Cadaveric validation of porcine model suggests noninvasive positive pressure ventilation may be safe following esophagectomy
Introduction
Respiratory complications occur in about 40% of patients following esophagectomy (1). Noninvasive positive pressure ventilation (NPPV) has been shown to reduce complications, mortality, and cost when compared to endotracheal intubation (ET). However, clinicians have been hesitant to use NPPV following esophagectomy due to the hypothetical risk of barotrauma to the anastomosis. In our previous study, we used an ex vivo and in vivo porcine model to quantify the pressure tolerance of an esophageal anastomosis and the pressure received in the esophagus during NPPV (2). We found that a porcine esophageal anastomosis tolerates manifold higher pressures than are delivered to the esophagus during NPPV, suggesting that NPPV may be a safe alternative to ET after esophagectomy. The validity of our porcine model in human beings remains an open question. In this study, we created a substitute model for a clinical trial by quantifying the pressure threshold of cadaveric esophageal anastomoses, and comparing it to our porcine data. This is the critical final step before a trial of NPPV in patients undergoing esophagectomy.
Methods
Sample acquisition
Consent was waived by our Institutional Review Board. Ten human cadaveric esophageal specimens were obtained from autopsied patients at our institution. Esophageal specimens were only obtained from patients whose esophagus was not suspected to contain pathology and consequently was not dissected during autopsy. The entire length of the esophagus from the proximal pharynx to the gastroesophageal junction was harvested by the forensic pathologist. The stomach was not available for harvest as the autopsy protocol in our institution requires complete gastric removal and dissection. Upon receipt of the specimen, the esophagus was frozen at −20 °C until experimentation, following the protocol observed in our last study (2).
Measurement of pressure threshold of cadaveric esophageal anastomosis
Since no gastric specimens were obtained, we performed esophagoesophageal anastomoses in all our cadaveric specimens following a protocol identical to that published in our previous work (2). Briefly, we transected a segment of cadaveric esophagus and used a linear cutter (DST GIATM 80 mm; Covidien) to perform a side-to-side, functional end-to-end anastomosis of both esophageal segments. With intraluminal pressure monitoring, we insufflated the anastomosis with air until an anastomotic leak was observed, and measured the pressure threshold of the anastomosis. A leak was identified by failure of the anastomosis to maintain pressure and by excursion of air bubbles from the anastomosis when immersed in a water bath. All experiments were performed by the same author as in the previous study to minimize inter-operator variability.
Measurement of pressure threshold of porcine gastroesophageal and esophagoesophageal anastomoses
Next, we investigated if there is a difference in pressure tolerance between gastroesophageal and esophagoesophageal anastomoses using our previously established ex vivo porcine model. Following the above protocol, we performed 10 gastroesophageal and 10 esophagoesophageal anastomoses in porcine tissue, insufflated the anastomoses until a leak was observed, and measured the maximum tolerated pressure. To minimize variables, the same author performed all experiments, alternating gastroesophageal and esophagoesophageal anastomoses in a single sitting.
Statistical analysis
All data is reported as a mean with 95% confidence interval and error bars representing the standard error of the mean (S.E.M.). The Student’s t Test was used to compare continuous data. Statistical analysis was performed with GraphPad Prism version 6.00 (GraphPad Software, La Jolla, California, USA).
Results
Characteristics of patients
The interval between death and autopsy, age, sex, and cause of death of each patient whose esophagus was used are detailed in Table 1. No gross esophageal pathology was noted in any specimen.
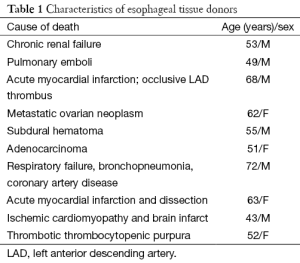
Full table
Pressure threshold of cadaveric anastomoses
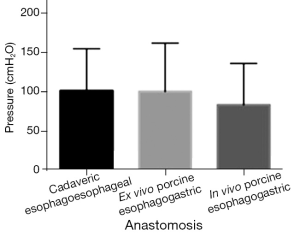
Ex vivo cadaveric esophagoesophageal anastomoses tolerated 101±39 cmH2O (range, 63-140 cmH2O) before an anastomotic leak was observed (Figure 1). The recorded maximum tolerated pressure ranged from 59 to 246 cmH2O (median 86 cmH2O). Leaks only occurred at the staple line and not in other parts of the tissue. There was no significant difference in pressure tolerance between cadaveric and previously reported ex vivo (P=0.98) and in vivo (P=0.46) porcine esophagogastric anastomoses (Figure 1).
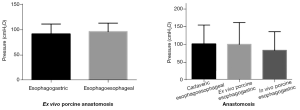
Pressure threshold of porcine gastroesophageal vs. esophagoesophageal anastomoses
Ex vivo porcine gastroesophageal anastomoses tolerated 92±14 cmH2O (range, 78-106 cmH2O) before anastomotic leak (Figure S1). Esophagoesophageal anastomoses tolerated 96±12 cmH2O (range, 85-102 cmH2O) before leak was observed. There was no significant difference (P=0.42) between porcine gastroesophageal and esophagoesophageal anastomoses.
Discussion
In this study, we found that cadaveric esophageal anastomoses tolerate significant pressure before leak, which corroborates the findings in our recent porcine model (2). In our previous study, we found that the proximal porcine esophagus senses 5 to 15 cmH2O when 20 to 40 cmH2O of pressure via a laryngeal mask airway (LMA) were applied (2). Therefore, an esophageal anastomosis can tolerate a much greater pressure than is delivered to the esophagus by NPPV, suggesting that NPPV may pose a minimal threat to an esophageal anastomosis and may be safe following esophagectomy.
Our study has several limitations. The most important limitation in this study was the use of esophagoesophageal rather than esophagogastric anastomoses that are most common clinically. Unfortunately, the stomach is always dissected in autopsy and consequently unavailable for our study. We did demonstrate, however, that the pressure tolerance of esophagoesophageal and esophagogastric anastomoses is similar in porcine specimens, which suggests that the same may be true in human cadaveric tissue (Figure S1). Two, we used cadaveric rather than live human tissue. Live tissue would not suffer necrotic changes and would be expected to have a higher pressure tolerance, so our study likely erred on the side of caution. Additionally, we found no difference in pressure thresholds between ex vivo and in vivo esophageal anastomoses in pigs in our previous study, suggesting that cadaveric tissue might have a similar pressure tolerance to that of live human tissue as well. Three, our model only tests the pressure tolerance in the immediate post-operative setting. As inflammation peaks several days post-operatively, the pressure threshold of an anastomosis may change. Four, we discovered in our previous work that NPPV results in significant gastric distension, which may compromise flow and perfusion to the conduit (2). Our cadaveric model was not designed to evaluate this potential risk, which needs further investigation.
Conclusions
We created a cadaveric model as a proxy for a live, human trial and established the pressure threshold of an esophageal anastomosis. Along with our previous work, we suggest that an esophageal anastomosis can tolerate a significantly higher pressure than is sensed by the esophagus during NPPV. NPPV is likely safe following esophagectomy. This is the important final step before a trial of NPPV in patients undergoing esophagectomy.
Acknowledgements
This study was funded by a Dartmouth SYNERGY grant. We are grateful to Susan Kane, C.V.T., for technical assistance.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ferguson MK, Celauro AD, Prachand V. Prediction of major pulmonary complications after esophagectomy. Ann Thorac Surg 2011;91:1494-500. [PubMed]
- Raman V, MacGlaflin CE, Erkmen CP. Noninvasive positive pressure ventilation following esophagectomy: safety demonstrated in a pig model. Chest 2015;147:356-61. [PubMed]