Seven times replacement of permanent cardiac pacemaker in 33 years to maintain adequate heart rate: a case report
Introduction
Pacemaker implantation is a technically challenging but a valuable and widely used technique in cardiac arrhythmic patients worldwide; implicated globally as a treatment of choice for various cardiac manifestations. Use of permanent pacemakers (PPMs) is increasing with an aging population, rising medical comorbidities and expanding cardiac indications, which demands the use of such devices. Worldwide, there are more than 3 million functioning PPMs and about 600,000 pacemakers are implanted each year (1,2). On an average, 70–80% of all PPMs are implanted in patients 65 years of age or older. As per a latest research, PPM demand will show a continuous rising trend in future in developed economy (3-5).
Over the years, pacemaker technology has progressed from fixed-rate single-chamber pacemakers to dual-chamber pacemakers with pacing algorithms for improved rate response and minimized ventricular pacing (5). Technically, the entire pacemaker unit (pulse generator and a lead system) is driven by a power supply (battery) to deliver electrical pulse with the proper intensity to the proper location for desired heart rate. It is indeed very important that batteries have high levels of safety, reliability and longevity to avoid frequent replacements and effective functioning. Despite the technical advancements in pacemakers, complications are still reported and concerns have been raised about the long-term efficacy, safety and integrity of the device. These complications may be associated with the malfunctioning of the pacemaker itself, related and unrelated to the location type or the ones occurring during the implantation procedure such as bleeding, infection, or collapsed lung Nonetheless, periodic check and follow-ups are often advised to patients for assuring proper functioning of pacemakers with a certainty in reduction of complications (1,3,6,7).
Having documented pacemaker implantation as a widely used technique now-a-days, this clinical presentation with a longest period of follow-up to our knowledge for PPM implantation would be of prime interest to cardiac physicians as it demonstrates a complete era from single-chamber pacemakers to dual-chamber pacemaker in a patient. Here, we share our longest clinical experience with an 85-year-old man who underwent 7 times replacement of cardiac pacemaker over the tenure of 33 years to maintain adequate heart rate.
Case presentation
An 85-year-old male from China suffering from dizziness and syncope was admitted to our hospital (People’s Hospital of Yuxi City, China). Initial diagnosis revealed third-degree atrioventricular (AV) block with a heart rate of 35–40 beats per minute (bpm) along with Aase’s syndrome and primary hypertension. Unfortunately, pharmacological treatment alone was not sufficient to control all the symptoms. Considering the degradation of patient’s condition, we decided for pacemaker implantation immediately. A single incision on the right upper chest was made to isolate cephalic veins following which a single-chamber pacemaker (VVI) was implanted. Symptomatic relief was noted after VVI implantation. Electrocardiogram (ECG) and regular follow-up was then continued and ventricular pacing was observed after a long period of follow-up.
Five years post-surgery, VVI was replaced through the same position because of battery exhaustion, while the primary electrode catheter was kept in use. Three years later, the patient presented with a complaint of dizziness again and re-examination, revealed VVI battery debilitation due to premature battery exhaustion. We then decided to implant a Medronic single-chamber pacemaker via the same position of right upper chest. The primary electrode catheter was detected under normal threshold and was retained.
Seven years later, pacemaker was again replaced for the fourth time due to battery depletion. However, threshold of the primary electrode catheter was recorded to be as high as 2.6 V. This time, we decided to implant Medronic 8081 through left subclavian venipuncture.
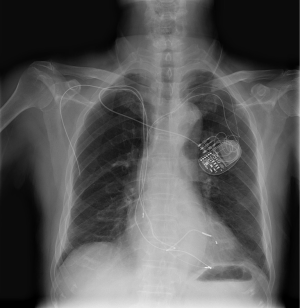
After 3 years, patient was readmitted to our hospital with complaints of frequent cardiopalmus, distress, and edema of both the lower limbs. We carefully assessed pacemaker and found it to be favorably stable. Diagnostic tests revealed patient suffering from coronary artery disease (CAD), third-degree AV block, cardiac dysfunction with New York Heart Association Functional Classification (NYHA) class III heart failure and primary hypertension. No significant improvement was observed in patient’s condition with repeated drug therapy. However, after adjusting the frequency of stimulation of the pacemaker to 70 bpm, patient had a symptomatic relief. Further, after 2 years, battery was discharged again. Considering the severity of patient’s disease and knowing that cardiac dysfunction was reported previously, a tri-chamber pacemaker was chosen to take place of previous single-chamber pacemaker. The original electrode catheter was placed in right ventricular through left subclavian vein, and other electrode catheters were implanted in right atrium and left ventricular via left subclavian vein. However, difficulty was observed while inserting the catheter to coronary sinus; as a result, the procedure was unsuccessful and we ended up implanting Medronic 7966i dual chamber pacemaker (Medtronic, Minneapolis, USA) instead (Figure 1). Post-surgical assessment demonstrated significant improvement in cardiac function without any complications.
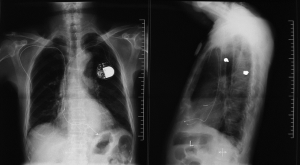
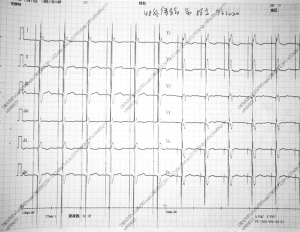
Almost after 6 years, pacemaker was out of battery and was changed for the sixth time to Medronic Kappa KDR701 dual chamber pacemaker; however, original catheter was retained. Patient was routinely followed up for next 4 years and pacemaker functioning was reported to be normal. Post-4 years, the patient again suffered from frequent cardiopalmus, distress, and edema of both lower limbs and dyspnea under regular treatment of heart failure (Figure 2). We then decided to update dual chamber pacemaker to triple chamber pacemaker considering his medical history. Fortunately enough, this time implantation of the wire guide through left subclavian vein puncture was successful; however, we felt obstruction while placing catheter into left superior vena cava due to its narrowness as indicated by digital subtraction angiography (DSA). Following this, we re-punctured through right subclavian vein and successfully implanted electron catheter of left ventricular to posterior branch of the left ventricle of coronary sinus ensuring that all parameters fulfill standard requirements. We connected the catheter to left upper chest through subcutaneous tunnel, and replaced Medronic 8042 tri-pacemaker at the original position. ECG indicated significant narrowing of ventricular complex (Figure 3). Pacemaker was found to be stable with normal pacemaker and cognitive functions; moreover, cardiac function improved after pacemaker replacement.
Recently, the patient underwent seventh time pacemaker replacement. Under the protection of temporary pacemaker through femoral vein, an incision of about 2 cm was made under left clavicle after administration of 1% lidocaine injection. A blunt dissection to deep and superficial fasci was made and primary pacemaker was dissected. Parameter settings of right ventricular were demonstrated as follows: the threshold of ventricular pacing was 0.4 V; impedance 440 Ω whereas the parameter settings of left ventricular were satisfactory with threshold of 0.9 V and impedance 580 Ω. Primary electrode was connected to new pacemaker, sac was implanted and finally incision was sutured. After successful replacement of pacemaker, patient was discharged from hospital without any apparent symptoms. A long following up till now demonstrated no major complications with normal functioning of all parameters indicating a good result and complete resolution.
Discussion
Ever since the first success in PPM implantation was achieved in 1958, it has been a pervasive technique used in hospitals and gradually becomes an important method and mainstay treatment for effective management of cardiovascular diseases (8). Moreover, use of PPM is showing an increasing trend in the past few decades. Surgery success rate and disease cure rates have been improved to a great extent due to technical advancements in pacemakers. Indication of pacemaker has expanded to other type of arrhythmia and heart failure as well (9). Even though being such an important technique, various complications are associated with the use of PPM owing to active lifestyle, possibility of traumatic events, and localized or systemic infections that may affect the pacing system. Despite recent technical advancements, battery exhaustion remains the ‘weakest link’ of the permanent pacing system. Concerns have been raised for the long term reliability and integrity of the battery system. Various studies indicated that the primary reason for pacemaker replacement is battery exhaustion, which revealed a decent rate of abnormal replacement (10-13). Moreover, faulty program control functions also contributed to frequent pacemaker replacements (14). Here, in our case report, the patient with PPM for a period of 33 years underwent 7 times replacements of pacemaker. During the entire duration, pacemaker was updated from single chamber to dual chamber, and at last upgraded to tri-chamber pacemaker indicated that pace maker from right ventricular may induce the occurrence and development of heart failure. Additionally, it was also found out by Chow et al. that right ventricular pacing either has no hemodynamic benefit or had detrimental effects on left ventricular function. This probably attributes that right ventricular apical pacing (which creates a left bundle branch block pattern) causes ventricular dyssynchrony with detrimental effects on overall cardiac pump function or heart’s natural pacemaker. For third-degree AV block, long time use of dual chamber pacemaker may induce and exacerbate heart failure. Cardiac resynchronization therapy or biventricular pacing increases the systolic synchronicity of both the ventriculars; therefore, it is effective for treatment of heart failure caused by pacemaker. Both the multisite stimulation in cardiomyopathies (MUSTIC) and the multicenter insync randomized clinical evaluation (MIRACLE) studies were randomized crossover trial of biventricular pacing which demonstrated significant improvements in quality of life scores, exercise tolerance, NYHA class, peak oxygen uptake, and cardiac ejection fraction during biventricular pacing (15). In our case, long term following up and upgrading the replacement pacemaker proved that biventricular pacing is superior to traditional right ventricular pacing in patients with AV block. These findings were in accordance with Curtis who conducted a randomized study in 918 patients and concluded that conventional right ventricular pacing in patients with AV block and left ventricular systolic dysfunction with NYHA class I, II, or III heart failure is inferior to biventricular pacing. Although the potential dysfunction rate of pacemaker is 1%, several studies showed the infection prevalence is much higher in later replacement as compared to primary pacemaker implantation (14,15). It is now a widely known fact that infection is a ruinous complication of PPM with varying rates from 0.13% to 19.9% (13,15). Therefore, the prevailing opinion is to conduct the operation in optimal conditions maintaining sterility to prevent infection keeping in view patients baseline characteristics, low BMI, hypoimmunity and age (9,10,15). In our case, we accomplished the replacement of pacemaker at same position multiple times with due vigilance and care in spite of having a possibility of phlebostenosis and venous embolism. Finally, the patient reported ease without any symptoms till date. We further suggest that PPM implantation should be accompanied by routine follow up to avoid complications and assuring proper functioning of pacemakers. To the best of our knowledge, this is the only case-report with such a long follow up and highest number of pacemaker replacements.
Conclusions
We successfully performed overall seven pacemaker implantations and upgradation in an 85-year-old patient diagnosed with third-degree AV block for 33 years. The patient is now healthy with normal heart rate and without any symptoms of dizziness and syncope. Hopefully, this interesting case may serve as a miniature of the development of pacemaker operation for cardiac physicians.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Consents: The study was approved by the ethics committee of People’s Hospital of Yuxi City, Yuxing Rd Hongta, Yuxi, Yunnan, China, and case report form were approved by ethics committees, and written informed consent was obtained from the patient for publication of this case report and accompanying images. The study methods were conducted in accordance with approved national and international guidelines.
References
- Mallela VS, Ilankumaran V, Rao NS. Trends in cardiac pacemaker batteries. Indian Pacing Electrophysiol J 2004;4:201-12. [PubMed]
- Elahi MM, Lee D, Dhannapuneni RR. Predictors of permanent pacemaker implantation during the early postoperative period after valve surgery. Tex Heart Inst J 2006;33:455-7. [PubMed]
- Wood MA, Ellenbogen KA. Cardiology patient pages. Cardiac pacemakers from the patient’s perspective. Circulation 2002;105:2136-8. [PubMed]
- Bradshaw PJ, Stobie P, Knuiman MW, et al. Trends in the incidence and prevalence of cardiac pacemaker insertions in an ageing population. Open Heart 2014;1:e000177. [PubMed]
- Greenspon AJ, Patel JD, Lau E, et al. Trends in permanent pacemaker implantation in the United States from 1993 to 2009: increasing complexity of patients and procedures. J Am Coll Cardiol 2012;60:1540-5. [PubMed]
- Gul EE, Kayrak M. Common Pacemaker Problems: Lead and Pocket Complications, Modern Pacemakers - Present and Future. Available online: , accessed August 5, 2015.http://www.intechopen.com/books/modern-pacemakers-present-and-future/commonpacemaker-problems-lead-and-pocket-complications
- Schiariti M, Cacciola M, Puddu PE. Complications of Pacemaker Implantation, Modern Pacemakers - Present and Future. Available online: , accessed August 10, 2015.http://www.intechopen.com/books/modern-pacemakers-present-andfuture/complications-of-pacemaker-implantation
- Furman S, Schwedel JB. An intracardiac pacemaker for Stokes-Adams seizures. N Engl J Med 1959;261:943-8. [PubMed]
- Keping Chen, Zhang P. Clinical analysis of 2553 cases of pacemaker implantation. Chinese Circulation Journal 2001;16:12-4. In Chinese.
- Davies JG, Siddons H. Experience with implanted pacemakers: technical considerations. Thorax 1965;20:128-34. [PubMed]
- Liu XL, Ren LH, Ye HM. Reasons and complications of pacemaker replacement operation: clinical analysis of 69 case-times. Zhonghua Yi Xue Za Zhi 2008;88:1989-91. [PubMed]
- Maisel WH. Pacemaker and ICD generator reliability: meta-analysis of device registries. JAMA 2006;295:1929-34. [PubMed]
- Sowton E, Hendrix G, Roy P. Ten-year survey of treatment with implanted cardiac pacemaker. Br Med J 1974;3:155-60. [PubMed]
- Zhan J, Chen K, Hua W. Analysis of causes of pacemaker replacement for 1023 cases. Chinese Circulation Journal 2009;24:360-63. In Chinese.
- Abraham WT, Fisher WG, Smith AL, et al. Cardiac resynchronization in chronic heart failure. N Engl J Med 2002;346:1845-53. [PubMed]