Mobile bearing and fixed bearing total knee arthroplasty
Introduction
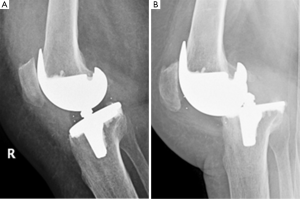
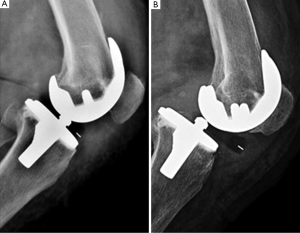
Conventional fixed bearing (FB) total knee arthroplasty (TKA) showed a proven clinical success over time; nevertheless, most of the patients involved in long term survival studies have been elderly individuals with low activity levels (Figure 1). Because of changing demographics in patients requiring TKA, with an increasing proportion of younger patients with higher functional demands, mobile bearing (MB) inserts have been proposed to achieve greater survivorship and clinical outcomes (1) (panel A in Figures 2,3).
MBs were designed to reduce the wear and the consequent loosening of the implant documented in FB devices. Decoupling the complex multidirectional motions which occur in FB designs in unidirectional motion at two bearing interfaces, the MB implants allow a more congruent articular surface increasing the contact area and reducing the contact stresses (2). MB should also address the problem of wear between the Polyethylene (PE) insert and the tibial baseplate. FB implants, in order to grant a suitable locking junction in the tibial component, are necessarily made of titanium alloy and thus, however well finished, unable to provide an ideal smooth surface for PE; MB tibial baseplate are usually made of a highly polished chromium-cobalt alloy instead (3).
In vivo kinematic studies have shown that normal knee permits axial rotation during flexion: the lateral femoral condyle contacts the tibia anterior to the midline in the sagittal plane and with progressive knee flexion there is an average of 14.2 mm of posterior translation (4). Thus the introduction of MB portended an enhancement in range of motion (ROM) and deep knee flexion due to a more physiological sagittal gait kinematics.
At least, a MB offers the potential advantage of self-correcting the rotational mismatch between the tibia and the femur providing an optimization of patello-femoral mechanics and a potential reduction of related complications including anterior knee pain and patellar clunk syndrome.
In contrast, the mobile junction between the tibial baseplate and the insert could be a relevant cause of failure due to PE dislocation, with a reported incidence ranging from 0 to 9.3% (5,6) (panel B in Figures 2,3). Component malposition, extensor mechanism dysfunction, hamstring contracture, extensive postero-lateral release, and increased flexion laxity were contributed to dislocation after TKA (7,8). At least, the cost of a MB TKA is higher, up to 35% more than the corresponding FB device.
The first widely used MB device was the Oxford Unicompartmental Knee (Biomet, Warsaw, IN, USA), introduced in 1976 and still used today, followed by the Low Contact Stress (LCS, formerly New Jersey Knee, DePuy, Warsaw, IN, USA) which was approved by FDA in 1984. While most orthopedic surgeons in USA at the time did not accept the MB concept, there was more enthusiasm for LCS system in Europe, where the first European congress on MB was held in 1988. In 1994, 10 years after the LCS concept introduction, the majority of LCS prostheses were sold in Europe and Asia, compared with only 25% in USA. MB knee designs implants then increased between 1994 and 1998 from 25% to 88% of all TKAs in USA, and from 37% to 72% in Europe and Asia (9). After an increasing trend maintained in the first part of the century, a recent analysis on a database representing approximately a 3% sample in USA, reported a decrease in MB implants from 19% to 7% of primary TKAs between 2005 and 2012 (10).
Over the years, the term “mobile bearing” has been referred to various designs, differing in their mobility: rotating-platform designs allow for free rotation of the PE insert around the central axis of the tibia, meniscal-bearing designs allow unconstrained movement of the insert, and rotating/translating designs allow for gliding in the AP plane and some rotation around the central axis of the tibia (11).
Biomechanical and clinical review
Over the past years, few studies were able to prove some of the theoretical advantages of MB TKAs.
Among these, Tibesku et al. (12) reported a better clinical result (Knee Society Score, KSS) in cruciate-retaining rotating/translating MB TKAs; nevertheless, the results of gait analysis, electromyography and other functional and clinical measures did not show any differences compared to FB TKAs.
In 2015 Tjørnild et al. (13) randomised 46 patients to a mobile or a FB PFC Sigma (DePuy Warsaw, IN, USA) TKA and accomplished a radiostereometric and bone mineral density (BMD) study; they found higher migration for the FB than for the MB tibial plateau, but with equal loss of periprosthetic BMD at the 2-year follow-up time. Overall, the implant migration measured was low and similar to that reported for other well-performing cemented TKAs; functional outcomes (Oxford Knee Score, OKS) were similar in both groups.
The results of a randomized trial comparing FB and MB TKAs in 61 patients at 9-year follow-up was recently published by Poirier et al. (14); they implanted the same prosthesis, Natural-Knee II (Zimmer, Warsaw, IN, USA), that was cementless in all but four cases. There was no significant difference between the two bearing types in terms of ROM, being the ROM at final follow-up identical to the preoperative value. The functional evaluation (KSS and OKS) did not reveal any significant differences between the FB and MB groups. They found a significantly greater risk of osteolysis after 9 years in the FB group, but all the cases of osteolysis occurred in patients with cementless tibial baseplates that had screw holes, which likely caused back-side wear of the PE insert and diffusion of debris along the screws; this difference between the two groups was not clinically meaningful in terms of survival rates.
In 2015 Pais-Brito et al. (15) evaluated 157 consecutive knees which underwent NexGen (Zimmer Warsaw, IN, USA) TKA implantation with patellar resurfacing (82 FB LPS and 75 MB MBK). They found a statistically significant advantage for the MB group at 5-year follow-up in terms of pain on walking, pain on ascending/descending stairs, patello-femoral pain, patients’ ability to walk and to ascend/descend stairs; no difference was detected in patient satisfaction or muscular strength at 5 years. Nevertheless this non randomized study is affected by some relevant patient related bias, as preoperative data reported in the FB group showed statistically significant higher age, higher proportions of female gender, higher degrees of extension lag and lower muscular strength. Furthermore, the study compared a FB posterior stabilized (PS) design with a meniscal bearing posterior cruciate retaining (PCR) design, being PS implants related to patello-femoral complications in several previous studies (16).
Examining the 11-year report of the New Zealand Joint Registry, in 2013 Wyatt et al. (17) found a significantly higher rate of revision for secondary resurfacing of the patella in the FB PS TKA designs compared with either FB PCR or MB designs. They included only TKAs implanted in more than 500 knees, but unfortunately they did not differentiate between PS and PCR implants within the MB group and were not able to know the indication for secondary resurfacing of the patella (pain or instability).
In contrast, several papers in literature rejected the theoretical kinetic and kinematic advantages of the MB design. A summary of the results of previous in vivo kinematic studies about antero-posterior femorotibial contact pattern was reported by Callaghan et al. in 2001 (3). Patient treated with a FB PS TKA exhibited a paradoxical anterior femoral translation during gait. Patients with a meniscal bearing TKA demonstrated a posterior contact position at full extension, a small amount of posterior femoral rollback during the first 60° of flexion, then a paradoxical anterior femoral translation from 60° to 90° of flexion; thus contact pathways in meniscal bearing TKAs proved to be quite similar to FB TKAs. In further analyses, LCS PS rotating-platform TKA showed a continual posterior rollback of the lateral femoral condyle from 0° to 90° of flexion during a deep knee bend, while a paradoxical anterior femoral translation was observed at some point in the range of flexion in 40% of posterior cruciate substituting (PCS) rotating-platform TKA. Both PCR and PS rotating-platform TKA demonstrated axial femorotibial internal rotation with progressive flexion, although less in magnitude than normal knees. However, both PCR and PS rotating-platform TKAs demonstrated minimal variance in contact patterns of medial and lateral femoral condyles during gait; PS rotating-platform TKA showed a normal axial rotational pattern, whereas PCS rotating-platform TKA demonstrated an abnormal reverse rotational pattern. The overall ROM was reduced in weight bearing condition compared to passive non weight bearing condition and the average ROM of rotating-platform and meniscal-bearing TKAs were not superior to FB TKAs.
In 2014 Urwin et al. (18) published the results on gait analysis of fixed and mobile-bearing TKA during walking; sixteen patients were randomized to receive a FB or MB PS Sigma (DePuy Warsaw, IN, USA) TKA. No significant differences were observed between FB and MB in spatiotemporal, kinematic and kinetic results (stride length, gait velocity, stride time, minimum knee flexion angle during walking, sagittal knee ROM and maximum knee adduction moment) at 9 months post-surgery. Comparing FB and MB groups to the controls, important differences were reported following surgery: both TKA groups walked with greater minimum knee flexion and reduced knee adduction moment than the control group.
The femorotibial contact points at 90° of flexion and their relation with anterior knee pain were recently analyzed by van Stralen et al. (19) using the study population of the randomized multi-centre trial of Jacobs et al. (20). They found that the contact point was significantly more anterior in MB than in FB TKAs (59.5% SD 7.8 vs. 66.1% SD 5.3 of the tibial plateau), with the FB group comparable to the healthy non-prosthetic knees. However, this difference in contact points was not correlated with visual analogue scale (VAS) pain, knee function and ROM in KSS.
In 2014 Okamoto et al. (21) studied the weight bearing TKA kinematics in step-up activity; 37 patients (40 knees) were randomized to a MB or a FB Nexgen LPS Flex (Zimmer, Warsaw, IN, USA) TKA, being all the interventions performed by the same surgeon with a measured resection technique and without patellar resurfacing. They found no statistically significant difference between the two groups in post-operative ROM, Hospital for Special Surgery (HSS) score, tibiofemoral angle and component alignment. FB and MB groups demonstrated no major kinematic differences in terms of antero-posterior translation and axial rotation during step-up activity, although a wider range of axial rotation was registered in MB group.
Recently, Artz et al. (22) surveyed FB and MB TKAs regarding kneeling ability, which is considered an important outcome by approximately 50% of patients. Including 206 TKAs, self-reported kneeling ability from OKS at 1 and 2 years after surgery was significantly higher in FB (from 4% preoperative to 28% at 2 years after surgery) versus MB group (from 3% preoperative to 11% at 2 years after surgery), with a significant correlation for Western Ontario and McMaster Universities Arthritis Index (WOMAC) pain and function scores; interestingly, in spite of the difference in reported ability to kneel, ROM and WOMAC score were similar in both groups after surgery.
In a cadaveric study, Heinert et al. (23) compared patellar tracking and patellar kinematics in the natural knee and in mobile and FB PS Sigma (DePuy, Warsaw, IN, USA) TKAs without patellar resurfacing using optical computer navigation. The study reproduced the intraoperative situation where the surgeon assess patellar tracking without muscle tone, with the proximal femur, pelvis, quadriceps attachment and soft tissue envelope intact; furthermore, in vivo quadriceps contraction doesn’t seem to affect patellar congruence angles (24). No significant differences between FB and MB TKAs were found in patellar tilt, patellar rotation, mediolateral position at 0° of flexion and medio-lateral translation relative to the contact point on the patellar groove. Compared to the natural knee, both TKA groups showed a significantly more medial tilt from 50° of flexion, a lack of external rotation with flexion, a tendency of the patella to be slightly more medial relative to its groove in extension and to move laterally with flexion and an early loss of contact with the patellar groove on the femoral component.
In 2014 Snir et al. (16) published a retrospective study on patellar clunk syndrome incidence in fixed (Scorpio NRG, Stryker, Mahwah, NJ, USA) vs. MB (PFC Sigma, DePuy, Warsaw, IN, USA) PS TKAs. They found a significantly higher incidence of clunk syndrome in the MB group compared to the FB group (11.7% vs. 1.8%); there was a significantly higher incidence in males compared to females (8.8% vs. 5.5%), comparably to other recent studies (25), probably due to the higher femoral component average size in males.
Lateral release rates in FB vs. MB TKAs were recently compared by Ferguson et al. (1). A total of 352 patients were randomized to receive a FB or a MB PFC Sigma PS (DePuy, Warsaw, IN, USA) TKA, with a subrandomisation to determine whether the patella would be resurfaced or not; lateral release was performed when tilting or subluxation of the patella was observed through the ROM using a “no thumb” technique. The lateral release rate was equal for the two groups (10%), with a significantly higher incidence in patellar resurfaced group (14% vs. 6%). In the MB group, a statistically significant lower rate of lateral release was found in patients who had patellar resurfacing compared to those who did not; based on this findings, they suggested that the advantages offered by the MB are only realized once the patello-femoral geometry has been optimized by patellar resurfacing.
Even the incidence and the functional effect of partial posterior cruciate ligament (PCL) release in FB and MB PCR TKAs has been analyzed by Schwarzkopf et al. (26); a tight PCL is thought to produce excessive posterior femoral rollback in FB inserts, while is thought to be a potential cause of spin-out or dislocation of a MB insert. They reviewed 1,388 PFC Sigma (DePuy, Warsaw, IN, USA) TKAs (1,014 FB and 374 MB) performed by the same surgeon; percentage of PCL release was decided intra-operatively in order to best balance the flexion gap, beginning with the antero-lateral PCL band and progressing as needed from lateral to medial and from anterior to posterior, then subjectively estimated in percentage. They found a significantly greater proportion of TKAs requiring some degree of PCL release and a significantly greater percentage of the PCL released overall in the MB group, presumably due to the increased sagittal conformity of the insert; however, partial PCL release did not show a clinically significant impact on intra-operative flexion amount or post-operative knee stability at 1 year.
Two international comparative evaluations on aggregated registry data collected by the International Consortium of Orthopaedic Registries, including six national and regional total joint arthroplasty registries were published in 2014. Namba et al. (27), including 319,616 patients who underwent FB (81%) or MB (19%) non PS TKAs between 2001 and 2010, found a significantly higher risk of revision for MB designs with a hazard ratio of 1.43 (P<0.001); similarly, Graves et al. (28), including 137,616 patients who underwent FB (82.4%) or MB (17.6%) PS TKAs between 2001 and 2010, found a significantly higher risk of revision for MB designs with a hazard ratio of 1.86 (P=0.001) in the first year post-surgery.
In recent years, many randomized trials were designed to compare the functional and radiological outcomes of FB and MB TKAs. In 2011 Mahoney et al. (29) published their John Insall Award winning randomized study on short-term functional outcome of MB vs. FB bearing PS TKAs. No statistically significant differences in WOMAC, SF-12 or KSS scores were found up to 2 years post-surgery, although the MB group showed slightly greater average knee flexion at 6 months and 1 year post-surgery. Survival was similar between the two groups using revision of any component both for any reason and for radiolucency or tibial component subsidence as the end point; incidence of complications and non-revision reoperations was similar between the groups.
A randomized controlled trial comparing functional performance in 92 TKAs was published by Jacobs et al. (20), using the PCR Balansys (Mathys, Bettlach, Switzerland) fixed or rotating/translating bearing design without patellar resurfacing. They found no statistically significant difference in active knee flexion and overall functional KSS, with a significant advantage for FB group in stair climbing subscore at 3- and 12-month follow-up.
In a randomized controlled radiostereometric trial, Pijls et al. (30) found no significant differences in overall mean migration or clinical and radiological scores comparing mobile and FB TKAs at 10 to 12 years.
A long-term prospective comparison of FB and MB in patients younger than 51 years of age was published by Kim et al. (31); they evaluated 108 patients in which the FB and MB version of PFC Sigma (DePuy, Warsaw, IN, USA), manufactured by the same company at the same time, were implanted simultaneously by the same surgeon in the same patient. At a mean follow-up of 16.8 years (range, 15-18 years), they found no significant difference in ROM, clinical and functional KSS, survivorship, revision and complication rates.
In 2014 Ferguson et al. (32) published the results of a prospective study including 352 patients which were randomized to undergo a mobile or a FB PS PFC Sigma (DePuy, Warsaw, IN, USA), then subrandomised to have a resurfaced or a retained patella. At 2-year follow-up, they found no statistically significant differences in ROM, SF-12, OKS and KSS between the four subgroups; patients with resurfaced patella in MB TKAs showed marginally greater outcome in KSS and SF-12 scores.
The results of the Knee Arthroplasty Trial commissioned by the Health Technology Assessment programme of the UK NHS were published by Murray et al. (33) in 2014; the study consisted of a multicentre randomized controlled trial with 2,352 participants formally in the trial and 539 in the comparison assessing the MBs. They found no conclusive evidence of any risks or benefits associated with MB in terms of post-operative functional status, quality of life, reoperation and revision rates or cost-effectiveness. There was a 2% incidence of instability or bearing dislocation in the MB group and none in the FB group. Although MB were more expensive for the hospital than FB, these initial costs were partly offset by decreases in the cost of subsequent follow-up; overall, MB increased costs by £85 (95% CI, –£911 to £1081; P=0.87).
In 2015 Fransen et al. (34) performed a prospective randomized controlled clinical trial to evaluate two types of MB inserts and two types of FB inserts of the Genesis II (Smith & Nephew, London, UK) TKA in 146 patients with 5-year follow-up, in order to test the effect of the advancement in insert design (deep dish FB and rotating/translating MB). Knee function (KSS), quality of life (SF-12) and temporal gait parameters did not show any clinically significant differences for both types of bearing and types of insert used. Compared to the MB, the survival of the FB TKAs with respect to revisions for any reasons was better and the number of manipulations was lower, especially when a rotating/translating insert was used.
In a systematic review and meta-regression including 41 studies and over 6,000 TKAs, van der Voort et al. (35) found no significant differences in terms of revision rates, clinical or patient reported outcome (ROM, KSS, OKS, SF-12) and radiological scores between mobile and FB TKAs.
In 2009 Smith et al. (36) published a meta-analysis on clinical and radiological outcomes of FB and MB TKAs including 33 studies and 3,532 knees overall, with a mean follow-up period of 42.2 months. They found no statistically significant differences between MB and FB regarding ROM, quality of life (SF-12, SF-36) and all clinical outcome measures (KSS, HSS, OKS, WOMAC) with the exception of functional KSS, where better results were registered among patients with FB TKAs; moreover, there was no significant difference between the two groups regarding radiological outcome, revision and complication rates.
A meta-analysis comparing FB and MB TKAs, with the latter restricted to rotating platform designs, was carried out by Moskal et al. (11). Including 17 studies with over 1900 knees at a mean 6-year follow-up, they found no differences in clinical scores (KSS, HSS, or SF-12 scores), ROM measures, radiographic evaluations, complication and revision rates. Even if the evaluation of the frontal tibial alignment favored the FB groups, the effect size was small and was not considered clinically important.
In 2014 Bo et al. (7) published a meta-analysis considering only bilateral TKAs using a MB design in one knee and a FB design in the other knee, in order to reduce observer and patient-related bias to the greatest degree; in total, 807 patients and 1,614 knees from 12 studies were included. Results showed that there was no statistical difference between MB and FB in terms of KSS, pain score, ROM, patient satisfaction, complication and reoperation rates and radiolucent lines at different follow-up times (1, 2 to 5, 5 to 8, and more than 8 years).
The first Cochrane review about post-operative functional status in MB versus FB designs for TKA was published by Jacobs et al. (37) in 2004. They found no evidence of superiority for 1 of the 2 prosthesis types with regard to ROM or functional performance of the patients, but the methodological quality of the considered studies was low; in fact only two articles were involved in this review. A newer Cochrane review was published by Hofstede et al. (38) in 2015, regarding only cruciate retaining design, including 19 studies, 1,641 participants (98.5% with osteoarthritis) and 2,247 knees; moderate quality evidence suggests that MB prostheses may have similar effects on knee pain compared with FB prostheses in PCR TKA, considering KSS and VAS. Both Cochrane reviews registered also the same results in clinical and functional scores, health-related quality of life, revision surgery rate, mortality, reoperation rate and other serious adverse events in the two groups, but with low quality evidence.
Conclusions
When MB concept was introduced, the theoretical advantages were represented by the more conforming articular surfaces with lower contact stress and backside wear, the dissipation of the stress wear in two different surfaces and an enhancement of flexion allowing posterior translation, portending knee kinematics closer to physiological gait; moreover, a self-correcting rotational alignment was supposed to enhance the patello-femoral mechanics.
However, clinical studies did not confirm these advantages, as improvement in respect to FB designs in kinematics during step-up activity, kneeling ability, gait function and patello-femoral kinematic were not detected. Moreover, in PCR designs, MB inserts proved a higher need of partial PCL release. The more anterior contact point of MB inserts was proved but with no impact on functional and pain scores, and a lower incidence of lateral release in MB knees was detected just in resurfaced patellas.
No significant advantages in term of functional and radiological outcome, ROM, pain and patient satisfaction were detected by large cohort studies, randomized clinical trials and meta-analyses.
On the other hand, MB inserts showed a relevant complication not reported in FB designs regarding PE dislocation, a higher risk of revision in the first year after surgery, a higher incidence of patellar clunk syndrome in high-flex MB implants and higher costs of the implants.
In conclusion, the theoretical advantages of MB inserts in TKA have not been proven by clinical studies and scientific literature, while a higher rate of complications and higher revision rates were detected. On the basis of the literature review, the routine choice of a MB insert is not currently supported by evidence, as the choice of the implant should be made on the basis of other factors.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ferguson KB, Bailey O, Anthony I, et al. A comparison of lateral release rates in fixed- versus mobile-bearing total knee arthroplasty. J Orthop Traumatol 2015;16:87-90. [Crossref] [PubMed]
- Huang CH, Liau JJ, Cheng CK. Fixed or mobile-bearing total knee arthroplasty. J Orthop Surg Res 2007;2:1. [Crossref] [PubMed]
- Callaghan JJ, Insall JN, Greenwald AS, et al. Mobile-bearing knee replacement: concepts and results. Instr Course Lect 2001;50:431-49. [PubMed]
- Hoff WA, Komistek RD, Dennis DA, et al. Three-dimensional determination of femoral-tibial contact positions under in vivo conditions using fluoroscopy. Clin Biomech (Bristol, Avon) 1998;13:455-472. [Crossref] [PubMed]
- Hasegawa M, Sudo A, Uchida A. Staged bilateral mobile-bearing and fixed-bearing total knee arthroplasty in the same patients: a prospective comparison of a posterior-stabilized prosthesis. Knee Surg Sports Traumatol Arthrosc 2009;17:237-43. [Crossref] [PubMed]
- Thompson NW, Wilson DS, Cran GW, et al. Dislocation of the rotating platform after low contact stress total knee arthroplasty. Clin Orthop Relat Res 2004.207-11. [Crossref] [PubMed]
- Bo ZD, Liao L, Zhao JM, et al. Mobile bearing or fixed bearing? A meta-analysis of outcomes comparing mobile bearing and fixed bearing bilateral total knee replacements. Knee 2014;21:374-81. [Crossref] [PubMed]
- Ridgeway S, Moskal JT. Early instability with mobile-bearing total knee arthroplasty: a series of 25 cases. J Arthroplasty 2004;19:686-93. [Crossref] [PubMed]
- Hamelynck KJ. The history of mobile-bearing total knee replacement systems. Orthopedics 2006;29:S7-12. [PubMed]
- Nguyen LC, Lehil MS, Bozic KJ. Trends in total knee arthroplasty implant utilization. J Arthroplasty 2015;30:739-42. [Crossref] [PubMed]
- Moskal JT, Capps SG. Rotating-platform TKA no different from fixed-bearing TKA regarding survivorship or performance: a meta-analysis. Clin Orthop Relat Res 2014;472:2185-93. [Crossref] [PubMed]
- Tibesku CO, Daniilidis K, Skwara A, et al. Gait analysis and electromyography in fixed- and mobile-bearing total knee replacement: a prospective, comparative study. Knee Surg Sports Traumatol Arthrosc 2011;19:2052-9. [Crossref] [PubMed]
- Tjørnild M, Søballe K, Hansen PM, et al. Mobile- vs. fixed-bearing total knee replacement. Acta Orthop 2015;86:208-14. [Crossref] [PubMed]
- Poirier N, Graf P, Dubrana F. Mobile-bearing versus fixed-bearing total knee implants. Results of a series of 100 randomised cases after 9 years follow-up. Orthop Traumatol Surg Res 2015;101:S187-92. [Crossref] [PubMed]
- Pais-Brito JL, Rafols-Urquiza B, Gonzalez-Massieu L, et al. Reduced patellofemoral and walking pain with mobile-bearing vs. fixed-bearing total knee replacements: a mid-term prospective analytic study. Acta Orthop Traumatol Turc 2015;49:375-81. [PubMed]
- Snir N, Schwarzkopf R, Diskin B, et al. Incidence of patellar clunk syndrome in fixed versus high-flex mobile bearing posterior-stabilized total knee arthroplasty. J Arthroplasty 2014;29:2021-4. [Crossref] [PubMed]
- Wyatt MC, Frampton C, Horne JG, et al. Mobile- versus fixed-bearing modern total knee replacements- which is the more patella-friendly design?: The 11-year New Zealand Joint Registry study. Bone Joint Res 2013;2:129-31. [Crossref] [PubMed]
- Urwin SG, Kader DF, Caplan N, et al. Gait analysis of fixed bearing and mobile bearing total knee prostheses during walking: do mobile bearings offer functional advantages? Knee 2014;21:391-5. [Crossref] [PubMed]
- van Stralen RA, Heesterbeek PJ, Wymenga AB. Different femorotibial contact points between fixed- and mobile-bearing TKAs do not show clinical impact. Knee Surg Sports Traumatol Arthrosc 2015;23:3368-74. [Crossref] [PubMed]
- Jacobs WC, Christen B, Wymenga AB, et al. Functional performance of mobile versus fixed bearing total knee prostheses: a randomised controlled trial. Knee Surg Sports Traumatol Arthrosc 2012;20:1450-5. [Crossref] [PubMed]
- Okamoto N, Nakamura E, Nishioka H, et al. In vivo kinematic comparison between mobile-bearing and fixed-bearing total knee arthroplasty during step-up activity. J Arthroplasty 2014;29:2393-6. [Crossref] [PubMed]
- Artz NJ, Hassaballa MA, Robinson JR, et al. Patient Reported Kneeling Ability in Fixed and Mobile Bearing Knee Arthroplasty. J Arthroplasty 2015;30:2159-63. [Crossref] [PubMed]
- Heinert G, Kendoff D, Preiss S, et al. Patellofemoral kinematics in mobile-bearing and fixed-bearing posterior stabilised total knee replacements: a cadaveric study. Knee Surg Sports Traumatol Arthrosc 2011;19:967-72. [Crossref] [PubMed]
- Masri BA, McCormack RG. The effect of knee flexion and quadriceps contraction on the axial view of the patella. Clin J Sport Med 1995;5:9-17. [Crossref] [PubMed]
- Agarwala SR, Mohrir GS, Patel AG. Patellar clunk syndrome in a current high flexion total knee design. J Arthroplasty 2013;28:1846-50. [Crossref] [PubMed]
- Schwarzkopf R, Woolwine S, Josephs L, et al. The Incidence and Short Term Functional Effect of Partial PCL Release in Fixed and Mobile Bearing PCL Retaining TKA. J Arthroplasty 2015;30:2133-6. [Crossref] [PubMed]
- Namba R, Graves S, Robertsson O, et al. International comparative evaluation of knee replacement with fixed or mobile non-posterior-stabilized implants. J Bone Joint Surg Am 2014;96 Suppl 1:52-8. [Crossref] [PubMed]
- Graves S, Sedrakyan A, Baste V, et al. International comparative evaluation of knee replacement with fixed or mobile-bearing posterior-stabilized prostheses. J Bone Joint Surg Am 2014;96 Suppl 1:59-64. [Crossref] [PubMed]
- Mahoney OM, Kinsey TL, D'Errico TJ, et al. The John Insall Award: no functional advantage of a mobile bearing posterior stabilized TKA. Clin Orthop Relat Res 2012;470:33-44. [Crossref] [PubMed]
- Pijls BG, Valstar ER, Kaptein BL, et al. Differences in long-term fixation between mobile-bearing and fixed-bearing knee prostheses at ten to 12 years' follow-up: a single-blinded randomised controlled radiostereometric trial. J Bone Joint Surg Br 2012;94:1366-71. [Crossref] [PubMed]
- Kim YH, Kim JS, Choe JW, et al. Long-term comparison of fixed-bearing and mobile-bearing total knee replacements in patients younger than fifty-one years of age with osteoarthritis. J Bone Joint Surg Am 2012;94:866-73. [Crossref] [PubMed]
- Ferguson KB, Bailey O, Anthony I, et al. A prospective randomised study comparing rotating platform and fixed bearing total knee arthroplasty in a cruciate substituting design--outcomes at two year follow-up. Knee 2014;21:151-5. [Crossref] [PubMed]
- Murray DW, MacLennan GS, Breeman S, et al. A randomised controlled trial of the clinical effectiveness and cost-effectiveness of different knee prostheses: the Knee Arthroplasty Trial (KAT). Health Technol Assess 2014;18:1-235. vii-viii. [Crossref] [PubMed]
- Fransen B, Hoozemans MJ, Keijser LC, et al. Does insert type affect clinical and functional outcome in total knee arthroplasty? A randomised controlled clinical trial with 5-year follow-up. J Arthroplasty 2015;30:1931-7. [Crossref] [PubMed]
- van der Voort P, Pijls BG, Nouta KA, et al. A systematic review and meta-regression of mobile-bearing versus fixed-bearing total knee replacement in 41 studies. Bone Joint J 2013;95-B:1209-16. [Crossref] [PubMed]
- Smith TO, Ejtehadi F, Nichols R, et al. Clinical and radiological outcomes of fixed- versus mobile-bearing total knee replacement: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 2010;18:325-40. [Crossref] [PubMed]
- Jacobs W, Anderson P, Limbeek J, et al. Mobile bearing vs fixed bearing prostheses for total knee arthroplasty for post-operative functional status in patients with osteoarthritis and rheumatoid arthritis. Cochrane Database Syst Rev 2004.CD003130. [PubMed]
- Hofstede SN, Nouta KA, Jacobs W, et al. Mobile bearing vs fixed bearing prostheses for posterior cruciate retaining total knee arthroplasty for postoperative functional status in patients with osteoarthritis and rheumatoid arthritis. Cochrane Database Syst Rev 2015;2:CD003130. [PubMed]



