Rotational alignment of the femoral component in total knee arthroplasty
Introduction
A correct limb alignment, with good joint kinematics, without pain and long time survivorship is to obtained for a very good total knee arthroplasty (TKA).
One critical step in good TKA is the correct sizing and alignment of femoral component in three dimensions, mainly on the sagittal plane and considering rotational alignment.
The rotational alignment establishes the symmetry of flexion gap (1,2), this is the key point to obtain a stable knee during all range of motion and a correct joint kinematic.
Any misplacement with asymmetric flexion gap will lead to varus or valgus instability during knee flexion (3,4) with pain in particular in mid-flexion. Knee with medial laxity in flexion (valgus-stress) is statistically painful, while it is more tolerated a little lateral laxity (in varus-stress) (5,6).
Symptomatic laxity can lead to an early failure of the prosthetic implant. Several papers emphasize the detrimental effect of femoral component’s internal rotation; which leads to a valgus alignment during flexion, with mechanical overload on medial side of the joint with consequential implant failure (7).
The femoral component rotational alignment influences also the correct patellar tracking.
The femoral component misplacement in medial translation or internal rotation leads to patellofemoral complications with anterior knee pain syndrome and maltracking causing patellar subluxation and even patellar dislocation (8,9).
There are several landmarks and references to obtain a correct alignment (10-12).
We describe different methods to align the femoral component. The choice of a method depends on the personal surgeon’s experience and on the instruments he is going to use.
Despite everyone is being convinced of the clinical importance of correct rotational alignment, there is no widely accepted surgical technique leading to superior results.
The authors believe that a modern combined method, considering ligamentous tension even with bone references may be more reliable and reproducible in different arthritic deformity correction during TKA Figure 1.
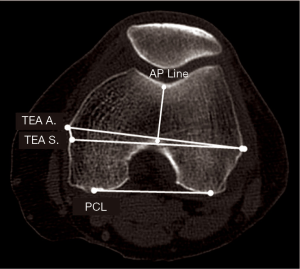
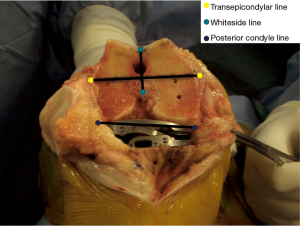
There is a possible method: surgeon uses bone landmarks of the femur intraoperatively as a reference as shown in Figure 2:
- Transepicondylar axis (TEA): anatomical (lateral to medial epicondyle) or surgical (medial sulcus lateral epicondyle) axis;
- Posterior condylar line;
- Trochlear AP axis, as known as whiteside line.
A second method achieves the rotational alignment of femoral component by specific instruments in order to obtain rectangular gap space tensioning the ligamentous apparatus. It’s necessary to use spacers of known thickness (gap based technique) or tensors (tension based technique). In tension based technique the force applied could be defined manually by surgeon’s perception or measured with specific sensor-tensor tools.
The spacer or the tensor must be inserted between tibial resection plane and posterior femoral condyle with knee at 90° of flexion.
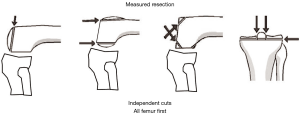
Surgical techniques using bone landmarks allow independent bone cuts and are defined measured resection technique, Figure 3 shows the cuts obtained by the use of this technique.
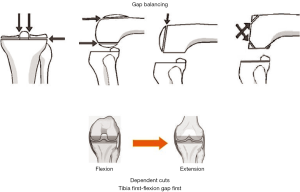
The gap balanced technique requires dependent bone cut. The first is the tibial cut (master cut) and the next cuts follow and depend on it.
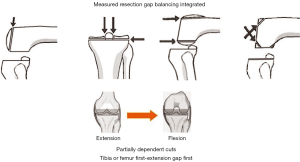
The third method (preferred by the authors) provides cuts that depend partially on each other. There are two independent master cuts (distal femoral and tibial) and the following cuts are dependent on these ones.
After the primary cuts the surgeon defines the size and the symmetry of extension gap with spacer blocks or tensors consequentially performing the ligamentous releases when necessary.
The size and the position of the femoral component, including specifically the femoral rotation, are defined using the gap balancing technique instruments, but the reference of bone landmarks (TEA and whiteside line).
Surgical techniques
Bone landmarks
Transepicondylar axis (TEA)
It is defined as the axis connecting lateral and medial epicondyles.
Theoretically it is an excellent reference for femoral rotation, but during surgery the epicondyles are not always so easy to be identified. If the reference on lateral condyle is unique on the apex of bony prominence, there are two possible references for the medial condyle:
- The apex of the medial prominence defines the anatomical TEA (A TEA);
- The surgical TEA (S TEA) connects the lateral condyle and the medial sulcus on femur.
During surgery the right determination of bone landmarks is hard to be found because of possible deformities and surgical approach used.
Several papers (13,14) showed a great inter and intra-observer variability in TEA landmarks leading to mean femoral component misplacement of 3.5° (SD ±5°) (8). For that reason TEA should not be the only reference for femoral component rotation, since it has very low reproducibility and reliability level.
Posterior condyle line
It’s an easy to find and reliable reference.
It is used extensively in the knee artrhoplasty instruments because with all-in-one tool it is possible to define the size, the placement in the anterior-posterior plane and the rotation of the femoral component.
The instruments have a bearing surface on the posterior condyles and a reference to the anterior cortex in order to define the size and the anterior-posterior placement. Once these parameters are set it is possible to choose the rotation of the femoral component.
This method, although very employed, presents some critical points.
The presence of important wear of one of the two posterior condyles, (e.g., lateral condyle in the case of valgus knee or medial condyle in unstable varus knee), can lead to an error in the choice of the rotation, as well as the femoral size, for positioning the bearing surface on a particularly worn condyle.
In addition, it should be understood that the determination of the rotation on the basis of posterior condyles only, if not associated with other references, can lead to an arbitrary choice.
Antero-posterior (AP) whiteside line
This is defined as the line connecting the lowest point of the patellar groove and the top of the intercondylar notch.
It is easily identified intraoperatively and somewhat reliable.
In some cases prior to its identification, it is necessary to remove osteophytes that may deform the intercondylar notch.
It has a certain correlation with the TEA but is more easily identifiable.
It provides a landmark for reliable and accurate valuation of patellar tracking and a second landmark when the size and the position of femoral component is measured using posterior condyle line as a reference.
Gap based technique
This technique is without specific bone landmarks. Reference for rotation is obtained with knee flexed at 90° and the ligamentous apparatus properly tensioned in order to get a rectangular flexion gap.
Theoretically, it provides a self-alignment of the element independently on the type and degree of deformity (torsional too).
The size of the gap, however, is strictly dependent on the tibial cut.
The original method requires a tibia first resection in order to provide the flexion gap, then adjusting the subsequent resections in order to balance the extension gap consequently.
The main limitation of this method is that it could lead to move the joint line generally in a proximal and anterior direction. This provides a prosthesis stable and balanced in extension and 90° flexion, but potentially unstable in mid flexion.
Moreover bone landmarks as a second check are not to be used: this could lead to femoral malrotation if tibial resection is incorrect or if ligamentous apparatus is unreliable due to surgical variation.
Figure 4 shows the cuts obtained by the use of the gap-based technique.
Combined technique
You start this technique by getting a symmetrically extension gap and performing the primary bone resections (distal femur and tibia) independently.
The distal femoral resection is measured so as to avoid the displacement of the joint line. The quantity of bone resected corresponds to the thickness of the distal femoral component. The angle of distal resection is determined by radiographic planning that takes into consideration the patient’s morphotype.
After the primary resections, if the extension gap is asymmetrical, it is necessary to perform a ligamentous release in order to obtain a symmetric space, and the gap size finally is measured with spacer block or tensors.
The next step, with knee flexed at 90°, is defining the size and the position of the femoral component in the three planes of space, including rotation, which allows to balance the flexion gap size to the extension one and to have a symmetric flexion gap, with a specific tool as shown in Figure 5.
There is no further ligamentous release in flexion.
The only remaining release is about the posterior cruciate ligament (PCL) and the choice of prosthesis cruciate retaining (CR) or posterior stabilized (PS).
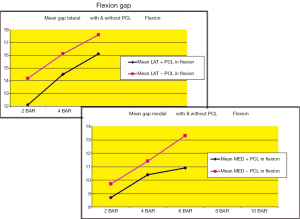
It’s important to know that PCL sacrifice works on the volume and on the symmetry of flexion gap. The PCL resection makes a significant increase on the flexion gap (from 2 to 4 mm) related to the distraction force applied, while it doesn’t affect the extension gap. Moreover, it modifies the flexion gap’s symmetry because with the same tension applied between the tibial cut surface and the posterior condyles, the space opens more on the medial side than on the lateral one as shown in Figure 6. So less rotation must be applied on femoral component to obtain a rectangular gap when PCL is resected.
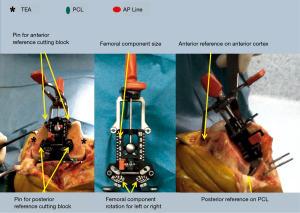
The main purpose is, as in the balanced gap technique, to get a rectangular flexion gap with a correctly tensioned ligamentous apparatus. This purpose is, however, verified with the bone landmarks (TEA and whiteside line). Furthermore, the amount of bone resected from the posterior condyles in particular the medial one is measured, in order not to move the posterior joint line.
The advantages of this combined technique are to reduce malpositioning and increase the reproducibility.
On the contrary, the main limitation is the need of systems with modern design of femoral component with the availability of many sizes. In fact, the principle of adjusting the flexion gap to the extension one needs to be very accurate for a sagittal balance of the knee.
Figure 7 shows the above mentioned technique.
Ligamentous tension evaluation
The amount of force necessary to get a symmetric gap is the critical point of all the techniques providing the femoral rotation and the balancing of the flexion gap by dependent resections.
The correct force for balanced gap is not yet identified. Fiskin and colleagues demonstrate a relationship between the applied force, expressed in Newton, and elongation of the ligaments (expressed in mm as shown in Figure 8). The ligaments visco-elastic properties determine a curve divided in three zones (Figure 9) (15-17).
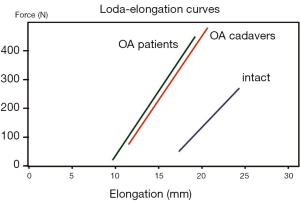
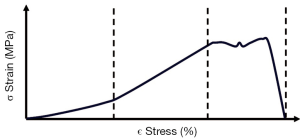
To get a good ligamentous balance the force applied is to remain in the first two zones of the curve as shown in Figure 9, but there aren’t defined values in relation to the patient morphology.
In a previous anatomic study on specimens, the authors (18), with hydraulic balancer, demonstrate the different value of pressure necessary to balanced gap in flexion (65, 6N per condyle) and in extension (98, 4N per condyle).
Furthermore, this technique requires the use of tensors. There are several types of tensors, the main difference between them is that the force can be applied independently to the two joint compartments (medial and lateral) or be applied symmetrically on both condyles.
Technical notes
In all the techniques the resection guide type is crucial: lateral pivoting resection guide maintains a fixed lateral resection. In order to increase the external rotation, an increasing of the medial side resection is necessary.
On the contrary, central pivoting resection guide distributes the variation on both compartments with a lesser resection of the medial side, as you can see in Figure 10.
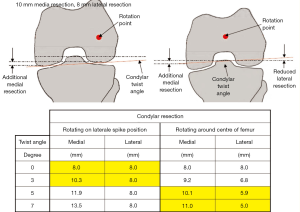
It is strongly recommended to avoid more than 3° of extrarotation with lateral pivot cutting guide because it involves a medial posterior condyle over-resection and consequential instability.
On the contrary central pivot cutting guide allows safe and free rotation without jeopardizing the stability of the joint.
In fact, the type of pivot applied achieves different symmetries and different thickness of bone resection of the posterior condyles and in particularly the medial one.
Advanced ligament based by computer assisted surgery (CAS)
As described above, each reference for the choice of femoral rotation has advantages and disadvantages. However, multiple references are to be used in order to reduce errors.
CAS allows virtual intraoperative planning as shown in Figure 11. That way it is possible to simulate the real size of the gap obtained by bone resections and to calculate, by the use of a calibrated tensors, the distraction force applied.

It even allows to calculate and display the size and the position in rotation of the femoral component for a suitable gap in size and symmetry, as shown in Figure 12.
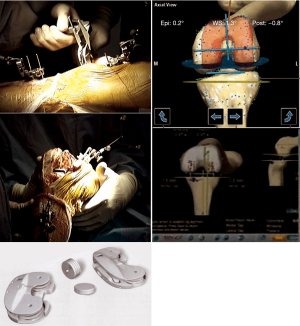
Simultaneously the bone landmark values are shown on the screen: TEA, posterior condyle line and whiteside line.
In our experience the most reliable bone reference is the whiteside line (19).
Beyond a routine clinical use, CAS is a terrific learning tool.
Conclusions
For a correct alignment in rotation of the femoral component there are several bone references (TEA, posterior condyle line and AP line), and techniques of gap balancing and CAS.
None of these showed significantly greater statistically reliability.
It is therefore essential to know different techniques, the instruments and the use at least two references: a reliable bone landmark and soft tissue envelop balancing.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Fehring TK. Rotational malalignment of the femoral component in total knee arthroplasty. Clin Orthop Relat Res 2000.72-9. [PubMed]
- Anouchi YS, Whiteside LA, Kaiser AD, et al. The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res 1993.170-7. [PubMed]
- Olcott CW, Scott RD. The Ranawat Award. Femoral component rotation during total knee arthroplasty. Clin Orthop Relat Res 1999.39-42. [PubMed]
- Laskin RS. Flexion space configuration in total knee arthroplasty. J Arthroplasty 1995;10:657-60. [PubMed]
- Castelli C, Barbieri F, Gotti V, et al. A validated method to assess fluoro-scopically varus-valgus stability in flexion in TKA. 6th Annual meeting of CAOS Proceeding.
- Van Damme G, Defoort K, Ducoulombier Y, et al. What should the surgeon aim for when performing computer-assisted total knee arthroplasty? J Bone Joint Surg Am 2005;87 Suppl 2:52-8. [PubMed]
- Hanada H, Whiteside LA, Steiger J, et al. Bone landmarks are more reliable than tensioned gaps in TKA component alignment. Clin Orthop Relat Res 2007.137-42. [PubMed]
- Matsuda S, Miura H, Nagamine R, et al. Effect of femoral and tibial component position on patellar tracking following total knee arthroplasty: 10-year follow-up of Miller-Galante I knees. Am J Knee Surg 2001;14:152-6. [PubMed]
- Akagi M, Matsusue Y, Mata T, et al. Effect of rotational alignment on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res 1999.155-63. [PubMed]
- Siston RA, Patel JJ, Goodman SB, et al. The variability of femoral rotational alignment in total knee arthroplasty. J Bone Joint Surg Am 2005;87:2276-80. [PubMed]
- Yau WP, Chiu KY, Tang WM. How precise is the determination of rotational alignment of the femoral prosthesis in total knee arthroplasty: an in vivo study. J Arthroplasty 2007;22:1042-8. [PubMed]
- Incavo SJ, Coughlin KM, Pappas C, et al. Anatomic rotational relationships of the proximal tibia, distal femur, and patella: implications for rotational alignment in total knee arthroplasty. J Arthroplasty 2003;18:643-8. [PubMed]
- Jenny JY, Boeri C. Low reproducibility of the intra-operative measurement of the transepicondylar axis during total knee replacement. Acta Orthop Scand 2004;75:74-7. [PubMed]
- Berger RA, Rubash HE, Seel MJ, et al. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 1993.40-7. [PubMed]
- Fishkin Z, Miller D, Ritter C, et al. Changes in human knee ligament stiffness secondary to osteoarthritis. J Orthop Res 2002;20:204-7. [PubMed]
- Sinha RJ, Sheik B, Halbrecht J. Collateral Ligament Strain After Total Knee Arthroplasty. American Academy of Orthopaedic Surgeons- Annual Meeting, Anheim-CA, 1999.
- Kennedy JC, Hawkins RJ, Willis RB, et al. Tension studies of human knee ligaments. Yield point, ultimate failure, and disruption of the cruciate and tibial collateral ligaments. J Bone Joint Surg Am 1976;58:350-5. [PubMed]
- Castelli C, Gotti V, Barbieri F. Effect of PCL release on gaps size and configuration. 6th EFFORT Annual Meeting Helsinki, 2003.
- Castelli C, Barbieri F, Gotti V. Choice of femoral component rotational alignment in tkr-ct less navigation system’s role. 3th Annual Meeting of CAOS, Marbella, 2003.