Tritanium acetabular wedge augments: short-term results
Introduction
Reconstruction of acetabular defects presents a great challenge to orthopaedic surgeons. These acetabular defects may be due to congenital causes, such as developmental dysplasia of the hip (DDH), or may be post-traumatic in origin. Crowe et al. (1), developed one of the most widely use classifications for DDH, of which grade III may require the largest degree of acetabular defect reconstruction. Acetabular defects may also occur as a result of bone loss following a failed primary total hip arthroplasty (THA), secondary to osteolysis, cup migration, or removal of implants.
Paprosky et al. (2) developed a classification of acetabular defects that recommend reconstruction options in revision THA. There are numerous publications on how to manage various acetabular defects (2-4). Due to lack of resources, the initial treatment for these types of defects was structural allografts (5,6). Later on, newer technology allowed the use of cages (7,8), jumbo cups (9-11), and most recently, acetabular augments have been added to our armamentarium (12,13). All these treatment options have been used for filling acetabular defects, but consensus for superiority of one method over others has not been reached. Lack of integration or reabsorption of allograft can happen (14), and despite precautions, transmission of infections can happen with the use of allografts (15). Following cage reconstruction, there can be increased bone loss and structural failure (16), and elevation of the center of rotation can occur after using jumbo cups (17,18). Previous studies have reported on the use and outcomes of trabecular metal acetabular augments for the reconstruction of acetabular defects (13). However, no study has been conducted evaluating augmentation of acetabular defects using tritanium acetabular wedge augments.
Thus, the purpose of this study is to present the short-term results of tritanium acetabular wedge augments for the reconstruction of acetabular defects in DDH and for revision following a failed primary THA.
Methods
A retrospective study was conducted using a prospective database at a single institution including primary and revision THA patients from January 2013 to December 2014. Patients were included if they received a tritanium acetabular wedge augment system (Restoration®, Stryker Orthopaedics, Mahwah, NJ, USA) and there was a minimum of 2-year follow-up. Patients were excluded if the tritanium acetabular wedge was not used as final implant. Tritanium is composed of a highly porous commercially pure titanium matrix.
Demographic data was collected on patients, including age, gender, body mass index (BMI), American Society of Anesthesiology classification, Charlson Comorbidity Index, and laterality. Outcomes data including Short-Form 12 (SF-36) and Harris Hip Scores (HHS) were collected and compared preoperatively and postoperatively. Preoperative classification was performed using Paprosky classification for revision THA cases (2) and Crowe classification for DDH cases (1), and radiographic analysis of the acetabulum at last follow-up was assessed using DeLee and Charnley’s classification system (19). This study received Institutional Review Board approval prior to commencement. Written informed consent was obtained from all patients.
Statistical analysis
Demographic data was presented as descriptive data. Preoperative outcomes were compared to postoperative outcomes using paired t-tests. Statistical significance was determined by P<0.05. SPSS (IBM, Armonk, New York, USA) version 23.0 was used to perform statistical analysis.
Results
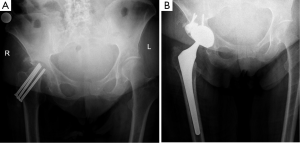
There were a total of 8 patients that underwent surgery for primary or revision THA where tritanium acetabular wedge augments were used during the study period. These augments were used in 4 revision THA patients, 3 DDH patients, and 1 patient with posttraumatic arthritis. The demographics of the patient population are presented in Table 1.
Full table
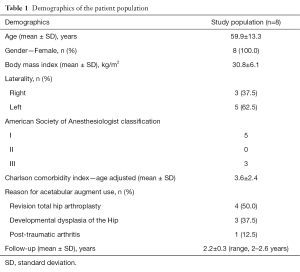
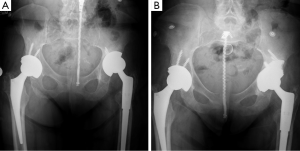
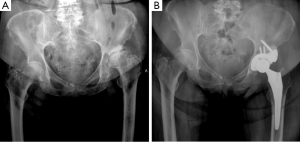
Revision THA patients underwent revision for aseptic loosening (3) and periprosthetic joint infection (1); all of which resulted in superior migration of the acetabular component with Paprosky IIB classification. Figure 1A demonstrates the preoperative imaging of a revision THA patient with superior and vertical migration of the acetabular cup, while Figure 1B demonstrates the postoperative radiograph of the acetabular wedge augment to reconstruct the superior defect. DDH patients, of which 2 were Crowe III and 1 was Crowe IV, often presented with severe degenerative joint disease and supero-lateral subluxation of the femoral head (Figure 2A), and acetabular wedges were placed supero-laterally (Figure 2B). The posttraumatic arthritis was a result of a right displaced femoral neck fracture, which was treated with three cannulated screws. The patient developed osteonecrosis with femoral head collapse (Figure 3A), which was treated with conversion THA using acetabular augments since the protruding cannulated screws damaged some of the superior acetabular bone (Figure 3B).
The average follow-up was 2.2 years ±0.3 (range, 2–2.6 years). During the follow-up period, there was one closed reduction for early dislocation (six weeks after surgery) and no open revision surgery. At the latest radiographic follow-up, there were no lucent lines in DeLee and Charnley Zones I, II or III.
With regards to outcomes, the SF-36 physical significantly improved from preoperative assessment [mean ± standard deviation (SD), 29.6±2.2] to postoperative assessment (52.2±8.7, P=0.003). The SF-36 mental score also significantly improved from preoperative values (34.5±4.5) to postoperative values (52.2±7.5, P=0.003). Total HHS scores also significantly improved comparing preoperative values (27.8±19.1) to postoperative values (85.0±13.7, P=0.02); the pain score improved (preoperative 5.0±10.0, postoperative 38.0±12.0, P=0.01) and the function score improved (preoperative 18.8±13.9, postoperative 43.0±5.2, P=0.02).
Discussion
Acetabulum defects present a challenge to the adult reconstruction surgeon. Whether the cause of such defects is DDH or osteolysis present in a failed THA, reconstruction needs to be addressed accordingly (2-4). Technology has evolved from the use of structural allografts (5,6) to the use of cages (7,8), jumbo cups (9-11), and acetabular augments (12,13), depending on the size and location of the defect. Superiority of one over the others has not been reached (20). Allografts can reabsorb or fail to integrate (14), and continue to be a risk for transmission of infections (15). Structural failure is a concern seen following reconstructions with cages (16). Elevation of the center of rotation is known to be the result in some instance when jumbo cups are used (17,18). There is scant literature on the outcomes of acetabular wedge augments, and these publications are not exclusive for acetabular augments and only report on trabecular metal augments (13,16). Thus, the purpose of our study was to evaluate the ability of a tritanium acetabular wedge system to fill acetabular defects after primary and revision THA.
The overall experience with the tritanium acetabular wedge augment in this short follow-up case series report has being excellent, as no early failures have been detected in any of the patients in our study. This reflects findings in literature on other acetabular augments, as early follow-up with trabecular metal augments demonstrated improved clinical outcomes and low revision rates (21-23), and mid-term follow-up with these same acetabular augments report 92% survivorship at ten years (12). Other trabecular titanium augments have shown less robust results, but have demonstrated improved functional scores at a minimum of 2-year follow-up (13). Porous tantalum metal has also been used in conjunction with impaction bone grafting (24,25) and for doing one-stage exchange arthroplasty for periprosthetic hip infections (26).
While this is the first study to report outcomes based results on the tritanium acetabular wedges, there are limitations to this study. This is a small series of patients with limited follow-up, as there are limited indications for using acetabular wedges. This is also a non-randomized study, and this study would have been strengthened with a comparison group, such as allograft or acetabular wedges composed of different materials.
Despite these limitations, this is the first study that reports the short-term results of tritanium acetabular wedges in a case series of patients that demonstrate good clinical radiographic outcomes. Further longitudinal studies with mid- to long-term follow-up are needed to further evaluate these promising findings.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study received Institutional Review Board approval prior to commencement and written informed consent was obtained from all patients.
References
- Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am 1979;61:15-23. [PubMed]
- Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty 1994;9:33-44. [Crossref] [PubMed]
- Jain S, Grogan RJ, Giannoudis PV. Options for managing severe acetabular bone loss in revision hip arthroplasty. A systematic review. Hip Int 2014;24:109-22. [Crossref] [PubMed]
- Abolghasemian M, Sadeghi Naini M, Tangsataporn S, et al. Reconstruction of massive uncontained acetabular defects using allograft with cage or ring reinforcement: an assessment of the graft's ability to restore bone stock and its impact on the outcome of re-revision. Bone Joint J 2014;96-B:319-24. [Crossref] [PubMed]
- Abdel MP, Stryker LS, Trousdale RT, et al. Uncemented acetabular components with femoral head autograft for acetabular reconstruction in developmental dysplasia of the hip: a concise follow-up report at a mean of twenty years. J Bone Joint Surg Am 2014;96:1878-82. [Crossref] [PubMed]
- Arts JJ, Verdonschot N, Buma P, et al. Larger bone graft size and washing of bone grafts prior to impaction enhances the initial stability of cemented cups: experiments using a synthetic acetabular model. Acta Orthop 2006;77:227-33. [Crossref] [PubMed]
- Paprosky W, Sporer S, O'Rourke MR. The treatment of pelvic discontinuity with acetabular cages. Clin Orthop Relat Res 2006.183-7. [Crossref] [PubMed]
- Pieringer H, Auersperg V, Böhler N. Reconstruction of severe acetabular bone-deficiency: the Burch-Schneider antiprotrusio cage in primary and revision total hip arthroplasty. J Arthroplasty 2006;21:489-96. [Crossref] [PubMed]
- Gustke KA, Levering MF, Miranda MA. Use of jumbo cups for revision of acetabulae with large bony defects. J Arthroplasty 2014;29:199-203. [Crossref] [PubMed]
- Lachiewicz PF, Soileau ES. Fixation, survival, and dislocation of jumbo acetabular components in revision hip arthroplasty. J Bone Joint Surg Am 2013;95:543-8. [Crossref] [PubMed]
- Rees HW, Fung DA, Cerynik DL, et al. Revision total hip arthroplasty without bone graft of high-grade acetabular defects. J Arthroplasty 2012;27:41-7. [Crossref] [PubMed]
- Whitehouse MR, Masri BA, Duncan CP, et al. Continued good results with modular trabecular metal augments for acetabular defects in hip arthroplasty at 7 to 11 years. Clin Orthop Relat Res 2015;473:521-7. [Crossref] [PubMed]
- Steno B, Kokavec M, Necas L. Acetabular revision arthroplasty using trabecular titanium implants. Int Orthop 2015;39:389-95. [Crossref] [PubMed]
- Nousiainen MT, Maury AC, Alhoulei A, et al. Long-term outcome of shelf grafts in total hip arthroplasty for developmental hip dysplasia. Orthopedics 2009.32. [PubMed]
- Lomas R, Chandrasekar A, Board TN. Bone allograft in the U.K.: perceptions and realities. Hip Int 2013;23:427-33. [Crossref] [PubMed]
- Hansen E, Shearer D, Ries MD. Does a cemented cage improve revision THA for severe acetabular defects? Clin Orthop Relat Res 2011;469:494-502. [Crossref] [PubMed]
- Nwankwo CD, Ries MD. Do jumbo cups cause hip center elevation in revision THA? A radiographic evaluation. Clin Orthop Relat Res 2014;472:2793-8. [Crossref] [PubMed]
- Nwankwo C, Dong NN, Heffernan CD, et al. Do jumbo cups cause hip center elevation in revision THA? A computer simulation. Clin Orthop Relat Res 2014;472:572-6. [Crossref] [PubMed]
- DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res 1976.20-32. [PubMed]
- Deirmengian GK, Zmistowski B, O'Neil JT, et al. Management of acetabular bone loss in revision total hip arthroplasty. J Bone Joint Surg Am 2011;93:1842-52. [Crossref] [PubMed]
- Grappiolo G, Loppini M, Longo UG, et al. Trabecular Metal Augments for the Management of Paprosky Type III Defects Without Pelvic Discontinuity. J Arthroplasty 2015;30:1024-9. [Crossref] [PubMed]
- Elganzoury I, Bassiony AA. Early results of trabecular metal augment for acetabular reconstruction in revision hip arthroplasty. Acta Orthop Belg 2013;79:530-5. [PubMed]
- Del Gaizo DJ, Kancherla V, Sporer SM, et al. Tantalum augments for Paprosky IIIA defects remain stable at midterm followup. Clin Orthop Relat Res 2012;470:395-401. [Crossref] [PubMed]
- Gehrke T, Bangert Y, Schwantes B, et al. Acetabular revision in THA using tantalum augments combined with impaction bone grafting. Hip Int 2013;23:359-65. [Crossref] [PubMed]
- Borland WS, Bhattacharya R, Holland JP, et al. Use of porous trabecular metal augments with impaction bone grafting in management of acetabular bone loss. Acta Orthop 2012;83:347-52. [Crossref] [PubMed]
- Klatte TO, Kendoff D, Sabihi R, et al. Tantalum acetabular augments in one-stage exchange of infected total hip arthroplasty: a case-control study. J Arthroplasty 2014;29:1443-8. [Crossref] [PubMed]


