Hotspotting sepsis: applying analytic tools from other disciplines to eliminate disparities
A recent manuscript by Moore and colleagues (1) identified geographic disparities in sepsis mortality. Using death certificates obtained from the National Center for Health Statistics, they performed a descriptive analysis of sepsis-related death over a 10-year period [2003–2012]. The investigators used three different approaches to identify mortality clusters (groups of sepsis death) in each of the 3,109 counties in the contiguous United States. They categorized sepsis deaths in each county as strongly clustered, moderately clustered, or nonclustered, based on clustering method agreement (agreement between three methods, two methods, and less than two methods, respectively). After adjusting for patient age and county-level characteristics (e.g., education, income, percentage of medically uninsured) the cluster groups had the following average mortality rates: 85.7 per 100,000 for strongly-clustered, 74.8 per 100,000 for moderately-clustered, and 56.8 per 100,000 for nonclustered counties. The investigators found that 92% of strongly- and moderately-clustered counties were located in the south. Sepsis-related mortality was highest in three regions, all within the Southeastern United States: “Mississippi Valley”, “Middle Georgia”, and “Central Appalachia”. Strongly clustered sepsis counties were more likely to have a higher percentage of residents who are unemployed, uninsured, and with less education and lower income.
Geographic relatedness is a core component of epidemiologic research and outbreak investigation. An early application of cluster analysis dates to 1854, when British anesthesiologist John Snow showed that cholera deaths were spatially related to the Broad Street water pump in London (2). Interest in geolocation continues today, with recent work in the United States showing highest age-adjusted sepsis mortality in 11 adjacent southeast and mid-Atlantic states (3), and the greatest seasonal swings in sepsis in the Northeast (4). Moore and colleagues extend this work by identifying county-level clusters of sepsis deaths. By using a smaller geographic unit (i.e., the county), the authors present a more nuanced description of outcome variation. The county-level approach allowed them to identify communities with very high mortality rates that might otherwise have been missed if data were averaged across the entire state. Likewise, the authors were able to identify community characteristics that were significantly associated with the clusters—characteristics that may have been obscured in a higher level aggregation.
Moore and colleagues’ analysis combined three spatial clustering methodologies: empirical Bayes, local indicators of spatial autocorrelation (LISA), and Getis-Ord (Gi*) statistic. Empirical Bayes methods use statistical inference, where each county rate estimate is combined with information from the entire cohort. The approach employs a smoothing function, guarding against rate instability caused by small changes in case numbers in counties with low censuses. LISA identifies counties with similar mortality values to their surrounding counties. LISA will therefore identify dense regions of multiple counties with high mortality. Clusters of adjacent counties were variably defined: “high-high cluster”, “high-low outlier”, “low-high outlier”, and “low-low cluster”. Instead of identifying the similarities between values, Gi* determines how local patterns compared to the global pattern, identifying “hot-spots” and “cold-spots” of sepsis-related mortality. Using these three approaches the investigators were able obtain a stable analysis of sepsis-related death, compare sepsis mortality rates at the local level, and put local patterns in the context of national patterns.
The methods and overall approach are both novel, yet this paper is only one step towards characterizing the actionable factors contributing to disparities in sepsis. The authors’ results are consistent with prior observations linking disparities in sepsis outcomes to patient conditions, genetics, income and healthcare access (5-8). Moore and colleagues found that the majority of counties with strong clusters of sepsis mortality occur in the southeastern US, a part of the country with higher concentrations of these inequities. In prior work, the authors labeled this region the “sepsis belt”, based on similar patterns described at the state level (3). Indeed, sepsis is not the only disease process that has a disproportionate impact on the southeastern US. Similar patterns are seen in other life-threatening conditions such as stroke and heart failure (9,10).
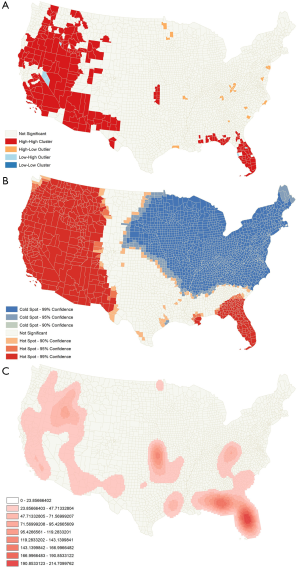
Other disciplines use geospatial mapping and cluster analysis in both cutting-edge research and everyday practice, with tangible impact. The Forest Service and the Department of Interior uses geospatial analysis to note patterns in large fires across the United States. Figure 1 demonstrates national patterns in forest fires over approximately a 30-year period using three different analytics. The top panel uses Anselin Local Moran’s I, which identifies high and low-risk counties based on a set of weighted features, and relates them spatially to values of surrounding counties which creates clusters. The middle panel uses Gi* to identify county hotspots where forest fires are more common. The bottom panel shows a kernel density analysis of point locations. This kind of data is used to make real-time tactical decisions about resident evacuations and prospective resource allocation decisions before the fire season even starts (11).
CrimeStat is a geographic information system (GIS) software tool that analyzes time and location patterns for crimes in many municipalities (12). CrimeStat identifies crime hotspots using a variety of tools. One such tool is k-means clustering, a machine learning algorithm used to partition data by plotting k “focal points” and building data clusters around them (13). New crime events are added to the map through an iterative process, assigning each new data point to the closest focal point and reweighting the cluster means to determine a new geometric center of the cluster. Police departments routinely deploy additional prevention resources in hotspots, or alternatively, use the information to guide investigations when the data suggests a pattern. They can also map changes in the distribution of crime over time using CrimeStat’s space-time analysis routine. The use of such mapping has been shown to decrease drug-related and violent crime in at least one major American city (14).
With real-time geographic analyses routinely applied to forestry, crime and other disciplines, why not healthcare? The time has come to use cluster analyses and other geospatial tools to identify and eliminate disparities in health care quality. All existing GIS studies in sepsis (including that of Moore and colleagues) were done in the era prior to the Affordable Care Act (ACA). The effect of the ACA on the disparities of sepsis mortality has yet to be seen, but recent research shows that the rates of uninsured patients has declined since the ACA became law in 2010 (15). We anticipate that these gains will translate into a cooling of Moore’s sepsis belt hotspots; however, this is an untested hypothesis. Future work should incorporate information on outcomes and exposures derived from clusters to strengthen the causal inference between insurance status and healthcare quality.
Once observational studies identify other modifiable risk factors, randomized controlled trials are needed to test if addressing those factors will improve sepsis mortality. Such studies can test whether strategic interventions in hotspot areas can improve sepsis outcomes, similar to the CrimeStat approach of focused resource allocation.
As research defines risk factors for sepsis disparities and the most effective strategies to eliminate them, GIS systems should also be used to implement those strategies in everyday healthcare practice. The ACA calls for healthcare providers and hospitals to form Accountable Care Organizations (ACOs), to make healthcare more efficient for patients and more affordable for the healthcare system. As ACOs are incentivized for healthcare quality and cost savings (16), they should use GIS to both monitor and improve healthcare delivery. When sepsis hotspots are identified, ACOs or insurance companies could plan insurance enrollment campaigns at community events. ACOs can also use information from hotspots to determine if modifiable factors other than insurance contribute to poor outcomes in a particular hotspot (e.g., an outbreak of catheter-associated urinary tract infections from urinary catheters among nursing home residents) and implement targeted interventions (e.g., institute a nursing home quality improvement checklist to remove unnecessary catheters). In the inpatient setting, hospitals with the highest sepsis incidence and mortality may benefit from ACO collaboration to ensure that sepsis quality benchmarks are being met, and to intensify quality improvement efforts at the bedside if they are not. Thus, geospatial analytic tools can have an impact on day-to-day sepsis care in multiple settings.
Moore and colleagues refined the way we look at an old problem. Sepsis-related death varies dramatically by geographic location, and this can be tied to differences in known risk factors. They introduce cutting-edge approaches from other disciplines to isolate regions with known risk factors for sepsis-related death. This is a good first-step, but we must move from describing the problem of sepsis-related disparities and begin addressing the factors and patterns in real-time so that disparities in sepsis are eliminated. We welcome future studies and applications of novel analytic tools that get us closer to this goal.
Acknowledgements
Dr. Wallace is currently funded to use geographic information system analytics through a K08 award provided by the National Heart, Lung, and Blood Institute of the National Institutes of Health (NIH).
Footnote
Provenance: This is a Guest Commentary commissioned by Section Editor Zhi Mao, MD (Department of Critical Care Medicine, Chinese People’s Liberation Army General Hospital, Beijing, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
Disclaimer: The article’s contents are solely the responsibility of the authors and do not necessary represent the official view of the NCRR or NIH.
References
- Moore JX, Donnelly JP, Griffin R, et al. Defining Sepsis Mortality Clusters in the United States. Crit Care Med 2016;44:1380-7. [Crossref] [PubMed]
- Lilienfeld DE. Commentary: John Snow's 'On the supposed influence of offensive trades on mortality': the 'Snow paradigm'. Int J Epidemiol 2013;42:1240-1. [Crossref] [PubMed]
- Wang HE, Devereaux RS, Yealy DM, et al. National variation in United States sepsis mortality: a descriptive study. Int J Health Geogr 2010;9:9. [Crossref] [PubMed]
- Danai PA, Sinha S, Moss M, et al. Seasonal variation in the epidemiology of sepsis. Crit Care Med 2007;35:410-5. [Crossref] [PubMed]
- Esper AM, Moss M, Lewis CA, et al. The role of infection and comorbidity: Factors that influence disparities in sepsis. Crit Care Med 2006;34:2576-82. [Crossref] [PubMed]
- Soto GJ, Martin GS, Gong MN. Healthcare disparities in critical illness. Crit Care Med 2013;41:2784-93. [Crossref] [PubMed]
- Lyon SM, Benson NM, Cooke CR, et al. The effect of insurance status on mortality and procedural use in critically ill patients. Am J Respir Crit Care Med 2011;184:809-15. [Crossref] [PubMed]
- Mendu ML, Zager S, Gibbons FK, et al. Relationship between neighborhood poverty rate and bloodstream infections in the critically ill. Crit Care Med 2012;40:1427-36. [Crossref] [PubMed]
- Casper ML, Wing S, Anda RF, et al. The shifting stroke belt. Changes in the geographic pattern of stroke mortality in the United States, 1962 to 1988. Stroke 1995;26:755-60. [Crossref] [PubMed]
- Mujib M, Desai R, Levitan EB, et al. Prospective population studies of incident heart failure without data on baseline left ventricular ejection fraction. Arch Med Sci 2010;6:686-8. [Crossref] [PubMed]
- National Park Service, U.S. Department of the Interior. Using MTBS data to assist with land management decisions Grand Canyon National Park. Available online: http://www.mtbs.gov/files/posters/GrandCanyon_DecisionSupport.pdf
- Levine N. Crime mapping and the CrimeStat program. Geographical Analysis 2006;38:41-56. [Crossref]
- U.S. Department of Justice, Office of Justice Programs, National Institute of Justice. Mapping crime: understanding hotspots. Available online: https://www.ncjrs.gov/pdffiles1/nij/209393.pdf
- Lawton BA, Taylor RB, Luongo AJ. Police officers on drug corners in Philadelphia, drug crime, and violent crime: Intended, diffusion, and displacement impacts. Justice Quarterly 2005;22:427-51. [Crossref]
- French MT, Homer J, Gumus G, et al. Key Provisions of the Patient Protection and Affordable Care Act (ACA): A Systematic Review and Presentation of Early Research Findings. Health Serv Res 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Fisher ES, Staiger DO, Bynum JP, et al. Creating accountable care organizations: the extended hospital medical staff. Health Aff (Millwood) 2007;26:w44-57. [Crossref] [PubMed]


