian and vaginal involvement are the most common gynecological metastatic sites for both extra-genital and genital primary malignancies (1). The ovaries are relatively common sites of metastasis from primary lung adenocarcinoma (2). Metastatic ovarian tumors account for approximately 10–30% of all ovarian cancers (3,4). The common primary sites are colon, stomach, appendix, breast and pancreas (3). Ovarian metastasis from lung cancer is extremely rare, it accounts for only 0.3–0.4% of metastatic ovarian tumors (5). Surgical approach remains the best method for permanent results, however; there are cases where stent applications by endoscopic methods are more efficient in the treatment of benign or malignant central airway lesions (6-8). It is known that Dumon was the first to place silicon stents in the respiratory system. There are two major types of stents the silicon and the metallic stents. These endoprostheses can be applied benign and malignant airway conditions (9). The safest method of deploying a stent is through a rigid bronchoscope, although this is not always necessary as for example in the case of a dynamic stent. The method of application depends on the position of deployment and type of stent. Semi-rigid technique with the flexible bronchoscope being inserted through the rigid bronchoscope is considered a very safe approach with the addition of jet-ventilation model. Self-expanding metallic stents can also be placed under fluoroscopic or guidewire guidance (10,11). Moreover; the treating physician will choose the method of application based on the general clinical condition of the patient, the experience of the team and the capacity of the treating unit. Currently there are guidelines for the use of either guidewires alone or guidewires with the combination of fluoroscopy (12,13). There is also a study where rigid bronchoscopy, as used without the need for either fluoroscopy or guidewires (14). Metallic stent placement has been applied with the use of fiber-optic bronchoscopy under fluoroscopic or guidewire guidance, using only local anesthesia, in patients to whom surgery and rigid bronchoscopy were contra-indicated. However; extreme caution has to be taken. The treating physician has to plan all backup plans in case of an emergency. It is considered that stent deployment under fiber-optic bronchoscopy and guidance of fluoroscopy and guidewire guidance is costly (13). However; not all interventional pulmonology units have all the necessary equipment, therefore it is better for the patient if a center does not have all the necessary equipment to cope the possible adverse effects not to insert stents. The most important tools are electrocautery, argon plasma coagulation (APC), YAG laser equipment, and cryotherapy that are usually needed for interventional pulmonology. It has been observed that SEMS placement via bronchoscopy under general anesthesia affords many advantages. It is known that bronchoscopy under general anesthesia prevents coughing or patient movement, and therefore blood clots or secretions can be quickly removed. Also, it is safer for the patients in case of an emergency such as bleeding to be handled. The stenotic airway segment can be maintained open by mechanical dilatation and desobstruction stent placement (15-17).
Case presentation
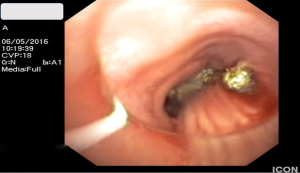
We report the case of a 55 years old women who had been surgically treated for ovarian cancer at the age of 50. Seven months after successful surgery she gradually developed intense cough and dyspnea. An X-ray was performed and afterwards based on the findings CT scan of the thorax and bronchoscopy (Figure 1). She had lesions inside the trachea and right stem bronchus. Biopsies showed that the lesions were metastasis from her previous ovarian cancer. Loop electrocautery probe and APC probe were used after rigid bronchoscope insertion (STORZ 12 mm with working channel 11 mm) through the working channel of an Olympus® fiberoptic bronchoscope. The woman had in total two lines of chemotherapy sessions of six cycles each and five sessions of interventional bronchoscopy for debulking at different time intervals and finally stent placement (Figures 2-4). Finally after recurrent disease progression within the airways it was decided that a self-extendable covered Y stent was placed on the carina. During the follow-up no coin lesions were observed within the lung parenchyma and chemotherapy was administered only for the intrabronchial lesions. Also, upon follow-up no distant metastasis was observed. After 5 days of stent placement the patient developed severe dyspnea with severe desaturation. Bronchoscopic evaluation showed that the right stem bronchus was full of secretions and was cleared with saline. The major problem for this patient was that the right stem bronchus was filled with malignant tissue at the last time of follow up because the patient was not observed regularly as supposed based on her will. Therefore before stent placement the debulking (laser, APC and mechanical debulking with forceps) was very difficult and took almost 2 hours with the patient under jet-ventilation and regular stops. It was observed with CT scan of the thorax that a tissue was starting to form around the right stem bronchus which assisted in pressing the stent. The patient is under follow-up.
Discussion
In our case we used a rigid bronchoscope and fiber-optic bronchoscope to place a Y SEMS in the carina. Initially we performed debulking (APC), electrocautery and mechanical debulking with forceps mainly in the right stem bronchus and using fluoroscopy and guidewires placed the Y covered SEMS. No severe complication occurred upon placement. It is known that bifurcated stents are preferred in the case of carinal stenosis, or in the case of a tracheoesophageal fistula. There is also the case where a fistula might develop at the anastomotic site after operation. Moreover; rigid bronchoscopy is more efficient in such situations (18-20). It is very important that these procedures take place in centers with experience in order to avoid laceration of the airways, tracheobronchial wall and main vessels damage (21). SEMS are either silicon-covered, made of nickel titanium alloy or without cover.
Previously in a study by Herth et al. the authors placed plain metallic stents in 96 patients using fiberoptic bronchoscopy with guidewire guidance, where fluoroscopy was not employed. In this study no procedure-related complication was noted (13). In a study by Lin et al. the authors used fiberoptic bronchoscopy with guidewire guidance to treat airway lesions, where fluoroscopy was not used. In this study plain metallic stents were placed in 26 patients who then underwent endotracheal tube intubation because of acute respiratory insufficiency. Only fourteen of these patients were weaned from mechanical ventilation afterwards (22). In the study by Husain et al. the authors placed ultraflex airway stents in 66 patients with malignant and benign airway obstructions. The complications observed were only in four patients and were not stent-related. Until now various endoscopic methods have been used and can be used, alone or in combination for different airway lesions. Depending on the underlying disease, the type of stenosis, and the clinical condition of the patient different methods can be used in centers with experience in this field (23,24). Therefore several parameters have to be considered for a patient. It has been observed that for safety reasons for whom endoscopy is planned if general anaesthesia can be tolerated then rigid rather than simple fiberoptic bronchoscopy has to be used (25). Using rigid bronchoscopy the hemorrhage and ventilatory deficiency can be effectively managed (jet-ventilation model), along with blood secretions aspiration. For safety reasons we use general anaesthesia in the daily practice in our unit. However; we have to say that general anaesthesia again increases procedure time and is associated with anaesthesia-related complications (e.g., investigate patients for chronic obstructive disease and proper treatment administration) (22). Moreover; additional systematic chemotherapy administration is necessary if the patient is fit, since it acts additionally to the local treatment effect and prolongs the positive result. There is no meaning to act only locally, except in the case where the patient has low performance status. Also, radiotherapy could be considered on a case by case choice. Multimodality treatment approach is necessary for such extreme cases where there are very few cases published. Soon local microwave therapy application will be available for such cases (26).
Conclusions
Our major concern was whether we should insert a silicon stent or a SEM, based on the medical history of the patient, since the disease was only inside the bronchial lumen and not inside lung parenchyma. We chose SEM in order to support the Y structure of the trachea since we felt that the force of the lesions that would be created through time would severely affect the architecture of this airway region.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Mazur MT, Hsueh S, Gersell DJ. Metastases to the female genital tract. Analysis of 325 cases. Cancer 1984;53:1978-84. [Crossref] [PubMed]
- Irving JA, Young RH. Lung carcinoma metastatic to the ovary: a clinicopathologic study of 32 cases emphasizing their morphologic spectrum and problems in differential diagnosis. Am J Surg Pathol 2005;29:997-1006. [PubMed]
- Alvarado-Cabrero I, Rodríguez-Gómez A, Castelan-Pedraza J, et al. Metastatic ovarian tumors: a clinicopathologic study of 150 cases. Anal Quant Cytopathol Histpathol 2013;35:241-8. [PubMed]
- Jung YE, Lee JW, Kim BG, et al. Ovarian metastasis from pulmonary adenocarcinoma. Obstet Gynecol Sci 2013;56:341-4. [Crossref] [PubMed]
- Fujiwara K, Ohishi Y, Koike H, et al. Clinical implications of metastases to the ovary. Gynecol Oncol 1995;59:124-8. [Crossref] [PubMed]
- Bolliger CT, Mathur PN, Beamis JF, et al. ERS/ATS statement on interventional pulmonology. European Respiratory Society/American Thoracic Society. Eur Respir J 2002;19:356-73. [PubMed]
- Seijo LM, Sterman DH. Interventional pulmonology. N Engl J Med 2001;344:740-9. [Crossref] [PubMed]
- Casal RF. Update in airway stents. Curr Opin Pulm Med 2010;16:321-8. [Crossref] [PubMed]
- Dumon JF. A dedicated tracheobronchial stent. Chest 1990;97:328-32. [Crossref] [PubMed]
- Hautmann H, Bauer M, Pfeifer KJ, et al. Flexible bronchoscopy: a safe method for metal stent implantation in bronchial disease. Ann Thorac Surg 2000;69:398-401. [Crossref] [PubMed]
- Saad CP, Murthy S, Krizmanich G, et al. Self-expandable metallic airway stents and flexible bronchoscopy: long-term outcomes analysis. Chest 2003;124:1993-9. [Crossref] [PubMed]
- Dasgupta A, Dolmatch BL, Abi-Saleh WJ, et al. Self-expandable metallic airway stent insertion employing flexible bronchoscopy: preliminary results. Chest 1998;114:106-9. [Crossref] [PubMed]
- Herth F, Becker HD, LoCicero J 3rd, et al. Successful bronchoscopic placement of tracheobronchial stents without fluoroscopy. Chest 2001;119:1910-2. [Crossref] [PubMed]
- Husain SA, Finch D, Ahmed M, et al. Long-term follow-up of ultraflex metallic stents in benign and malignant central airway obstruction. Ann Thorac Surg 2007;83:1251-6. [Crossref] [PubMed]
- Bacon JL, Patterson CM, Madden BP. Indications and interventional options for non-resectable tracheal stenosis. J Thorac Dis 2014;6:258-70. [PubMed]
- Crerar-Gilbert A, Madden BP. The use of rigid bronchoscopy for bronchial stenting in patients with tracheal stenosis. J Cardiothorac Vasc Anesth 2007;21:320. [Crossref] [PubMed]
- Guibert N, Mazieres J, Marquette CH, et al. Integration of interventional bronchoscopy in the management of lung cancer. Eur Respir Rev 2015;24:378-91. [Crossref] [PubMed]
- Saji H, Furukawa K, Tsutsui H, et al. Outcomes of airway stenting for advanced lung cancer with central airway obstruction. Interact Cardiovasc Thorac Surg 2010;11:425-8. [Crossref] [PubMed]
- Ernst A, Majid A, Feller-Kopman D, et al. Airway stabilization with silicone stents for treating adult tracheobronchomalacia: a prospective observational study. Chest 2007;132:609-16. [Crossref] [PubMed]
- Yata S, Kaminou T, Hashimoto M, et al. Successful closure of intractable tracheoesophageal fistula using a combination of a modified silicon stent and metallic stents. Acta Radiol Short Rep 2012;1. pii: arsr.2012.110005.
- Conacher ID. Anaesthesia and tracheobronchial stenting for central airway obstruction in adults. Br J Anaesth 2003;90:367-74. [Crossref] [PubMed]
- Lin SM, Lin TY, Chou CL, et al. Metallic stent and flexible bronchoscopy without fluoroscopy for acute respiratory failure. Eur Respir J 2008;31:1019-23. [Crossref] [PubMed]
- Hsia D, Musani AI. Interventional pulmonology. Med Clin North Am 2011;95:1095-114. [Crossref] [PubMed]
- Akulian J, Feller-Kopman D, Lee H, et al. Advances in interventional pulmonology. Expert Rev Respir Med 2014;8:191-208. [Crossref] [PubMed]
- Alraiyes AH, Machuzak MS. Rigid bronchoscopy. Semin Respir Crit Care Med 2014;35:671-80. [Crossref] [PubMed]
- Chhajed PN, Tamm M. Will There Be a Role for Bronchoscopic Radiofrequency Ablation? J Bronchology Interv Pulmonol 2005;12:184.





