Spinal cord infarct as a presentation of cholangiocarcinoma with metastases
Introduction
Cancer-associated thrombosis (CAT) includes spectrum of diseases ranging from deep vein thrombosis (DVT), pulmonary embolism (PE), arterial thrombosis, nonbacterial thrombotic endocarditis, superficial thrombophlebitis, catheter-related thrombosis to hepatic veno-occlusive disease. It is estimated that the risk of venous thrombosis is 4- to 7-fold higher in cancer patients than general population or patients without cancer (1). Different types of cancer carry different risks of thromboembolism, among which brain, pancreas, lung, and ovarian cancers have the highest risk (1). However, limited data are available for risks of CAT on patients with cholangiocarcinoma. Approximately 13% of cholangiocarcinoma patients developed VTE (2).
Spinal cord infarct (SCI) is a rare disease which contributes to 1.2% of all strokes (3). It is commonly encountered as a complication of major surgery involving thoracic aorta (4). SCI secondary to CAT is very rare, our case seemingly represents the first reported case of SCI due to acquired hypercoagulable state secondary to metastatic cholangiocarcinoma in the English literature.
Case presentation
A 62-year-old African-American woman with past medical history of untreated hepatitis C virus infection presented with worsening shortness of breath. The patient had a computed tomography (CT) angiography which revealed acute segmental PE at right lower lobe. The patient also had a duplex ultrasonography of lower extremities which was reported as chronic bilateral venous thrombosis of superficial femoral vein, popliteal vein and great saphenous vein. Vital signs upon presentation showed a temperature of 98.2 °F, heart rate 117 beats per minute, blood pressure 157/77 mmHg, and oxygen saturation 98% on 2 L nasal cannula. Physical examination was remarkable for mild respiratory distress, conjunctival pallor, mild right upper abdominal tenderness, and a tender, swollen left lower extremity. There was also a palpable, firm left supraclavicular lymph node measuring 1 cm in diameter. Laboratory studies showed a hemoglobin concentration of 6.8 g/dL, white blood cell count 14.8×103/µL with left shift, and platelet count 128×103/µL. She was admitted and treated with enoxaparin, and she received one unit of blood transfusion.
One month ago, the patient presented to our facility with persistent right flank pain. She was found to have an incidental 9.8 cm × 7.7 cm × 3.5 cm mass within the right hepatic lobe suspicious of hepatocellular carcinoma on CT scan of the abdomen. Subsequent magnetic resonance imaging (MRI) with contrast showed a 6 cm × 6.4 cm early enhancing and rapid washout mass lesion which was suggestive of hepatocellular carcinoma. However, there were also multiple lesions in right and left lobes of the liver suggesting intrahepatic metastases. She was placed for follow-up with an oncologist as outpatient.
On the fourth day of hospital stay, patient complained of sudden onset of lumbar back pain, tingling, numbness and weakness of lower extremities. On neurological examination of lower extremities, she was noted to have decreased sensation of pain, temperature and vibration below the L1 dermatome level bilaterally. She had a flaccid paralysis of both lower extremities as well. Reflexes were absent in the patellar and Achilles tendons. Complete neurological examinations of upper extremities as well as cranial nerve were unremarkable.
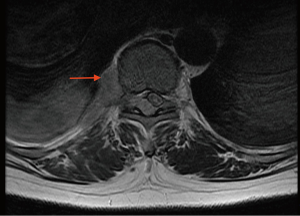
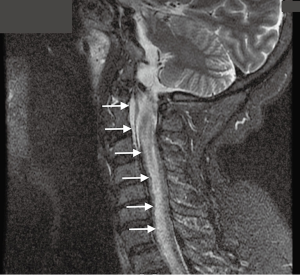
MRI studies of the lumbar and thoracic spine demonstrated a 1.8 cm × 2.6 cm right paraspinal mass at T10 level (Figure 1) with extension into the right epidural space posterolaterally. In addition, there was a bright T2 signal area extending from T6 through to conus medullaris (Figure 2) which was consistent with subacute SCI. Patient’s neurological deficit had progressed to upper extremities over the next 3 days with worsening respiratory distress requiring immediate intubation and ventilator support. MRI of cervical spine (Figure 3) was performed the following day due to worsening of ascending paralysis, and findings were also suggestive of subacute infarction.

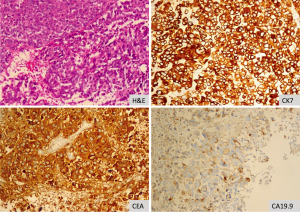
Histopathological examination of supraclavicular lymph node was performed, to evaluate for malignancy, which revealed pleomorphic malignant cells consistent with high-grade carcinoma. Immunohistochemical analysis was positive for CK7, CK20, CDX-2, pCEA, CA19.9 and vimentin but negative for Hep-Par-1, AFP, Glypican-3, TTF-1, Napsin-A, GATA-3, melanin-A and S-100 as shown in Figure 4. In conjunction with the early washing out in imaging study, and multiple masses throughout the liver, it is highly suggestive of metastatic poorly differentiated cholangiocarcinoma. Serum tumor markers such as CA 19-9 was 23.5 µg/mL (reference range 0.00-37.0 µg/mL), CA 125 was 11.6 µg/mL (reference range 1-35 µg/mL) and AFP was 6 ng/mL (reference level <6.1 ng/mL).
Outcome and follow up
The patient died from infection and metabolic derangements approximately 2 weeks after diagnosis of extensive SCI despite treatments with antibiotics, anticoagulation and full ventilator support.
Discussion
The association between cancer and thrombosis was first described in 1823 by the French physician Jean-Baptiste Bouillaud (5). Armand Trousseau, a well-known French internist, also noticed an association between venous thromboembolism and occult malignancy in 1865 (6). Currently, it is widely recognized as CAT which comprises DVT, PE, arterial thrombosis, nonbacterial thrombotic endocarditis, superficial thrombophlebitis, catheter-related thrombosis, and hepatic veno-occlusive disease. CAT is accountable for approximately 20% to 30% of all first VTE. Cancers of brain, pancreas, lung, and ovary are the most thrombogenic (1); however, data are limited for thrombogenicity of cholangiocarcinoma possibly due to its aggressive nature and advanced stage at diagnosis.
Our case represents the first reported case of SCI associated with cholangiocarcinoma. She had a high risk for thrombosis, proven by DVT and PE on presentation, which further progressed to SCI despite treatment with anticoagulation. It is unlikely that paraspinal mass at T10 caused paraplegia because there was no evidence of spinal cord compression on imaging studies. In addition, rapidly developed subsequent upper extremity paralysis secondary to SCI indicates vascular event which could be arterial thrombosis and embolism, venous thrombosis or tumor embolization.
Multiple factors such as clinical and complex biological factors contribute to the pathogenesis of CAT. Increased expression of tissue factor (TF) on tumor cells is the principal biologic mechanism causing CAT. TF expression can also be potentiated by heparanase which causes dissociation of TF pathway inhibitor on the surface of endothelial and tumor cells. TF induces thrombin generation as well as expression of VEGF on malignant and host vascular cells with subsequent neo-vascularization, tumor cell growth, coagulation, and thrombosis (7).
Cholangiocarcinoma, a malignancy of the biliary duct system arising from the malignant transformation of bile duct epithelial cells, attributes about 15% of primary hepatic neoplasm. The prevalence of cholangiocarcinoma in the United States is ~1.22/100,000 in Hispanics and ~0.3/100,000 in African American population (8). There have been cases of DVT, PE, portal vein thrombosis, hepatic vein thrombosis, and inferior vena cava thrombosis secondary to cholangiocarcinoma (2), however, there is no reported case of cholangiocarcinoma presented with SCI most likely secondary to arterial thrombosis. Nevertheless, the prognosis of advanced unresectable cholangiocarcinoma is extremely poor without surgery, chemotherapy or radiotherapy (9). Moreover, the presence of metastasis and thrombotic events are associated with much more dismal outcome (2,9).
Conclusions
The association linking between SCI and metastatic cholangiocarcinoma has never been reported previously. Multiple risk factors are involved in the development of thromboembolic complications in cancer patients with high impact on morbidity and mortality. Although SCI is rare, it is often a devastating disorder with poor patient outcome.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Timp JF, Braekkan SK, Versteeg HH, et al. Epidemiology of cancer-associated venous thrombosis. Blood 2013;122:1712-23.
- Jeon HK, Kim DU, Baek DH, et al. Venous thromboembolism in patients with cholangiocarcinoma: focus on risk factors and impact on survival. Eur J Gastroenterol Hepatol 2012;24:444-9.
- Sandson TA, Friedman JH. Spinal cord infarction. Report of 8 cases and review of the literature. Medicine (Baltimore) 1989;68:282-92.
- Robertson CE, Brown RD Jr, Wijdicks EF, et al. Recovery after spinal cord infarcts: long-term outcome in 115 patients. Neurology 2012;78:114-21.
- Bouillard JB, Bouillaud S. De l'Obliteration des veines et de son influence sur la formation des hydropisies partielles: consideration sur la hydropisies passive et general. Arch Gen Med 1823;1:188-204.
- Trousseau A. Phlegmasia alba dolens. Clin Med Hotel Dieu Paris 1865;3:654-712.
- Falanga A, Marchetti M, Vignoli A. Coagulation and cancer: biological and clinical aspects. J Thromb Haemost 2013;11:223-33.
- McLean L, Patel T. Racial and ethnic variations in the epidemiology of intrahepatic cholangiocarcinoma in the United States. Liver Int 2006;26:1047-53.
- Park J, Kim MH, Kim KP, et al. Natural History and Prognostic Factors of Advanced Cholangiocarcinoma without Surgery, Chemotherapy, or Radiotherapy: A Large-Scale Observational Study. Gut Liver 2009;3:298-305.


