Does patellofemoral congruence following total knee arthroplasty correlate with pain or function? Intraoperative arthroscopic assessment of 30 cases
Introduction
Total knee arthroplasty (TKA) is a successful procedure, with more than 560,000 operations performed annually in Europe (1) and over 600,000 in the United States (2). Despite its success, many patients remain dissatisfied after TKA, where patellofemoral pain and instability remain among the most common reasons for reoperation or revision (3-7).
Anterior knee pain (AKP) is observed in TKA both with and without patellar resurfacing (5,6,8,9). Neither patellar denervation (4,10) nor secondary resurfacing (11,12) proved effective for treating the symptoms. Although the exact causes for pain remain unclear, abnormal patellofemoral joint loads or kinematics due to patellar malalignment (7,13,14), or inadequate implant design (15,16) seem to play an important role.
Numerous authors observed that TKA increases patellofemoral pressures, particularly in mid- and late flexion (16-19). Recent in vitro studies demonstrated that retro-patellar pressures are influenced by trochlear geometry, as well as the morphology of the native patella, or the shape of the patellar button (16-18,20). Furthermore, when the patella is not resurfaced, the extent of patellar cartilage erosion could affect the incidence of pain and revision (21).
Various studies investigated the influence of patellar morphology, using the Wiberg classification, on patellofemoral pressure (18,20,22), congruence (23,24) or instability (23,25). While patellar morphology is often associated with excessive tilt, Wiberg type C being most predisposed (23,24), it does not necessarily correlate with patellar subluxation or osteosclerosis (22,25), and pressure distribution data cannot be extrapolated to conclude on AKP or clinical outcomes. Moreover, most studies of patellar congruence are either radiographic, and therefore represent limited static data with inconsistent reliability (26), or intra-operative with the joint capsule open and therefore under non-physiological conditions (27).
The purpose of the present study was to arthroscopically evaluate patellofemoral congruence after wound closure following TKA without patellar resurfacing, and to correlate congruence to patellar morphology and postoperative pain and function. The hypothesis was that Wiberg type C patellae or poor patellofemoral congruence would be associated with greater incidence of AKP and inferior functional outcomes.
Methods
Study design
The authors prospectively enrolled 30 patients that received uncemented postero-stabilized TKA by the senior author (Olivier Courage) between November 2014 and March 2015. All patients provided written consent for their participation in this study, which was approved by the institutional review board (CPP-SC #2015/009).
All knees were preoperatively evaluated using weight-bearing X-rays of the lower limb. The patellofemoral joint was assessed on ‘skyline views’ with the knees flexed at 45°, as described by Merchant (28), and the morphology of the patella was defined using the Wiberg classification (29):
- Type A: the medial facet is concave and has almost the same area of the lateral facet;
- Type B: the medial facet is still concave, but is smaller than the lateral face;
- Type C: the medial facet is convex and is almost vertical.
The inclusion criteria were stage III or IV tibiofemoral osteoarthritis, varus deformity with HKA <5°, and Caton-Deschamps index of patellar height between 0.8 and 1.2. The exclusion criteria were concomitant or isolated patellofemoral arthritis, previous surgery on the ipsilateral knee, valgus deformity, and history of patellar pain or instability.
Surgical technique
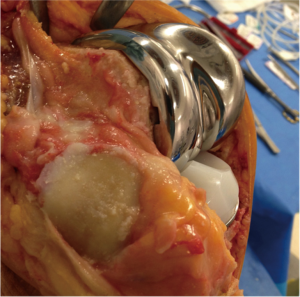
All operations were performed under general anaesthesia using a tourniquet though a standard midvastus approach. The implant used was the uncemented postero-stabilised HLS KneeTec® (Tornier SA, Montbonnot, France) with a mobile tibial insert. The implant design and operative techniques were consistent throughout the inclusion period. The patella was everted for the procedure and was left unresurfaced in all cases (Figure 1). The measured bone resection technique was followed to obtain equal flexion and extension gaps and to facilitate soft-tissue balancing. The medial third of the tibial tubercle was used as the anterior reference for alignment of the tibial base plate. The distal femoral resections were perpendicular to the femoral mechanical axis and the femoral component rotations were all aligned to Whiteside’s line.
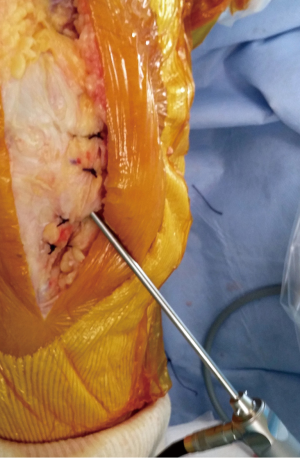
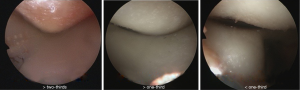
Patellofemoral congruence was assessed arthroscopically after wound closure by estimating the contact area between the native patellar cartilage and the prosthetic trochlea. The arthroscope was introduced, taking care not to damage the implanted components (Figure 2), and the tourniquet was removed. A lateral infrapatellar portal was used to secure the visual field in the joint which was visualized without fluid flow. The lower limb hang free and the knee was flexed up to 60° to visualize the entire patellofemoral contact surface. The congruence was classified either as (I) more than two-thirds of the surface; (II) more than one-third of the surface; or (III) less than one-third of the surface (Figure 3).
Postoperative evaluation
All patients were evaluated clinically 12 to 18 months following their index operation using the Knee Society Score (KSS), the Visual Analogic Scale (VAS) for AKP, in addition to subjective satisfaction on a four-point scale. The case notes for all patients were reviewed and intraoperative or postoperative complications were recorded.
Statistical analysis
Statistical analyses were performed using R version 3.1.3 (R Foundation for Statistical Computing, Vienna, Austria). Descriptive statistics were used to summarize the data. As data were not normally distributed, the statistical analyses were non-parametric. The postoperative outcomes were correlated with preoperative assessments of patellar morphology and to intraoperative patellofemoral congruence. Between group differences (patellar morphology, patellofemoral congruence) were tested using Wilcoxon rank sum tests (Mann Whitney U test), and within group differences (patellar morphology and congruence vs. clinical outcomes) using Wilcoxon signed rank tests. Categorical data were analyzed using Pearson chi-square tests or Fisher’s exact tests. P values <0.05 were considered statistically significant.
Results
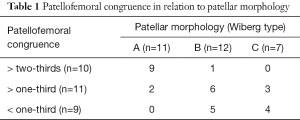
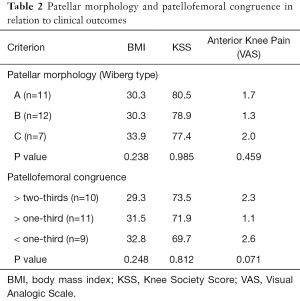
All 30 patients completed clinical assessment at mean follow-up of 14.0±1.8 months (median, 14; range, 12–18). They included 8 men and 22 women with mean age of 68.8±7.4 years (median, 67.5; range, 57–84). Their mean body mass index (BMI) was 31.2±6.1 (median, 31.3; range, 23.0–43.0). The preoperative patellar morphology was classified as Wiberg type A in 11 knees, B in 12 knees and C in 7 knees. The patellofemoral congruence assessed intraoperatively was > two-thirds of the surface in 10 knees, > one-third of the surface in 11 knees, and < one-third of the surface in 9 knees.
The mean KSS was 79.1±7.4 (median, 85; range, 50.0–94) and the VAS for AKP was 1.6±1.3 (median, 1; range, 0–5). Patient satisfaction was excellent in 13, good in 12, fair in 4 and poor in 1. The only complication recorded was knee stiffness at 2 postoperative months, in a woman aged 61 years, treated successfully by mobilization under anaesthesia. There were no subluxations, dislocations, nor instabilities of the patella throughout the follow-up period.
Multivariable analysis revealed a strong association between patellar morphology and patellofemoral congruence (P<0.001). Patellofemoral congruence was > two-thirds for most patellae of Wiberg type A, and it was < one-third only in patellae of Wiberg types B and C (Table 1).
Full table
There were no statistical correlations between clinical outcomes (KSS, VAS or satisfaction) and either patellar morphology, patellofemoral congruence, or any patient characteristics (age, gender or BMI). There were also no statistical correlations between patellar morphology or patellofemoral congruence and patient characteristics (Table 2).
Full table
Discussion
The most important finding of this study was that despite a strong association between preoperative patellar morphology and intraoperative patellofemoral congruence, neither of those two variables were correlated with any clinical outcomes nor with patient demographics. The original hypothesis, that Wiberg type C patellae or poor patellofemoral congruence would influence pain or functional outcomes, is therefore refuted. Considering that numerous incongruent patellofemoral joints were pain-free, and conversely, many perfectly congruent patellofemoral joints had anterior pain, the authors suppose that pain is probably caused by mechanisms other than patellofemoral pressures.
The present study is the first to investigate the relationship between patellofemoral morphology and AKP or functional outcomes following TKA. It is important to note that the implant used was postero-stabilised with a mobile-bearing tibial insert, which may not render identical results as cruciate-retaining models with fixed-bearing tibial inserts, although overall outcomes using both models are comparable (30,31). While several authors quantified changes in retropatellar pressures in vitro (16-19), to the authors’ knowledge, there are no published studies that demonstrated whether such forces and pressures have any relation to pain or function. Patellar morphology is known to influence patellofemoral pressure (18,20,22), congruence (23,24) or instability (23,25), and while it is often associated with tilt (23,24), it does not necessarily correlate with poor outcomes (22,25).
The authors are aware of only one study (21), that correlated pain and revision rates following TKA with preoperative characteristics of the patella, which proved that patellar cartilage erosion influences outcomes. The study did not take patellar morphology, congruence or pressures into consideration, but clearly concludes that what matters is the state of patellar cartilage that can influence outcomes. Our present study conversely did not account for the extent of cartilage erosion, which could be the principal factor influencing pain and function, rather than morphology or congruence. It could be that a dysplastic patella or an incongruent patellofemoral joint can function adequately and pain-free if the articular cartilage is sufficiently thick and healthy.
Whereas our findings cannot be directly translated into recommendations for clinical practice, as neither patellar morphology nor congruence were related to the measured outcomes, analysis of the literature suggests that the decision whether or not to resurface the patella should primarily depend on the condition of the patellar cartilage. Moreover, even if patellar morphology and congruence have no direct impact on postoperative pain and function, they are known predisposing factors to patellar tilt and instability, which leads us to recommend resurfacing for severely dysplastic patellae (Wiberg type C) regardless of the state of articular cartilage.
The principal limitations of the present are its small sample size, its relatively short follow-up, and non-consideration of preoperative AKP and KSS, which could correlate with postoperative AKP or KSS. Furthermore, the arthroscopic approach did not enable assessment of patellofemoral congruence beyond 60° of knee flexion where pressures could be greatest, and does not represent patellofemoral conditions under weight-bearing and physiological muscle loading, especially because assessments were made with patients still under general anesthesia. The main strengths are the arthroscopic visualization after wound closure, which enabled direct dynamic assessment of patellofemoral congruence with the joint capsule closed, and through various angles of early flexion. The exclusion of patients with history of patellar pain or instability also rendered a homogenous cohort which included all three patellar morphotypes.
Conclusions
While patellar morphology and patellofemoral congruence are strongly related, they are not associated with clinical outcomes or patient demographics. Considering that numerous incongruent patellofemoral joints were pain-free, and conversely, many perfectly congruent patellofemoral joints had anterior pain, the authors suppose that pain is probably caused by mechanisms other than patellofemoral pressures.
Acknowledgements
None.
Footnote
Conflicts of Interest: O Courage receives royalties or fees from Tornier SA (France). M Saffarini received fees for statistical analysis and manuscript preparation from Tornier SA (France). The other authors have no conflicts of interest to declare.
Ethical Statement: All patients provided written consent for their participation in this study, which was approved by the institutional review board (CPP-SC #2015/009).
References
- Eucomed Orthopaedic Committee. Implant Data Collection Report. 2012. Available online: http://archive.eucomed.org/newsroom/101/104/Orthopaedic-devices-increase-quality-of-life-at-good-value-for-money
- Losina E, Thornhill TS, Rome BN, et al. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am 2012;94:201-7. [Crossref] [PubMed]
- Australian Orthopaedic Association. National Joint Replacement Registry. Annual Report. Adelaide: AOA 2013. Available online: https://aoanjrr.sahmri.com/documents/10180/127202/Annual%20Report%202013?version=1.2&t=1385685288617
- Cheng T, Zhu C, Guo Y, et al. Patellar denervation with electrocautery in total knee arthroplasty without patellar resurfacing: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 2014;22:2648-54. [Crossref] [PubMed]
- Lygre SH, Espehaug B, Havelin LI, et al. Failure of total knee arthroplasty with or without patella resurfacing. Acta Orthop 2011;82:282-92. [Crossref] [PubMed]
- Pilling RW, Moulder E, Allgar V, et al. Patellar resurfacing in primary total knee replacement: a meta-analysis. J Bone Joint Surg Am 2012;94:2270-8. [Crossref] [PubMed]
- van Jonbergen HP, Reuver JM, Mutsaerts EL, et al. Determinants of anterior knee pain following total knee replacement: a systematic review. Knee Surg Sports Traumatol Arthrosc 2014;22:478-99. [Crossref] [PubMed]
- Chen K, Li G, Fu D, et al. Patellar resurfacing versus nonresurfacing in total knee arthroplasty: a meta-analysis of randomised controlled trials. Int Orthop 2013;37:1075-83. [Crossref] [PubMed]
- Kim SH, Lee S. Comparison of patellar resurfacing versus preservation in high flexion total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2015;23:1782-90. [Crossref] [PubMed]
- Arirachakaran A, Sangkaew C, Kongtharvonskul J. Patellofemoral resurfacing and patellar denervation in primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2015;23:1770-81. [Crossref] [PubMed]
- Daniilidis K, Vogt B, Gosheger G, et al. Patellar resurfacing as a second stage procedure for persistent anterior knee pain after primary total knee arthroplasty. Int Orthop 2012;36:1181-3. [Crossref] [PubMed]
- Helmy N, Greidanus NV, Masri BA, et al. To Resurface or Not to Resurface the Patella in Total Knee Arthroplasty. Clin Orthop Relat Res 2008;466:2775-83. [Crossref] [PubMed]
- Brown EC 3rd, Clarke HD, Scuderi GR. The painful total knee arthroplasty: diagnosis and management. Orthopedics 2006;29:129-36. [PubMed]
- Petersen W, Rembitzki IV, Brüggemann GP, et al. Anterior knee pain after total knee arthroplasty: a narrative review. Int Orthop 2014;38:319-28. [Crossref] [PubMed]
- Dejour D, Ntagiopoulos PG, Saffarini M. Evidence of trochlear dysplasia in femoral component designs. Knee Surg Sports Traumatol Arthrosc 2014;22:2599-607. [Crossref] [PubMed]
- Huang CH, Hsu LI, Chang TK, et al. Stress distribution of the patellofemoral joint in the anatomic V-shape and curved dome-shape femoral component: a comparison of resurfaced and unresurfaced patellae. Knee Surg Sports Traumatol Arthrosc 2014. [Epub ahead of print]. [Crossref] [PubMed]
- Kainz H, Reng W, Augat P, et al. Influence of total knee arthroplasty on patellar kinematics and contact characteristics. Int Orthop 2012;36:73-8. [Crossref] [PubMed]
- Leichtle UG, Wünschel M, Leichtle CI, et al. Increased patellofemoral pressure after TKA: an in vitro study. Knee Surg Sports Traumatol Arthrosc 2014;22:500-8. [Crossref] [PubMed]
- Tanzer M, McLean CA, Laxer E, et al. Effect of femoral component designs on the contact and tracking characteristics of the unresurfaced patella in total knee arthroplasty. Can J Surg 2001;44:127-33. [PubMed]
- Steinbrück A, Schröder C, Woiczinski M, et al. Patellofemoral contact patterns before and after total knee arthroplasty: an in vitro measurement. Biomed Eng Online 2013;12:58. [Crossref] [PubMed]
- Rodríguez-Merchán EC, Gómez-Cardero P. The outerbridge classification predicts the need for patellar resurfacing in TKA. Clin Orthop Relat Res 2010;468:1254-7. [Crossref] [PubMed]
- Takahashi A, Sano H, Ohnuma M, et al. Patellar morphology and femoral component geometry influence patellofemoral contact stress in total knee arthroplasty without patellar resurfacing. Knee Surg Sports Traumatol Arthrosc 2012;20:1787-95. [Crossref] [PubMed]
- Grelsamer RP, Saleh J, Gladstone J. Congruous versus incongruous patellar tilt--a preliminary study. Bull NYU Hosp Jt Dis 2012;70:232-4. [PubMed]
- Panni AS, Cerciello S, Maffulli N, et al. Patellar shape can be a predisposing factor in patellar instability. Knee Surg Sports Traumatol Arthrosc 2011;19:663-70. [Crossref] [PubMed]
- Monk AP, Doll HA, Gibbons CL, et al. The patho-anatomy of patellofemoral subluxation. J Bone Joint Surg Br 2011;93:1341-7. [Crossref] [PubMed]
- Smith TO, Davies L, Toms AP, et al. The reliability and validity of radiological assessment for patellar instability. A systematic review and meta-analysis. Skeletal Radiol 2011;40:399-414. [Crossref] [PubMed]
- Saffarini M, Zaffagnini S, Bignozzi S, et al. Does patellofemoral geometry in TKA affect patellar position in mid-flexion? Knee Surg Sports Traumatol Arthrosc 2015;23:1799-807. [Crossref] [PubMed]
- Merchant AC. Femoral sulcus angle measurements. Am J Orthop (Belle Mead NJ) 1997;26:820, 822.
- Wiberg G. Roentgenographic and anatomic studies on the femoropatellar joint, with special reference to chondromalacia patellae. Acta Orthop Scand 1941;12:319-410. [Crossref]
- Breugem SJ, van Ooij B, Haverkamp D, et al. No difference in anterior knee pain between a fixed and a mobile posterior stabilized total knee arthroplasty after 7.9 years. Knee Surg Sports Traumatol Arthrosc 2014;22:509-16. [Crossref] [PubMed]
- Li YL, Wu Q, Ning GZ, et al. No difference in clinical outcome between fixed- and mobile-bearing TKA: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 2014;22:565-75. [Crossref] [PubMed]