Improved survival with the addition of radiotherapy to androgen deprivation: questions answered and a review of current controversies in radiotherapy for non-metastatic prostate cancer
A recent report by Mason et al. (1) presented the updated results of the National Cancer Institute of Canada (NCIC Clinical Trials Group PR.3/Medical Research Council PR07/Intergroup T94-0110) (PMID 25691677) randomized trial comparing androgen-deprivation therapy (ADT) plus radiotherapy (RT) vs. ADT alone for locally-advanced non-metastatic prostate cancer. The NCIC/MRC trial evaluated 1,205 patients with high-risk prostate cancer, including patients with T3-4 N0/Nx M0 disease or T1-2 with a PSA >40 ng/mL or prostate-specific antigen (PSA) 20-40 ng/mL and Gleason score (GS) 8-10. Patients were randomized to lifelong ADT alone vs. ADT + RT with a primary endpoint of overall survival (OS). Patients randomized to the RT arm received a total dose to the prostate of 65-69 Gy delivered with a four-field box technique. Whole pelvic RT (WPRT) to 45 Gy was delivered in 72% of RT patients, while 28% received prostate RT alone at the discretion of the treating physician. Nodal staging by imaging and/or surgery was not required. ADT included either intended lifelong treatment with luteinizing hormone-releasing hormone (LHRH) agonists (92%) or orchiectomy (8%). Quality of life forms were used to assess toxicity. Biochemical relapse was defined as a PSA >10 ng/mL (later refined to reflect the Phoenix definition of PSA nadir plus 2 ng/mL) (2). The study was opened in 1995 and accrued patients until 2005; two interim analyses were performed prior to closing. After 320 deaths at the second interim analysis, the study had met stopping criteria by the data safety monitoring committee and was closed.
In the initial analysis presented by Warde et al. in 2011 (3), the addition of RT to ADT resulted in a significant improvement in OS (HR =0.77; P=0.03); 7-year OS for ADT + RT vs. ADT alone was 74% and 66% respectively. RT also reduced the risk of death from prostate cancer by approximately 50% (HR =0.54; P<0.001). Higher rates of short-term genitourinary and gastrointestinal toxicities in the ADT + RT cohort were observed; however, long-term toxicities were comparable in both groups. In the updated results presented by Mason et al. (1), with nearly 8 years of follow up, the benefits of RT remained for both OS (HR =0.70; P<0.001) and disease-free survival (DFS) (HR =0.46; P<0.001), with further improvement in the hazard ratios in the updated analysis. The 10-year biochemical progression-free rates using the Phoenix definition were 63% with ADT + RT vs. 27% with ADT alone. Additional toxicities including sexual function and cardiovascular were reported in the update and demonstrated no significant difference between the two groups. In conjunction with this publication, Brundage et al. (4) published quality of life outcomes from the trial, showing no significant difference in patient reported outcomes at 3 years.
Parallel results to the NCIC/MRC study were reported in a similar multicenter Scandanavian trial, the SPCG-7/SFUO-3 (5), which had several distinguishing features from the NCIC/MRC study design. The Scandanavian trial including patients with slightly lower risk features (T1b-T2, grade 2-3, or T3 with any grade, and a PSA ≤70 ng/mL), prostate-only radiation to 70 Gy (without pelvic lymph node RT), mandatory surgical nodal staging of the obturator fossa for patients with PSAs ≥11 ng/mL, and ADT consisting of 3 months of LHRH agonist followed by lifelong androgen receptor blockage with flutamide. The final results of the Scandinavian trial demonstrated similar improvements with RT to the NCIC/MRC trial in terms of OS (HR =0.52; P=0.004) and DFS (HR =0.44; P<0.001). The 10-year biochemical progression-free rates were 75% vs. 26% for the ADT + RT and ADT cohorts, respectively. The results from this study were published alongside the patient-reported quality of life, also demonstrating higher short-term toxicities in the ADT + RT cohort but again no significant difference in long-term quality of life outcomes (6).
Historical context is useful to consider when evaluating the designs of these landmark trials. Although, at the time of trial initiation the best outcomes for men with locally-advanced non-metastatic cancer had been observed with combination therapy, many clinicians wondered if the favorable survival outcomes were, in fact, driven by ADT alone. Ultimately, the NCIC/MRC and Scandanavian trials would each demonstrate a 50% reduction in prostate cancer specific-mortality with the addition of RT to ADT and laid this fundamental question to rest. However, over the past 20 years a battery of more granular questions regarding the optimal combined-modality RT strategy for prostate cancer have emerged. Since the initiation of these trials, intensity-modulated radiotherapy (IMRT) has supplanted the 3D techniques used in these studies and dose-escalated RT (e.g., total doses of 76-82 Gy in conventional fractionation) has become the standard of care in the wake of multiple randomized trials demonstrating improvements in progression-free survival (PFS) with dose-escalation over lower doses of approximately 70 Gy or less (7-12). Moreover, the lifelong ADT used in the NCIC/MRC trial has been replaced by contemporary recommendations of 2-3 years for patients with high-risk disease, with numerous reported and ongoing studies aiming to refine the ADT recommendations with improved risk stratifications. Here, we address a number of the contemporary controversies in RT for non-metastatic prostate cancer in the context of the final results of the NCIC/MRC randomized trial.
Is it reasonable to omit ADT in the setting of dose-escalated radiotherapy for patients with intermediate-risk prostate cancer?
This is an area of considerable debate and the topic of an ongoing North American cooperative randomized trial [Radiation Therapy Oncology Group (RTOG) 0815] for patients with intermediate-risk prostate cancer (clinical stage T2b or T2c, GS of 7, or PSA of 10-20 ng/mL). Interestingly, it is also the inverse question to that of NCIC/MRC trial and a return to a question which has been addressed numerous times in favor of ADT for patients with high-risk disease, albeit in the setting of lower doses radiation between 60-70 Gy (citations). Among patients with intermediate-risk disease, several studies predating dose-escalated RT have also reported improved OS with the addition of short-term ADT to RT (13,14). The RTOG 9408 trial included mostly low- and intermediate-risk patients all receiving conventional RT, 66.6 Gy, with or without 4 months of ADT. In that study, ADT resulted in an OS improvement of 5% at 10 years, largely driven by the intermediate-risk cohort (13). Similarly D’Amico et al. reported a randomized trial including predominately intermediate-risk patients, randomized to conventional RT (70 Gy) with or without 6 months ADT (14). After a median follow up of 8 years, the addition of ADT yielded an absolute OS benefit of 10% (P=0.04). It is debated whether the benefits of ADT for men with intermediate-risk disease may simply be a compensation for the suboptimal doses delivered in these older studies or, alternatively, if the benefits observed with ADT were related to independent and synergistic benefits when combined with RT irrespective of radiation dose. Certainly, the appeal of eliminating the need for ADT in the treatment regimen for men with intermediate-risk prostate cancer is related to its typical side effect profile: erectile dysfunction, fatigue, weight gain, osteoporosis, insulin resistance, and risk of cardiovascular disease (15,16).
Several more recent studies have evaluated the role of ADT for intermediate-risk patients in the setting of dose-escalated RT. The Groupe d’Etude des Tumeurs Uro-Genitales 14 (GETUG 14) presented preliminary results on a prospective randomized trial including 377 patients receiving dose-escalation (80 Gy) randomized to RT alone or RT and 4 months of ADT (17). Median follow up was 27 months and the trial was closed prematurely due to slow accrual; results showed a trend for improved biochemical and local control in the ADT arm (P=0.09). A recent phase III trial of short-term ADT for intermediate risk patients was presented at the American Society of Clinical Oncology (ASCO) 2015 conference (18). The study, consisted of 600 patients, randomized one of three arms. Including 6 months of ADT with 70 Gy (arm 1), 6 months of ADT with 76 Gy (arm 2), or 76 Gy RT alone (arm 3). At a median follow up of 6.5 years, there was a significant DFS benefit with the addition of ADT to 76 Gy of RT; although, this did not translate to significant OS benefit. Zumsteg et al. retrospectively reviewed 710 intermediate risk prostate patients treated with high-dose RT (≥81 Gy), demonstrating a significant PSA relapse-free survival difference, favoring those who received ADT, especially in patients with a GS 4+3 or percent positive cores ≥50% (19). In contrast, other retrospective studies have observed no benefit with the addition of ADT to dose-escalated RT for intermediate-risk patients (20,21). Valicenti et al. analyzed 883 patients enrolled on RTOG 9406, a phase I/II dose escalation (mean dose of 78.4 Gy), who either did or did not receive short-term ADT at the discretion of the treating physician (20). At a median follow up of 7 years for the intermediate-risk group, there was no significant benefit from ADT in terms of biochemical failure or DFS; only the high-risk population approached significance. Given the conflicting results between studies, differences in RT doses across eras, and the potential role of selection bias in retrospective analyses, the role of ADT for intermediate-risk patients remains unclear. The accruing RTOG 0815, which randomizes intermediate-risk patients to 6 months of ADT with dose-escalated RT vs. dose-escalated RT alone, is designed specifically to address this question. In the meantime, the NCCN (22) and ESMO (23) guidelines continue to recommend “consideration” of 4-6 months of ADT for patients with intermediate-risk prostate cancer.
What is the optimal duration of ADT for patients with high-risk prostate cancer in the dose-escalation era?
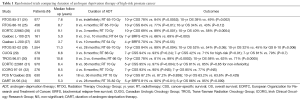
The NCIC/MRC study included intended lifelong ADT. However, since the initiation of that trial, multiple studies for patients with high-risk prostate cancer have addressed the optimal duration of ADT (Table 1) (24-34). The European Organization for Research and Treatment of Cancer (EORTC) 22961 study compared 6 vs. 36 months of ADT in patients treated to 70 Gy and found an improvement in 5-year OS with long-term ADT (31), defining 36 months as a de facto standard duration for high-risk prostate cancer. Given long-term toxicities from extended ADT use, more recent studies have attempted to reduce the duration of ADT. Abstract results from a phase III non-inferiority Canadian study comparing 18 vs. 36 months of ADT for high-risk disease treated to 70 Gy found no difference in OS, DFS, or rates of biochemical, regional or distant failure at 10 years (33). In the dose-escalation era, the Duration of Androgen-Deprivation Therapy (DART) 01/05 study compared 4 vs. 28 months of ADT delivered with 76-82 Gy and reported improved 5-year outcomes with longer ADT duration for OS, biochemical DFS and metastasis-free survival at a median follow up of 63 months (34). While provocative, the DART trial had some limitations including higher rates of unknown death in the short-term ADT arm, suggesting the presence of competing risks. In the United States, the ongoing phase III randomized RTOG 0924 trial evaluating the benefit of whole-pelvic RT (WPRT) may also indirectly address the duration of ADT for high-risk, with the inclusion of ADT courses of 6 vs. 32 months chosen at the discretion of the physician (35).
Full table
Should the pelvic lymph nodes be treated in addition to the prostate for patients with high-risk prostate cancer?
A subgroup analysis of the NCIC/MRC trial addressed the role of WPRT compared to prostate-only (PO-RT), used at the physician’s discretions in 72% and 28% of patients in the RT cohort, respectively. In this post hoc analysis, no significant differences in OS were reported, although the authors commented that a trend was observed toward improved survival with WPRT over PO-RT (HR =0.70; 95% CI, 0.45-1.09; P=0.12). In their discussion, however, the authors rightly point out the importance of selection bias, low patient numbers, and lack of nodal staging as potential contributing factors. Notably, the Scandinavian trial also demonstrated similar improvements in all oncologic endpoints to the NCIC/MRC study without the use of WPRT.
The role of WPRT for high-risk prostate cancer continues to be an area of controversy in the field of radiation oncology. To date, three randomized studies have failed to demonstrate a benefit with the addition of WPRT in node-negative prostate cancer (Table 2). The RTOG 7706 trial reported results of 445 prostate cancer patients in the pre-PSA era, which presented with clinical T1c-2c, and were randomized to WPRT vs. PO-RT; at 12-year median follow-up, no survival difference was detected (36). This was followed by RTOG 9413, which examined the role of WPRT in patients with ≥15% risk of lymph node involvement based on the Roach formula (37,38,42). The study included four arms: (I) WPRT with neoadjuvant and concurrent ADT (NCHT); (II) WPRT with adjuvant ADT (AHT); (III) PO-RT with NCHT; and (IV) PO-RT with AHT. Initial results demonstrated a significant improvement in 4-year PFS, favoring WPRT (54% vs. 47%; P=0.022); WPRT with NCHT had the highest 4-year PFS (60%). However, when Lawton et al. (38) published the updated results of RTOG 9413 after a median follow up of 6.6 years, no statistically significant differences were found in PFS or OS between NHT vs. AHT and WPRT vs. PO-RT, rendering the RTOG 9413 a negative study with mature follow up. Lastly, Groupe d’Etude des Tumeurs Uro-Genitales 01 (GETUG 01), which included all localized, node-negative prostate cancer patients (irrespective of risk category) also demonstrated no difference in PFS between WPRT and PO-RT (39). These results have also been redemonstrated in non-randomized analyses of more modern treatment cohorts. The GETUG 12 randomized phase III study evaluating the role of ADT plus docetaxel and estramustine for high-risk prostate cancer patients performed an unplanned secondary analysis to evaluate the role of elective nodal RT for high-risk, clinically node-negative prostate cancer and found no benefit with WPRT. A recent review of the National Cancer Data Base (NCDB) performed at our institution confirmed the above findings, again demonstrating no OS differences with WPRT for high-risk, node-negative prostate cancer, even in the present dose-escalation era (43). Nevertheless, the topic of WPRT for high risk clinically node negative patients will be debated until the results of RTOG 0924 (35), the European PEACE2 study (40), and the United Kingdom PIVOTAL trial (41) mature and, perhaps, irrespective of their results.

Full table
Conclusions
At the design of the NCIC/MRC study the survival impact of RT for locally-advanced prostate cancer was debated within the urologic oncology community. The updated study results presented by Mason et al. provides closure to this topic and confirms that local control of high-risk prostate cancer categorically improves survival at long term follow up. Close examination of subtleties of this trial’s design and era of treatment also highlight some of the most salient controversies in the contemporary era of IMRT and dose-escalated RT, including the risk-stratified roles of ADT, optimal ADT duration, and RT field design.
Acknowledgements
None.
Footnote
Provenance: This is a Guest Editorial commissioned by Bo Fan, MD, PhD (Department of Urology, the First Affiliated Hospital of Dalian Medical University, Dalian, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Mason MD, Parulekar WR, Sydes MR, et al. Final report of the intergroup randomized study of combined androgen-deprivation therapy plus radiotherapy versus androgen-deprivation therapy alone in locally advanced prostate cancer. J Clin Oncol 2015;33:2143-50. [PubMed]
- Roach M 3rd, Hanks G, Thames H Jr, et al. Defining biochemical failure following radiotherapy with or without hormonal therapy in men with clinically localized prostate cancer: recommendations of the RTOG-ASTRO Phoenix Consensus Conference. Int J Radiat Oncol Biol Phys 2006;65:965-74. [PubMed]
- Warde P, Mason M, Ding K, et al. Combined androgen deprivation therapy and radiation therapy for locally advanced prostate cancer: a randomised, phase 3 trial. Lancet 2011;378:2104-11. [PubMed]
- Brundage M, Sydes MR, Parulekar WR, et al. Impact of Radiotherapy When Added to Androgen-Deprivation Therapy for Locally Advanced Prostate Cancer: Long-Term Quality-of-Life Outcomes From the NCIC CTG PR3/MRC PR07 Randomized Trial. J Clin Oncol 2015;33:2151-7. [PubMed]
- Widmark A, Klepp O, Solberg A, et al. Endocrine treatment, with or without radiotherapy, in locally advanced prostate cancer (SPCG-7/SFUO-3): an open randomised phase III trial. Lancet 2009;373:301-8. [PubMed]
- Fransson P, Lund JA, Damber JE, et al. Quality of life in patients with locally advanced prostate cancer given endocrine treatment with or without radiotherapy: 4-year follow-up of SPCG-7/SFUO-3, an open-label, randomised, phase III trial. Lancet Oncol 2009;10:370-80. [PubMed]
- Zietman AL, DeSilvio ML, Slater JD, et al. Comparison of conventional-dose vs high-dose conformal radiation therapy in clinically localized adenocarcinoma of the prostate: a randomized controlled trial. JAMA 2005;294:1233-9. [PubMed]
- Michalski JM, Moughan J, Purdy J et al. A randomized trial of 79.2 Gy versus 70.2 Gy radiation therapy (RT) for localized prostate cancer. J Clin Oncol 2015;33:abstr 4.
- Kuban DA, Levy LB, Cheung MR, et al. Long-term failure patterns and survival in a randomized dose-escalation trial for prostate cancer. Who dies of disease? Int J Radiat Oncol Biol Phys 2011;79:1310-7. [PubMed]
- Dearnaley DP, Jovic G, Syndikus I, et al. Escalated-dose versus control-dose conformal radiotherapy for prostate cancer: long-term results from the MRC RT01 randomised controlled trial. Lancet Oncol 2014;15:464-73. [PubMed]
- Heemsbergen WD, Al-Mamgani A, Slot A, et al. Long-term results of the Dutch randomized prostate cancer trial: impact of dose-escalation on local, biochemical, clinical failure, and survival. Radiother Oncol 2014;110:104-9. [PubMed]
- Beckendorf V, Guerif S, Le Prisé E, et al. 70 Gy versus 80 Gy in localized prostate cancer: 5-year results of GETUG 06 randomized trial. Int J Radiat Oncol Biol Phys 2011;80:1056-63. [PubMed]
- Jones CU, Hunt D, McGowan DG, et al. Radiotherapy and short-term androgen deprivation for localized prostate cancer. N Engl J Med 2011;365:107-18. [PubMed]
- D'Amico AV, Manola J, Loffredo M, et al. 6-month androgen suppression plus radiation therapy vs radiation therapy alone for patients with clinically localized prostate cancer: a randomized controlled trial. JAMA 2004;292:821-7. [PubMed]
- O'Farrell S, Garmo H, Holmberg L, et al. Risk and timing of cardiovascular disease after androgen-deprivation therapy in men with prostate cancer. J Clin Oncol 2015;33:1243-51. [PubMed]
- Herr HW, O'Sullivan M. Quality of life of asymptomatic men with nonmetastatic prostate cancer on androgen deprivation therapy. J Urol 2000;163:1743-6. [PubMed]
- Dubray BM, Beckendorf V, Guerif S et al. Does short-term androgen depletion add to high-dose radiotherapy (80 Gy) in localized intermediate-risk prostate cancer? Intermediary analysis of GETUG 14 randomized trial (EU-20503/NCT00104741). J Clin Oncol 2011;29:abstr 4521.
- Nabid A, Carrier N, Vigneault C, et al. A phase III trial of short-term androgen deprivation therapy in intermediate-risk prostate cancer treated with radiotherapy. J Clin Oncol 2015;33:abstr 5019.
- Zumsteg ZS, Spratt DE, Pei X, et al. Short-term androgen-deprivation therapy improves prostate cancer-specific mortality in intermediate-risk prostate cancer patients undergoing dose-escalated external beam radiation therapy. Int J Radiat Oncol Biol Phys 2013;85:1012-7. [PubMed]
- Valicenti RK, Bae K, Michalski J, et al. Does hormone therapy reduce disease recurrence in prostate cancer patients receiving dose-escalated radiation therapy? An analysis of Radiation Therapy Oncology Group 94-06. Int J Radiat Oncol Biol Phys 2011;79:1323-9. [PubMed]
- Krauss D, Kestin L, Ye H, et al. Lack of benefit for the addition of androgen deprivation therapy to dose-escalated radiotherapy in the treatment of intermediate- and high-risk prostate cancer. Int J Radiat Oncol Biol Phys 2011;80:1064-71. [PubMed]
- National Comprehensive Cancer Network (NCCN) Guidelines. Prostate Cancer. Version I.2015. Available online: http://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf
- Parker C, Gillessen S, Heidenreich A, et al. Cancer of the prostate: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up†. Ann Oncol 2015;26 Suppl 5:v69-77. [PubMed]
- Pilepich MV, Winter K, Lawton CA, et al. Androgen suppression adjuvant to definitive radiotherapy in prostate carcinoma--long-term results of phase III RTOG 85-31. Int J Radiat Oncol Biol Phys 2005;61:1285-90. [PubMed]
- Roach M 3rd, Bae K, Speight J, et al. Short-term neoadjuvant androgen deprivation therapy and external-beam radiotherapy for locally advanced prostate cancer: long-term results of RTOG 8610. J Clin Oncol 2008;26:585-91. [PubMed]
- Bolla M, Van Tienhoven G, Warde P, et al. External irradiation with or without long-term androgen suppression for prostate cancer with high metastatic risk: 10-year results of an EORTC randomised study. Lancet Oncol 2010;11:1066-73. [PubMed]
- Laverdière J, Nabid A, De Bedoya LD, et al. The efficacy and sequencing of a short course of androgen suppression on freedom from biochemical failure when administered with radiation therapy for T2-T3 prostate cancer. J Urol 2004;171:1137-40. [PubMed]
- Horwitz EM, Bae K, Hanks GE, et al. Ten-year follow-up of radiation therapy oncology group protocol 92-02: a phase III trial of the duration of elective androgen deprivation in locally advanced prostate cancer. J Clin Oncol 2008;26:2497-504. [PubMed]
- Crook J, Ludgate C, Malone S, et al. Final report of multicenter Canadian Phase III randomized trial of 3 versus 8 months of neoadjuvant androgen deprivation therapy before conventional-dose radiotherapy for clinically localized prostate cancer. Int J Radiat Oncol Biol Phys 2009;73:327-33. [PubMed]
- Denham JW, Steigler A, Lamb DS, et al. Short-term neoadjuvant androgen deprivation and radiotherapy for locally advanced prostate cancer: 10-year data from the TROG 96.01 randomised trial. Lancet Oncol 2011;12:451-9. [PubMed]
- Bolla M, de Reijke TM, Van Tienhoven G, et al. Duration of androgen suppression in the treatment of prostate cancer. N Engl J Med 2009;360:2516-27. [PubMed]
- Armstrong JG, Gillham CM, Dunne MT, et al. A randomized trial (Irish clinical oncology research group 97-01) comparing short versus protracted neoadjuvant hormonal therapy before radiotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys 2011;81:35-45. [PubMed]
- Nabid A, Carrier N, Martin AG, et al. Duration of androgen deprivation therapy in high-risk prostate cancer: A randomized trial. J Clin Oncol 2013;31:abstr LBA4510.
- Zapatero A, Guerrero A, Maldonado X, et al. High-dose radiotherapy with short-term or long-term androgen deprivation in localised prostate cancer (DART01/05 GICOR): a randomised, controlled, phase 3 trial. Lancet Oncol 2015;16:320-7. [PubMed]
- RTOG 0924 Protocol Information. Available online: https://www.rtog.org/ClinicalTrials/ProtocolTable/StudyDetails.aspx?study=0924
- Asbell SO, Krall JM, Pilepich MV, et al. Elective pelvic irradiation in stage A2, B carcinoma of the prostate: analysis of RTOG 77-06. Int J Radiat Oncol Biol Phys 1988;15:1307-16. [PubMed]
- Roach M 3rd, DeSilvio M, Lawton C, et al. Phase III trial comparing whole-pelvic versus prostate-only radiotherapy and neoadjuvant versus adjuvant combined androgen suppression: Radiation Therapy Oncology Group 9413. J Clin Oncol 2003;21:1904-11. [PubMed]
- Lawton CA, DeSilvio M, Roach M 3rd, et al. An update of the phase III trial comparing whole pelvic to prostate only radiotherapy and neoadjuvant to adjuvant total androgen suppression: updated analysis of RTOG 94-13, with emphasis on unexpected hormone/radiation interactions. Int J Radiat Oncol Biol Phys 2007;69:646-55. [PubMed]
- Pommier P, Chabaud S, Lagrange JL, et al. Is there a role for pelvic irradiation in localized prostate adenocarcinoma? Preliminary results of GETUG-01. J Clin Oncol 2007;25:5366-73. [PubMed]
- A Phase III of Cabazitaxel and Pelvic Radiotherapy in Localized Prostate Cancer and High-Risk Features of Relapse (PEACE2). Available online: https://clinicaltrials.gov/ct2/show/NCT01952223
- A Study of Prostate and pelvIs Versus prOsTate Alone Treatment for Locally Advanced Prostate Cancer (PIVOTAL). Available online: https://clinicaltrials.gov/ct2/show/NCT01685190
- Roach M 3rd, Marquez C, Yuo HS, et al. Predicting the risk of lymph node involvement using the pre-treatment prostate specific antigen and Gleason score in men with clinically localized prostate cancer. Int J Radiat Oncol Biol Phys 1994;28:33-7. [PubMed]
- Amini A, Jones B, Yeh N, et al. Survival Outcomes of Whole-Pelvic Versus Prostate-Only Radiotherapy for High-Risk Prostate Cancer Patients Using the National Cancer Data Base. Int J Radiat Oncol Biol Phys. In Press.


