
Infection control management strategy for operating room during COVID-19 pandemic
Introduction
Coronavirus disease 2019 (COVID-19) has spread rapidly worldwide. Globally, as of 7:24 PM CEST, 23 June 2022, 539,893,858 confirmed cases of COVID-19, including 6,324,112 deaths, have been reported to the World Health Organization (1). The numbers of confirmed cases and deaths continue to increase. COVID-19 is caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This virus can easily spread from person to person through droplets and microparticles exhaled from an infected person (2,3). At present, the prevention and control of COVID-19 remains a formidable challenge for governments and health agencies around the world.
Given that the number of confirmed cases continues to increase dramatically, it is increasingly likely that COVID-19 patients will require emergency surgeries in the operating room (OR). Many factors during surgery may accelerate the spread of COVID-19, such as frequent contact with the patient in proximity, exposure to the patient’s bodily fluids, multi-person participation in a confined space, indirect contact through anesthesia apparatus, and the viral aerosol produced by the operation. It is extremely difficult to prevent COVID-19 from spreading during surgery on a COVID-19 patient; thus, it is important to establish a set of strategy to prevent COVID-19 from spreading in the OR. A few recommendations for the prevention of COVID-19 during surgery have been issued (4); however, comprehensive and specific OR management strategies for the perioperative COVID-19 prevention process are limited.
The Fifth Affiliated Hospital of Sun Yat-Sen University is a designated hospital for COVID-19 patients in the urban cluster on the west bank of Pearl River in Guangdong Province, China. Since the outbreak of COVID-19 in Wuhan at the end of 2019, more than 200 confirmed and 300 suspected cases of COVID-19 have been admitted to our hospital. We have performed emergency surgery on 1 patient with acute calculous cholecystitis and choledocholithiasis who was confirmed to have COVID-19 (5), and dozens of emergency surgeries on patients who were suspected to have COVID-19. We have achieved the satisfactory result of zero COVID-19 infections in the OR.
Based on our COVID-19 prevention experience in the OR, we developed this perioperative infection control management strategy to prevent COVID-19 from spreading in the OR during the COVID-19 pandemic. This strategy included COVID-19 knowledge training, surgery arrangement procedures, OR area arrangements, preoperative preparation procedures, procedures for wearing and removing personal protective equipment (PPE), anesthesia management, intraoperative management, and post-operative management. We hope this management strategy will help OR administrators around the world to develop some efficient infection prevention and control processes to prevent COVID-19 from spreading in the OR during the COVID-19 pandemic.
COVID-19 knowledge training
During the early stage of a COVID-19 outbreak, the number of elective surgeries in the OR should decrease due to government restrictions on traffic. This period should be taken full advantage of to conduct comprehensive COVID-19 knowledge training. Comprehensive COVID-19 knowledge training, including training on scientific prevention behaviors, should decrease the spread of COVID-19 (6,7). The training should involve all staff in the OR, including healthcare workers and non-healthcare workers, as all such staff may be exposed to the virus. Non-healthcare workers are at an increased risk of infection during a COVID-19 outbreak, as they have more exposure to the virus, but less medical knowledge to protect themselves. Given that SARS-CoV-2 can spread through respiratory droplets, the training should not be held in a crowded room. Remote online or video training should be provided. The director of the OR needs to monitor the training effect and re-train staff as necessary.
The COVID-19 training courses cover:
- The etiological features, epidemiological characteristics, clinical manifestations, clinical classification, diagnostic criteria, and treatment of COVID-19;
- Occupational health and safety for health workers during the COVID-19 epidemic;
- Hand hygiene;
- Wearing and removing PPE;
- Surgery arrangement procedures for patients’ suspected or confirmed to have COVID-19;
- COVID-19 medical waste disposal procedures;
- A COVID-19 prevention and control policy issued by the government and hospitals.
Surgery arrangement process during the COVID-19 pandemic
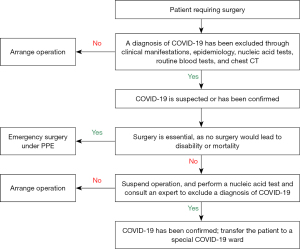
In principle, elective surgery must be suspended if a patient has been confirmed to have or is suspected to have COVID-19. Emergency surgeries should only be scheduled in situations in which not undergoing surgery would lead to disability or mortality. The surgery arrangement process during COVID-19 pandemic is shown in Figure 1. In making surgery arrangements during the COVID-19 pandemic, the following approaches should be adopted:
- For all surgical patients, a diagnosis of COVID-19 should first be excluded based on clinical manifestations, epidemiology, nucleic acid tests, routine blood tests, and chest computed tomography (CT);
- For patients suspected or confirmed to have COVID-19, elective surgeries should not be scheduled. Emergency surgeries should only be scheduled in situations in which not undergoing surgery would lead to disability or mortality;
- For patients suspected to have COVID-19 who require emergency surgeries, the patients should be treated as if a diagnosis of COVID-19 has been confirmed, and a diagnosis of COVID-19 should only be excluded following expert consultation.
OR area arrangements for COVID-19 surgery
A negative-pressure operation room (NPOR) that can prevent contaminated air from flowing out of the OR is preferred for COVID-19 patients (8). The negative-pressure system should be turned on 30 minutes before the operation to maintain room pressure at –5 to –10 Pa. However, as most hospitals do not have a NPOR, an isolated normal pressure OR with an isolated air exchange system should be used for COVID-19 patients who are too critical to transfer. A non-isolated positive-pressure OR cannot be used for COVID-19 patients, as the positive pressure can blow the virus out of the OR and contaminate the surrounding areas. Some ORs can adjust the volume of air output and input, such that if the air output of a positive-pressure OR is increased and continuously greater than the air input, the positive-pressure OR can be temporarily converted into a negative-pressure OR in which the pressure may reach –5 Pa. The OR area for COVID-19 patients should be physically separated from other routine ORs with a specially designated hallway to enter and exit. A clean zone and a buffer zone should be set up outside the contaminated zone to provide an isolated space for wearing and removing PPE.
Preoperative preparation procedures
- Sufficient PPE should be provided to all the healthcare workers and cleaners involved in the surgery. The minimum PPE for the OR includes a disposable surgery coat, surgery cap, surgery gloves, long-sleeved waterproof disposable coverall, N95 medical mask, face shield, and waterproof shoe covers (9).
- Review the COVID-19 patient’s physical condition preoperatively by reading the electronic medical records and avoid unnecessary contact with the patient outside the OR.
- All surgical and anesthetic items (e.g., medical equipment, surgical instruments, medical consumables, and anesthetic) should be readied in the OR in advance. All the items prepared for surgery in the OR should be 1-way; that is, they should only enter and not leave the OR.
- The anesthetic machine must be checked and put on standby in advance.
- Any unnecessary items and equipment should be removed from the OR to prevent virus infection.
- Areas that may come in direct or indirect contact with patients and are difficult to clean (e.g., surgery mattresses, computer monitors, mice, and keyboards) should be covered with a transparent waterproof plastic wrap.
- Patients should be transported between the isolation ward and the OR through a dedicated hallway with the cooperation of healthcare workers and transport workers wearing PPE. Patients should wear an N95 medical mask and be covered with medical non-woven disposable items during the entire transportation.
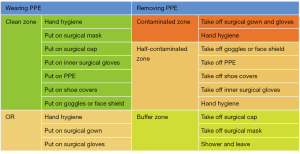
Wearing and removing PPE
The proper use of PPE, which protects against contact, droplet, and airborne transmission can prevent healthcare workers from being exposed to the virus (10). An appropriate procedure for wearing and removing PPE can provide the highest level of protection, and thus strengthen occupational safety and prevent the virus from spreading between healthcare workers and COVID-19 patients (11). A PPE supervisor should be present to oversee the healthcare workers and ensure they are correctly wearing and removing the PPE to achieve reliable protection. The procedure recommended for wearing and removing PPE is detailed in Figure 2.
Anesthesia management
Both regional anesthesia and general anesthesia can be used in COVID-19 patients, but regional anesthesia techniques are preferable (12,13). Regional anesthesia techniques, including Intervertebral anesthesia and regional nerve block anesthesia, do not require intubation and extubation, which can produce viral aerosols. If general anesthesia is required for the surgery, it is important to avoid SARS-CoV-2 transmission during endotracheal intubation. Rapid sequence induction and intubation are recommended (14).
The most familiar endotracheal intubation tool should be chosen to perform the intubation, and a visual laryngoscope that can increase the operating distance between the anesthesiologist and the patient during intubation is a primary tool for COVID-19 patients. A fiber electronic bronchoscope may also increase the operating distance; however, it is not recommended for use by inexperienced anesthesiologists, as its use may increase the time of intubation and the risk of virus infection.
Before intubation, the handle and the display screen of the laryngoscope should be covered with a disposable transparent protective film to avoid contamination. Before induction, the patient should be pre-oxygenated and denitrogenated sufficiently. To prevent the spread of viral aerosols, 2 layers of wet gauze should be used to cover the patient's mouth and nose before performing the mask ventilation, as this method does not affect the ventilation and oxygenation. Once the patient’s respiration disappears, oxygen should be administered by a mask in the mode of mechanical ventilation. The tidal volume should not be too large; 6–8 mL/kg is appropriate. The endotracheal intubation should be performed approximately 90 seconds after the induction of anesthesia. Adequate doses of opioids and muscle relaxants should be administered to avoid choking.
In total, 3 disposable heat and moisture exchange filters should be used (15,16); 1 between the endotracheal tube and the respiratory circuit, and 1 for the air inlet and air outlet of the anesthesia machine to minimize the probability of the virus entering breath circuits and the anesthesia machine.
At a minimum, anesthetists should wear an N95 mask and a face shield during endotracheal intubation or wear positive-pressure ventilation equipment if conditions permit. Other protective instruments, such as an Aerosol Box (17) or protective sleeve (18), can also be used to protect healthcare workers from viral aerosol pollution.
In principle, the endotracheal tube should be removed in the OR before the patient returns to the ward; however, patients with unstable vital signs will need to be sent to the intensive care unit with the endotracheal tube.
During extubation, agitation and coughing in patients should be avoided as much as possible, as such behaviors increase the production of virus aerosols, and thus increase the chances of COVID-19 transmission. Inhalation anesthetics should be stopped 30 minutes before the end of surgery. It is highly recommended that dexmedetomidine, which can effectively attenuate agitation, be administrated during surgery. Tracheal sputum suction should be performed under deep sedation before extubation. For the same reason, extubation should be performed under sedation if the patient resumes spontaneous respiration and the tidal volume and respiratory rate are sufficient to maintain normal oxygen saturation.
Intraoperative management
- The door of the OR must remain closed during the operation to prevent the virus from spreading outside the OR through air movement. All the medical materials, medicines, and equipment needed for the operation should be fully prepared before the patient enters the OR. All the medical materials and medicines left following the operation must be disposed of according to COVID-19 medical waste disposal procedures and cannot be used again.
- If regional anesthesia is used for the surgery, the patient should wear an N95 mask throughout the whole operation to prevent the virus spreading.
- The surgical team should be well protected by PPE during the surgery. It is highly recommended a PPE supervisor be employed to check that the healthcare workers wear and remove the PPE properly.
- The surgical team should be well-trained, cooperative, and operate with high precision and cautiousness to reduce aerosol production, avoid unintentional injury to other surgeons and nurses, and avoid damaging the PPE.
- An electrocautery that can reduce the time of surgically separating tissue should be set as low as possible to reduce the smoke. Smoke must be sucked away as quickly as possible to avoid the virus spreading through the smoke.
- When pollution occurs, it should be contained immediately. A small amount of pollution can be wiped away using disposable water-absorbing fabric with 1,000–2,000 mg/L chlorine-containing disinfectant (19). A large amount of pollution should be completely covered with disinfectant powder or an absorbent material, and soaked in 500 mg/L of disinfectant containing chlorine for >30 minutes (19). The pollution materials should be disposed of according to the COVID-19 medical waste disposal procedures.
- Touch screen equipment and screens in the OR should be wrapped with transparent plastic film to prevent the virus from surviving on surfaces, such as grooves, buttons, computer mice, and screen peripheries.
- Goggles and condensation: If goggles, glasses, and face shields are worn, condensation from breath may easily form on the surface of the goggles and face shields, affecting visibility. In our experience, wiping hand sanitizer on the inside surface of the goggles and face shields prevents condensation from forming.
- During the operation, a runner should be stationed outside the OR in case additional medications, materials, or equipment are needed.
Post-operative management
The primary goal of post-operative management is to prevent viruses from remaining, multiplying, and spreading. It is important to ensure that terminal disinfection is carried out to keep the sites, items, and substances virus-free. This should be completed with the cooperation of healthcare workers and cleaners who are familiar with the SARS-CoV-2 disinfection process.
Disposal of medical waste
In principle, the disposable of medical materials is the best way for COVID-19 surgery patients to avoid the risk of iatrogenic infection that is caused by the repeated use of medical materials. All the waste in a COVID-19 OR should be considered medical waste, regardless of whether or not it has come into direct contact with patients. The medical waste should be carefully put into a double-layered medical garbage bag. The medical garbage bag should be tightened, sealed, sprayed with 75% alcohol, and marked with a label that states, “COVID-19 infection, (the department), and (the date)” before being transported from the contaminated OR. Medical waste should be transported to designated locations for treatment through dedicated hallway by well-trained cleaners.
Post-operative disinfection
Contaminants (blood, secretions, and vomitus of patients)
Any visible contaminant (e.g., the tissue debris, blood, secretions, and vomitus of patients) should be removed as soon as possible, and the site should be disinfected with 1,000 mg/L of disinfectant containing chlorine. If not removed immediately, the contaminant should be covered with disinfectant powder containing water-absorbing ingredients, or disposable water-absorbing materials, and soaked in 500 mg/L of disinfectant containing chlorine for >30 minutes (19). Direct contact with contaminants in the removal procedure should be avoided. Surgical suction bottles should be half pre-filled with 2,000 mg/L of disinfectant containing chlorine mixed with a surgical aspirate. After the removal of the contaminants, the surfaces of the contaminated objects need to be thoroughly disinfected.
Surgical instruments
As surgical instruments are contaminated with blood, secretions, and tissue debris, they carry a high risk of spreading viruses, and should be disinfected before being cleaned. Disposable surgical instruments should be discarded as medical waste after the operation, while reusable surgical instruments should be put in a hollow metal wire basket and soaked in 500 mg/L of disinfectant containing chlorine for >30 minutes. Surgical instruments should be disassembled to increase their contact area with the disinfectant. After being soaked in 500 mg/L of disinfectant containing chlorine for 30 minutes, it is recommended that the metal instruments be cleaned with water to avoid oxidation and rust, as metal instruments are easily corroded by highly oxidizing disinfectant containing chlorine. After the above process, the surgical instruments can be cleaned and sterilized as per the routine process by workers wearing PPE.
Floors, walls, and other surfaces
After the operation, the floors, walls, and other surfaces should be sprayed from outside to inside with 1,000 mg/L of disinfectant containing chlorine at the ratio of 100–300 mL/m2, and this should be repeated again 30 minutes later. Any visible contaminants on the surfaces, should first be remove, and then the surfaces should be sprayed or wiped with 1,000 mg/L of disinfectant containing chlorine.
Air sterilization
As SARS-CoV-2 can form aerosols suspended in the air, the OR should be air-sterilized after surgery. The methods of air disinfection in the OR include spray, fumigation, and ultraviolet light. The principle of the spray disinfection method is to atomize the disinfectant into tiny particles and spray it evenly in the air to ensure it comes into full contact with the microbial particles and kills the microorganisms in the air. Hydrogen peroxide (3%), 5,000 mg/L of peracetic acid, or 1,000 mg/L of chlorine monoxide disinfectant can be added to an electric ultra-low volume sprayer and sprayed at a dosage of 20–30 mL/m3 by disinfecting personnel and then sprayed in the following order: up to down, left to right, inside to outside, and surface to space. The doors and windows should be closed before spraying and opened 60 minutes after spraying.
Ultraviolet disinfection could reduce the risk of bacterial and viral medical-associated infections by killing bacteria and viruses on surfaces and in the air (20). Given that UV disinfection cannot reach the shaded areas and it is difficult to sanitize grooves and corners by surface disinfection, OR disinfection after the surgery of COVID-19 patients must combine these 2 disinfection procedures to avoid any cleaning failures due to human and environmental factors.
Pathology specimen management
The pathological tissue should be carefully placed in a double leak-proof specimen bag and fixed with 20% formaldehyde as soon as possible. After being sealed and sprayed with 75% alcohol, the specimen bag should be put into a special storage container or bag. This storage container or bag should be labeled as follows: “COVID-19 infection, (the department), and (the date)”. The container or bag should then be transported to the Pathology Department for further processing by a well-trained worker wearing PPE. Automatic transport systems cannot be used for COVID-19 specimens.
Acknowledgments
Funding: This study was supported by COVID-19 Infection Prevention and Control Emergency Technology Project of Zhuhai City (No. ZH22036302200020PWC).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://atm.amegroups.com/article/view/10.21037/atm-22-4850/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Global situation of COVID-19. Available online: https://covid19.who.int/?mapFilter=cases.
- Ahn DG, Shin HJ, Kim MH, et al. Current Status of Epidemiology, Diagnosis, Therapeutics, and Vaccines for Novel Coronavirus Disease 2019 (COVID-19). J Microbiol Biotechnol 2020;30:313-24. [Crossref] [PubMed]
- In 't Veen JCCM, de Hond M, Boerstra AC. Viral transmission in COVID-19: the role of the aerosol. Ned Tijdschr Geneeskd 2020;164:D5399. [PubMed]
- Dexter F, Parra MC, Brown JR, et al. Perioperative COVID-19 Defense: An Evidence-Based Approach for Optimization of Infection Control and Operating Room Management. Anesth Analg 2020;131:37-42. [Crossref] [PubMed]
- Hong X, He J, Li P, et al. Evidence of SARS-CoV-2 infection in gallbladder and aggravating cholecystitis to septic shock: a case report. Ann Transl Med 2021;9:1631. [Crossref] [PubMed]
- Aleanizy FS, Alqahtani FY. Awareness and knowledge of COVID-19 infection control precautions and waste management among healthcare workers: Saudi cross-sectional study. Medicine (Baltimore) 2021;100:e26102. [Crossref] [PubMed]
- Shafiq M, Elharake JA, Malik AA, et al. COVID-19 Sources of Information, Knowledge, and Preventive Behaviors Among the US Adult Population. J Public Health Manag Pract 2021;27:278-84. [Crossref] [PubMed]
- Al-Benna S. Negative pressure rooms and COVID-19. J Perioper Pract 2021;31:18-23. [Crossref] [PubMed]
- Choosing the Right PPE for COVID-19 2022 [updated February 25, 2022. Available online: https://www.cdc.gov/infectioncontrol/projectfirstline/resources/ppe-covid-19.html#.
- Moore KA, Bouchoucha SL, Buchwald P. A comparison of the public's use of PPE and strategies to avoid contagion during the COVID-19 pandemic in Australia and Germany. Nurs Health Sci 2021;23:708-14. [Crossref] [PubMed]
- Daigle P, Leung V, Yin V, et al. Personal protective equipment (PPE) during the COVID-19 pandemic for oculofacial plastic and orbital surgery. Orbit 2021;40:281-6. [Crossref] [PubMed]
- Mejía-Terrazas GE, López-Muñoz E, Vilchis-Rentería JS, et al. COVID-19: Regional Anesthesia, Benefits, and Practical Recommendations. Asian J Anesthesiol 2021;59:83-95. [PubMed]
- Herman JA, Urits I, Kaye AD, et al. COVID-19: Recommendations for regional anesthesia. J Clin Anesth 2020;65:109885. [Crossref] [PubMed]
- Orser BA. Recommendations for Endotracheal Intubation of COVID-19 Patients. Anesth Analg 2020;130:1109-10. [Crossref] [PubMed]
- De Seta D, Carta F, Puxeddu R. Management of tracheostomy during COVID-19 outbreak: Heat and moisture exchanger filter and closed suctioning system. Oral Oncol 2020;106:104777. [Crossref] [PubMed]
- Garnier M, Julian N, Velly L. Heat moisture exchange/high-efficiency particulate filters and the risk of contamination of the ventilatory circuit and patient environment with SARS-CoV-2: A brief report. Anaesth Crit Care Pain Med 2022;41:101065. [Crossref] [PubMed]
- Fong S, Li E, Violato E, et al. Impact of aerosol box on intubation during COVID-19: a simulation study of normal and difficult airways. Can J Anaesth 2021;68:496-504. [Crossref] [PubMed]
- Chen C, Shen N, Chen L, et al. Application of a protective sleeve is associated with decreased occupational anxiety during endotracheal intubation: a randomized controlled trial. BMC Anesthesiol 2021;21:251. [Crossref] [PubMed]
- Zhang S, Wang C, Lin M, et al. Analysis of the Virus Contamination and Disinfection Effect in Isolation Ward of Patients With COVID-19. Front Public Health 2020;8:486. [Crossref] [PubMed]
- Strazzi-Sahyon. Ultraviolet irradiation as a disinfection protocol during COVID-19 outbreak for dental practices. Photodiagnosis Photodyn Ther 2020;32:102079. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)


