Rotational alignment of the tibial component in total knee arthroplasty
Introduction
Many studies related a total knee arthroplasty (TKA) poor functional outcome to rotational malalignment of the femoral and tibial components (1-3). The goal of tibial component rotational alignment in primary TKA is to achieve, on the coronal plane, parallelism between the femoral transepicondylar axis (TEA) and the medio-lateral (ML) axis of the tibial component, avoiding errors in internal or external rotation between the two axes. Unfortunately, this ideal coronal parallelism is hard to be achieved during range of motion (ROM) because the TEA (surgical and/or anatomical) has been demonstrated to be cylindrical (4) and the tibial plateau undergoes a substantial internal rotation when patients perform regular activities of daily living (ADLs) (5).
Early implant failures, when related to tibial rotational malalignment, are mainly characterized by extensor mechanism complications (6-8) and severe knee stiffness (9). A standard tibial rotational reference is still controversial in the current literature. Few anatomical landmarks have been proposed in order to obtain an accurate rotational position of the tibial component, including the medial third of the tibial plateau (10), the “Akagi” line (11), the central third of the tibial tubercle (12) and the postero-lateral tibial corner (13).
Several surgical techniques, following the use of these landmarks, have been described to rotationally orient the tibial component in TKA, including the “self range-of-motion” (1,7) and the “maximizing tibial coverage” (14) techniques. The “self range-of-motion” technique aligns the tibial component according to the rotational alignment of the femoral component during trial reduction with a “self-seeking method”. Because several recent morphological assessments concluded that contemporary tibial designs do not match global population morphology (15,16), the industry shifted its interest to achieve high coverage in many newer tibial designs, proponing asymmetric and even markedly anatomical designs. However, focusing solely on maximizing tibial coverage may lead to severe internal rotation errors (17).
In previous studies (18,19), the authors of the current study proposed and validated a new surgical technique for positioning of the tibial component in TKA: we intended to ascertain if there was a more adequate way of orienting tibial components in TKA, starting from the fact that matching of orientation of two similar curves (the anterior tibial contour after osteotomy and the anterior curvature of the tibial baseplate) would be an easier definable landmark than a single anatomical point or a line (“Curve-on-Curve Technique”).
This article reviews the author’s previous experience (from the proposal of a new anatomical rotational landmark to its “in vivo” validation in a consecutive series of TKA) comparing, in the discussion section of the current review, their studies with the current literature on different surgical techniques already proposed for a correct rotational alignment of the tibial component in primary TKA. In the first study, we will demonstrate that the anterior tibial surface contour is a reliable landmark for correct tibial component rotational positioning respect to the “Akagi” line and the medial third of the tibial tubercle. In the second study, we will test the reliability of this anatomical landmark and adapted surgical technique (“Curve-on-Curve Technique”) in an “in vivo” study using two different tibial baseplate designs: the first one symmetric and the second one strongly anatomical (right/left options).
First study
We analyzed 124 MRI knee scans from 124 patients (69 women and 55 men) with a mean age of 42 years (18 to 74 years): those radiological studies were originally performed to rule out possible ligamentous or cartilaginous lesion. Before MRI evaluation, the authors confirmed that none of the knees revealed the presence of moderate to severe osteoarthritis, ligamentous lesions, significant meniscal lesions, or flexion contracture. The MRI protocol included positioning the knee in full extension with the second metatarsal axis in a vertical position: all images were 2 mm in thickness and with 3 mm in reconstructive increments from the distal metaphysis to the tibial tubercle.
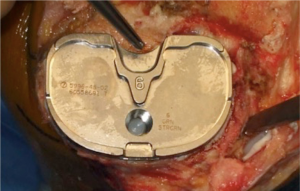
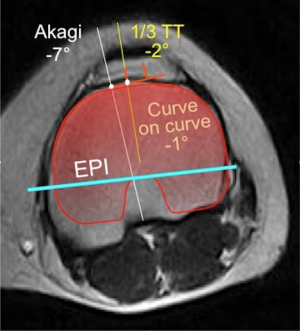
After selecting a single best axial scan, the femoral surgical transepicondylar axis (sTEA), the femoral posterior condylar axis (PCA) and the projection of the medial third of the tibial tubercle on the anterior tibial cortex were identified. For each knee, the sTEA, the PCA and the medial third of the tibial tubercle were projected on a tibial axial cut. The geometric center of the tibial area was also identified. A line was first drawn from the center of the tibial plate to the medial third of the tubercle and then the perpendicular line to the TEA passing through the tibial plate center was identified. At this point, the Akagi’s line was drawn. This landmark was made by a line starting at the medial third of the tibial tubercle and ending at the center of the posterior cruciate ligament tibial insertion. The most appropriate tibial baseplate tracing (size 3 to 8) for the Nex-Gen Total Knee System (Zimmer, Warsaw, USA) was superimposed at this time, matching the anterior tibial cortex with its anterior surface (“Curve-on-Curve Technique”). The rotation of the tibial plate tracing was calculated with respect to the sTEA, the medial third of the tibial tubercle line, the Akagi’s line and the PCA (Figure 1).
All axial images were evaluated independently by three observers (PFI, PCM, AB) utilizing a custom-made digital software. They independently repeated the entire process, from point gathering to angles measurement. The reliability of each measurement was then calculated using Bland-Altman analysis for interobserver agreement: the coefficient value has been reported as an average of multiple pairwise comparisons (PFI vs. PCM; PFI vs. AB, PCM vs. AB).
Results
Akagi’s line
The three observers showed an agreement on the localization of the Akagi’s line in 64% of the cases within 3° and in 85% of the cases within 5° (minimum, −16°; maximum, −7°). The average intraclass correlation coefficient was 0.923 (PFI vs. PCM: 0.910; PFI vs. AB: 0.933; PCM vs. AB; 0.927). The observers agreed on the statistically significant evidence that the use of this surgical landmark might lead to internal rotation of the tibial component.
Medial third of the tibial tubercle
The three observers showed an agreement on the localization of the medial third of the tibial tubercle in 29% of the cases within 3° and in 70% of the cases within 5° (minimum, −4°; maximum, +4°). The average intraclass correlation coefficient was 0.881 (PFI vs. PCM: 0.871; PFI vs. AB: 0.897; PCM vs. AB: 0.876). The use of this surgical landmark leaded to an average external rotation of the tibial component of 4.7° (±3.6º) respect to the TEA.
Anterior tibial surface curvature
The three observers showed an agreement on the localization of the anterior tibial surface contour in 89% of the cases within 3° and in 99% of the cases within 5° (minimum, −1°, maximum, +4°). The average intraclass correlation coefficient was 0.949 (PFI vs. PCM: 0.940; PFI vs. AB: 0.961; PCM vs. AB: 0.947). The final observation was that, aligning the tibial baseplate according to the anterior tibial contour guaranteed full matching ±3° with respect to the epicondylar axis in 75% of the cases with minor errors in external rotation.
Second study
The authors selected, after obtaining Institution Review Board (IRB) and patient’s consent, 80 consecutive patients affected by primary degenerative knee joint disease. All patients were originally scheduled for primary TKA. Preoperative diagnosis in this series was always osteoarthritis without previous history of trauma, previous surgery or major knee dysplasia. Patients’ mean age at surgery was 72 years (range, 60-81 years).
Total knee arthroplasty (TKA) component designs
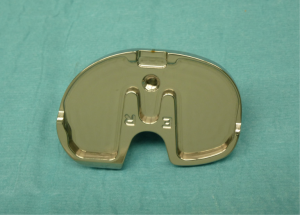
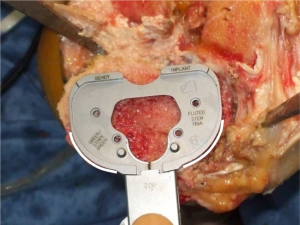
All patients received a posterior-stabilized (PS) fixed-bearing implant. Forty patients (group A: design 1) were randomly selected to receive a Nex-Gen Legacy posterior substituting TKA implant (Nex-Gen LPS, Zimmer, Warsaw, IN, USA), characterized by a symmetric tibial baseplate (Figure 2). Forty patients (group B: design 2) received a Persona, The Personalized Knee System TKA implant (Zimmer, Warsaw, IN, USA), characterized by having an anatomical tibial baseplate (Figure 3).
Intraoperative steps
The surgical approach in all cases included a classic midline skin incision and a standard medial peripatellar capsulotomy. The chosen surgical technique was always a combination of the “balanced gaps technique” (20) and the “measured resection technique” (21): first, a rectangular extension gap was created; secondarily, the rotation of the femoral component was oriented according to the surgical trans-epicondylar (sTEA) axis. All implants were aligned on the coronal plane reproducing patient’s neutral mechanical axis. All cemented PS femoral components (design 1 and 2) were aligned rotationally according to the patient’s sTEA. The rotational alignment of all cemented tibial components (design 1 and 2) was set matching the contour of the tibial anterior cortex (Figure 4) (“Curve-on-Curve Technique” for rotational alignment) (18).
Group 1 (design 1) included 25 females (62.5%) and 15 males (38.5%). Average age was 72 years (range, 60-81 years). Group 2 (design 2) included 24 females (60%) and 16 males (40%). Average age was 71 years (range, 66-80 years). Average preoperative anatomic alignment on standard antero-posterior knee view was 6.1º varus in group 1, and 6.7º varus in group 2 (range, varus 14º, valgus 11º). The differences between the two groups, in terms of epidemiology or preoperative deformity, were not statistically significant.
Total knee arthroplasty (TKA) components evaluation
All knees underwent computed tomography (CT) evaluation in the postoperative period utilizing a GE Healthcare scanning system (Little Chalfont, UK). The scanning protocol included positioning the knee in full extension with the second metatarsal axis in a vertical position according to Berger et al. (22), which has been followed to obtain a reproducible knee position for all CT scans. All images were 2 mm in thickness and with 3 mm in reconstructive increments from the distal metaphysis to the tibial tubercle. Specific software (SECTRA AB, Sectra, Sweden) was utilized for artifact suppression. On the best single femoral axial scan, the sTEA was selected and the femoral PCA was measured. At this point, the sTEA was projected on the tibial axial cut where the ML axis of the tibial baseplate was best identifiable through its “dwell points” (for the symmetric component) or the anterior axis of the polyethylene locking mechanism (for the asymmetric component); the rotation of the tibial component respect to the sTEA was then measured (Figure 5).

For this second study, customized software was created and used to analyze the CT datasets. All selected axial images were evaluated independently by two observers (AG, GP), not involved in the original surgery. They independently repeated the entire measurement process, from point gathering to angles measurement for every knee part of the two study groups. The reproducibility of this method was then calculated by using Bland-Altman analysis for interobserver agreement. The rotational alignment measurements in the two groups were reported as an average value. Statistical analysis was performed using independent two-sample t-test. The calculated P value for statistical significance was set at 0.05.
Results
Symmetric tibial baseplate (design 1)
All forty knees in this study group were available for radiological evaluation at follow-up. The rotational alignment measurement of the symmetric tibial baseplate with respect to the sTEA showed an average external rotation of 1.3º (minimum, 5°; maximum, -1°). All forty tibial components (100%) showed a rotation of 0±5° with respect to the sTEA: 91% showed 0±3° of rotation while 77.5% showed 0±2°. The tibial component appeared 1º internally rotated in 8 cases (20%). The average intraclass correlation coefficient was 0.927. The standard deviation value in this group was 1.826.
Anatomical tibial baseplate (design 2)
None of the patients in this study group were lost at follow-up. The rotational alignment measurement of the anatomical tibial baseplate with respect to the sTEA showed an average external rotation of 4.1º (minimum, 0.4°; maximum, 8.9°). Thirty-one tibial components (77.5%) showed a rotation between 0° and 5° with respect to the sTEA while 8 knees showed an external rotation of 6° and one knee had an external rotation of 8.9°. None of the design 2 tibial baseplates demonstrated internal rotation with respect to the sTEA. The average intraclass correlation coefficient was 0.945. The standard deviation value in this group was 2.276. The calculated P value for statistical significance between design 1 and design 2 group was <0.0001.
Discussion
Historically, rotational malalignment after TKA has been related to patient dissatisfaction and premature failure (8,23,24). While the TEA has been recognized as a primary reference for the rotational alignment of the femoral component (25-28) when the “measured resection” technique (21) is intra-operatively chosen, there is minimum consensus regarding a primary reference for the tibial rotational alignment. In fact, several surgical techniques, each one based on the use of a different anatomical landmark, have been proposed as being accurate for tibial rotational alignment in TKA (29-31).
Many proposed surgical techniques suggest the use of a single point as an intraoperative landmark for correct rotational alignment of the tibial component in TKA. Incavo et al. suggested aligning the antero-posterior axis of the tibial tray with a point close to the medial third of the patellar tendon (32). Lützner et al., in a CT evaluation of 80 TKA, showed that referencing the tibial rotation on a line from the medial third of the tibial tubercle to the center of the tibial tray resulted in a better CT determined femoro-tibial rotational alignment than using the medial border of tibial tubercle as a landmark (10). Matziolis et al. showed that the most prominent point of the tibial tubercle is more accurate than computer navigation for correct tibial component rotational alignment (33). Ikeuchi et al. demonstrated, in an intraoperative and postoperative CT study that using the medial border of the patellar attachment as tibial alignment landmark allows a more accurate tibial baseplate rotational alignment in respect to the range-of-movement technique (31). Recently, Rossi et al., in a cadaveric study, validated the postero-lateral tibial corner as a reliable reference landmark for tibial baseplate rotational alignment (13); however, the identification of this landmark requires a complete exposure of the tibial plateau, which is often difficult to obtain in many knees.
Other surgical techniques suggested the use of an axis or a sagittal plane, in place of a single-point-landmark, for correct rotational alignment. Akagi et al. described a line perpendicular to the projected femoral TEA, starting at the medial third of the tibial tubercle and pointing at the middle of the posterior cruciate ligament tibial insertion (11). Dalury proposed using a line from the mid-point between the tibial spines passing 1 mm medial to the medial border of the tibial tubercle (34). Luo proposed the use of a line perpendicular to the posterior joint surface passing through the medial third of the tibial tubercle (35). Unfortunately, many sagittal axes are not easily and reliably identifiable at surgery. Graw et al. showed high variability of several sagittal axes in relation to different tibial resection levels (36). Nagamine et al. demonstrated that a sagittal antero-posterior axis was less reliable than the PCA for use in tibial rotational alignment in TKA (37). Siston et al., in a study performed at the senior author institution, demonstrated that neither the axis technique nor the single-point reference technique establish a correct tibial rotation alignment (38).
In their first study, the current authors hypothesized that the anterior tibial surface contour was a more reliable landmark for correct tibial component rotational positioning in TKA with respect to other axes or single-landmark references techniques: we showed that, matching the contour of the tibial anterior cortex with a symmetric tibial baseplate, yields to a satisfactory rotational alignment between the femoral and tibial components, at least with the knee in full extension. Optimal coverage in this region may also avoid early loosening of the tibial baseplate: Bloebaum et al. (39), assessing the bone quality after tibial osteotomy, indicated presence of weak bone just posteriorly to the anterior cortex, predisposing tibial baseplates to anterior subsidence if the contact between the tibial baseplate and the anterior cortical is reduced.
In the authors’ second experience, the major finding was the discovery that tibial baseplate designs differ substantially in terms of rotational alignment when using identical anatomical landmarks. The authors recognize that this finding was only validated during CT evaluation of knees in full extension according to their arbitrary femoral sTEA. In the design 1 study group, all forty tibial components (100%) showed a 0±5° of rotation with respect to the surgical TEA: the average rotational alignment was 1.3º of external rotation. For design 2, the practice of aligning the anterior contour of its anatomical tibial baseplate along the anterior tibial cortex led to an average external rotation of the tibial component by more than 4º: none of those tibial baseplates were internally rotated. More than 20% of those tibial baseplates showed an external rotation more than 5º. The authors of the current review and others hypothesized that an excessive external rotation of the tibial component might be detrimental for the survivorship of the polyethylene insert (40).
Hypothetically, anatomic tibial component designs offer increased morphological fit to the proximal tibia compared to non-anatomic designs by improving tibial coverage (14). Several anatomical tibial baseplate designs have been proposed in order to increase the amount of tibial coverage with the goal of reducing the risk of aseptic loosening. Few surgeons, including Wevers et al. (41) and Hartel et al. (42), prefer the use of an asymmetrical/anatomical component maximizing tibial cover in order to provide stability, excellent load transfer in TKA and to mimic the asymmetry of the native tibia. Unfortunately, tibial coverage itself is not sufficient enough to guarantee a satisfactory tibial rotational alignment, leading to major malalignment errors (especially in terms of excessive internal-rotation) when using modern tibial geometries (17,43). On the other hand, tibial coverage of classical designs rarely exceeds 78%. Several authors have proposed a minimum of 75% coverage for adequate fixation; however, this is based on mechanical data and the degree to which this is clinically relevant is still unknown (9). Recently, Dai et al. (14), in a computer model study, suggested that anatomical designs correlate with better tibial coverage and contemporarily more accurate rotational alignment accuracy.
The current authors’ studies have several limitations. The main limitation is the use of a single anatomical landmark (the anterior tibial contour) for tibial rotational alignment, not comparing the rotational alignment of our symmetric or asymmetric tibial components with different alignment intraoperative methods. Our studies do not answer the question as to whether there is an overall optimal orientation of the tibial component during TKA. Both studies were not able to demonstrate if the satisfactory rotational alignment demonstrated with the knee in full extension may be maintained during range-of-motion. On the other side, we propone a simple and reproducible method for tibial component rotational orientation when a symmetric tibial baseplate is utilized: our technique is based on the theory that an alignment between the projected sTEA and the ML tibial baseplate axis is desirable (44,45) when the knee reaches full extension. The authors acknowledge that many surgeons prefer a visual method based on an angular relationship between the tibia and the prosthetic baseplate and rotational incongruity during ROM may be unavoidable, but strongly believe that rotational congruency between femoral and tibial components in full extension is extremely important. Based on the authors studied, it is unclear whether the tibial external-rotation caused by aligning an asymmetric tibial baseplate according to the anterior tibial contour would lead to clinical complications because of lack of clinical and functional results; anyway, the current authors, Martin et al. (17) and Clary et al. (43), all concluded that setting rotational alignment by maximizing coverage should be avoided for all tibial base designs because of the risk of excessive internal rotation. Both studies presented in this review did also not take into consideration the quality of bone that supported the tray and design-specific tibial resections were not investigated. Finally, the presence of osteophytes or significant bone defects may intraoperatively interfere with the resulting tibial resection, anterior profile, or placement of the tibial tray.
Conclusions
The current review did not answer the question on which anatomical landmark and associated surgical technique should be followed during tibial component positioning in primary TKA. On the other side, the authors’ experience suggests that the anterior tibial contour is a trustable and easily identifiable anatomic reference when a symmetric tibial design is intraoperatively chosen. The clinical value of these findings has still to be proven.
Acknowledgements
None.
Footnote
Conflicts of Interest: Part of the results presented in this study has been previously published (references 18 and 19). None of the authors have any financial interest in devices presented in the current study.
References
- Benjamin J. Component alignment in total knee arthroplasty. Instr Course Lect 2006;55:405-12. [PubMed]
- Patel J, Ries MD, Bozic KJ. Extensor mechanism complications after total knee arthroplasty. Instr Course Lect 2008;57:283-94. [PubMed]
- Gonzalez MH, Mekhail AO. The failed total knee arthroplasty: evaluation and etiology. J Am Acad Orthop Surg 2004;12:436-46. [PubMed]
- Hancock CW, Winston MJ, Bach JM, et al. Cylindrical axis, not epicondyles, approximates perpendicular to knee axes. Clin Orthop Relat Res 2013;471:2278-83. [PubMed]
- Iwaki H, Pinskerova V, Freeman MA. Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg Br 2000;82:1189-95. [PubMed]
- Berger RA, Crossett LS, Jacobs JJ, et al. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res 1998.144-53. [PubMed]
- Barrack RL, Schrader T, Bertot AJ, et al. Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res 2001.46-55. [PubMed]
- Bell SW, Young P, Drury C, et al. Component rotational alignment in unexplained painful primary total knee arthroplasty. Knee 2014;21:272-7. [PubMed]
- Bédard M, Vince KG, Redfern J, et al. Internal rotation of the tibial component is frequent in stiff total knee arthroplasty. Clin Orthop Relat Res 2011;469:2346-55. [PubMed]
- Lützner J, Krummenauer F, Günther KP, et al. Rotational alignment of the tibial component in total knee arthroplasty is better at the medial third of tibial tuberosity than at the medial border. BMC Musculoskelet Disord 2010;11:57. [PubMed]
- Akagi M, Oh M, Nonaka T, et al. An anteroposterior axis of the tibia for total knee arthroplasty. Clin Orthop Relat Res 2004.213-9. [PubMed]
- Bindelglass DF. Rotational alignment of the tibial component in total knee arthroplasty. Orthopedics 2001;24:1049-51. [PubMed]
- Rossi R, Bruzzone M, Bonasia DE, et al. Evaluation of tibial rotational alignment in total knee arthroplasty: a cadaver study. Knee Surg Sports Traumatol Arthrosc 2010;18:889-93. [PubMed]
- Dai Y, Scuderi GR, Bischoff JE, et al. Anatomic tibial component design can increase tibial coverage and rotational alignment accuracy: a comparison of six contemporary designs. Knee Surg Sports Traumatol Arthrosc 2014;22:2911-23. [PubMed]
- Cheng FB, Ji XF, Lai Y, et al. Three dimensional morphometry of the knee to design the total knee arthroplasty for Chinese population. Knee 2009;16:341-7. [PubMed]
- Hitt K, Shurman JR 2nd, Greene K, et al. Anthropometric measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. J Bone Joint Surg Am 2003;85-A Suppl 4:115-22. [PubMed]
- Martin S, Saurez A, Ismaily S, et al. Maximizing tibial coverage is detrimental to proper rotational alignment. Clin Orthop Relat Res 2014;472:121-5. [PubMed]
- Baldini A, Indelli PF. Rotational alignment of the tibial component in total knee arthroplasty: the anterior tibial cortex is a reliable landmark. Joints 2014;1:155-60. [PubMed]
- Indelli PF, Graceffa A, Baldini A, et al. Relationship between tibial baseplate design and rotational alignment landmarks in primary total knee arthroplasty. Arthritis 2015;2015:189294.
- Scott WN. Insall & Scott surgery of the knee. 4th ed. Philadelphia: Church Livingstone/Elsevier; 2006.
- Lotke PA, Lonner JH. Knee arthroplasty. 3rd ed. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2009.
- Berger RA, Rubash HE, Seel MJ, et al. Determining the rotational alignment of the femoral component in total knee arthroplasty using the epicondylar axis. Clin Orthop Relat Res 1993.40-7. [PubMed]
- Kawahara S, Okazaki K, Matsuda S, et al. Internal rotation of femoral component affects functional activities after TKA--survey with the 2011 Knee Society Score. J Arthroplasty 2014;29:2319-23. [PubMed]
- Meijer MF, Reininga IH, Boerboom AL, et al. Does imageless computer-assisted TKA lead to improved rotational alignment or fewer outliers? A systematic review. Clin Orthop Relat Res 2014;472:3124-33. [PubMed]
- Aglietti P, Sensi L, Cuomo P, et al. Rotational position of femoral and tibial components in TKA using the femoral transepicondylar axis. Clin Orthop Relat Res 2008;466:2751-5. [PubMed]
- Watanabe S, Sato T, Omori G, et al. Change in tibiofemoral rotational alignment during total knee arthroplasty. J Orthop Sci 2014;19:571-8. [PubMed]
- Asano T, Akagi M, Nakamura T. The functional flexion-extension axis of the knee corresponds to the surgical epicondylar axis: in vivo analysis using a biplanar image-matching technique. J Arthroplasty 2005;20:1060-7. [PubMed]
- Olcott CW, Scott RD. A comparison of 4 intraoperative methods to determine femoral component rotation during total knee arthroplasty. J Arthroplasty 2000;15:22-6. [PubMed]
- Akagi M, Mori S, Nishimura S, et al. Variability of extraarticular tibial rotation references for total knee arthroplasty. Clin Orthop Relat Res 2005.172-6. [PubMed]
- Chowdhury EA, Porter ML. How is the tibial tray aligned to the femoral prosthesis in a total knee arthroplasty? A survey of opinion from BASK? Knee 2005;12:79-80. [PubMed]
- Ikeuchi M, Yamanaka N, Okanoue Y, et al. Determining the rotational alignment of the tibial component at total knee replacement: a comparison of two techniques. J Bone Joint Surg Br 2007;89:45-9. [PubMed]
- Incavo SJ, Coughlin KM, Pappas C, et al. Anatomic rotational relationships of the proximal tibia, distal femur, and patella: implications for rotational alignment in total knee arthroplasty. J Arthroplasty 2003;18:643-8. [PubMed]
- Matziolis G, Krocker D, Weiss U, et al. A prospective, randomized study of computer-assisted and conventional total knee arthroplasty. Three-dimensional evaluation of implant alignment and rotation. J Bone Joint Surg Am 2007;89:236-43. [PubMed]
- Dalury DF. Observations of the proximal tibia in total knee arthroplasty. Clin Orthop Relat Res 2001.150-5. [PubMed]
- Luo CF. Reference axes for reconstruction of the knee. Knee 2004;11:251-7. [PubMed]
- Graw BP, Harris AH, Tripuraneni KR, et al. Rotational references for total knee arthroplasty tibial components change with level of resection. Clin Orthop Relat Res 2010;468:2734-8. [PubMed]
- Nagamine R, Miura H, Inoue Y, et al. Reliability of the anteroposterior axis and the posterior condylar axis for determining rotational alignment of the femoral component in total knee arthroplasty. J Orthop Sci 1998;3:194-8. [PubMed]
- Siston RA, Goodman SB, Patel JJ, et al. The high variability of tibial rotational alignment in total knee arthroplasty. Clin Orthop Relat Res 2006.65-9. [PubMed]
- Bloebaum RD, Bachus KN, Mitchell W, et al. Analysis of the bone surface area in resected tibia. Implications in tibial component subsidence and fixation. Clin Orthop Relat Res 1994.2-10. [PubMed]
- Osano K, Nagamine R, Todo M, et al. The effect of malrotation of tibial component of total knee arthroplasty on tibial insert during high flexion using a finite element analysis. ScientificWorldJournal 2014;2014:695028.
- Wevers HW, Simurda M, Griffin M, et al. Improved fit by asymmetric tibial prosthesis for total knee arthroplasty. Med Eng Phys 1994;16:297-300. [PubMed]
- Hartel MJ, Loosli Y, Delfosse D, et al. The influence of tibial morphology on the design of an anatomical tibial baseplate for TKA. Knee 2014;21:415-9. [PubMed]
- Clary C, Aram L, Deffenbaugh D, et al. Tibial base design and patient morphology affecting tibial coverage and rotational alignment after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2014;22:3012-8. [PubMed]
- Scott RD. Femoral and tibial component rotation in total knee arthroplasty: methods and consequences. Bone Joint J 2013;95-B:140-3. [PubMed]
- Lee DH, Seo JG, Moon YW. Synchronisation of tibial rotational alignment with femoral component in total knee arthroplasty. Int Orthop 2008;32:223-7. [PubMed]