Body fluid biomarkers in Alzheimer’s disease
Introduction
Dem.entia is a major global cause of disability and dependency. As of 2013, an estimated 44.4 million people had dementia worldwide; by 2030, this number will almost double to an estimated 75.6 million, and then almost double again to 135.5 million in 2050. Much of the increase will be in developing countries with the fastest growth in the elderly population. People with dementia living in developing countries have accounted for already 62% of all patients, but by 2050 this will rise to 71%. The total estimated global societal direct and indirect cost of dementia in 2010 was $604 billion (http://www.alz.co.uk/research/statistics). That will be a big challenge, and most of health care systems will be unable to deal with this development.
Alzheimer’s disease (AD), living in the global the third lethal disease (1), is a complex progressive neurodegenerative disease that is characterized by an irreversible cognitive functions decline, a loss of memory and a high degree of heterogeneity in clinical and radiological. Biomarkers can be defined as “a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes or pharmacological responses to a therapeutic intervention” (2). Therefore, biomarkers that reliably capture the different aspects of disease heterogeneity are needed, and might help to better understand AD aetiopathogenesis, diagnosis, and prognosis, to predict response outcome to treatments, and to develop new treatments.
The AD biomarker research field is always very active during several decades. The most famous theory, the “amyloid cascade hypothesis” for AD (3) posits that an imbalance between the production and clearance of β-amyloid (Aβ) is the initiating event in disease pathogenesis, ultimately leading to tauopathy, neurodegeneration, and cognitive and behavioral changes. Aβ was proposed as the initiating factor in the disease process which is correlated with β-amyloid precursor protein (APP) metabolism, Aβ generation and tau protein homeostasis. Mayeux and Stern (4) found that the lesions associated with the disease could begin decades prior to the emergence of clinical symptoms. Disease-modifying drugs will probably be more effective in the earlier stages of the disease, because in advanced AD patients plaque and tangle load as well as neurodegeneration will become highly severe (5-7). Thus, to find some useful early biomarkers is crucial, which might help to improve the diagnosis of AD especially prodromal or preclinical AD. It will most likely slow down disease progression and cut the morbidity and mortality by the early intervention. In spite of a substantial number of candidate biomarkers proposed and theories established, few biomarkers can meet the full needs of clinically useful biomarkers, which lead to another important challenge. In this review, we focus on some established biomarkers evaluated in several different studies and an assortment of novel biomarkers in AD, as well as their potential roles in clinical trials.
Aβ isoforms
Some of this category of biomarkers such as, cerebrospinal fluid (CSF) Aβ42 and Aβ40 isoforms, are repeatedly validated by different groups in an independent cohort of patients with AD, and even are currently used in AD clinical practice. In the wake of the development of so-called omics technologies which have enabled the identification of novel biomarkers in an unbiased and semiquantitative way (8), biomarker discovery has been strongly boosted in the past decades. Simultaneously, an assortment of technological approaches such as two-dimensional polyacrylamide gel electrophoresis and mass spectrometer analysis are employed in the exploration of biomarkers. Human beings have been able to employ a great diversity of novel Aβ isoforms to investigate the secrets of AD. Given β-site APP cleaving enzyme 1 (BACE1) and soluble amyloid precursor proteins α and β (sAPPα/sAPPβ) significantly associated with the metabolism of APP and the production of Aβ; much attentions were paid to both of them.
Cerebrospinal fluid Aβ isoforms
The discovery that playing a central role in the pathogenesis of AD, Aβ is derived from the transmembrane APP by proteolytic processing during normal cell metabolism and is secreted into the CSF served as the foundation for Aβ biomarker development. However, mechanisms associated with Aβ generation are not fully known. The most important Aβ isoform is Aβ42 which is a 42 amino-acid long and aggregation-prone protein. Many studies found that the levels of CSF Aβ42 in AD is reduced to approximately half of control levels by using several different enzyme linked immunosorbent assay (ELISA) methods (9,10). In recently study demonstrated that the decrease of Aβ42 concentrations in the CSF was associated with PSEN mutations that cause AD (11). Another study came to the opposite conclusion that mutation carriers had higher CSF Aβ42 levels than non-carriers (12). Low CSF Aβ42 levels reflect the decreased clearance and the increased deposition of Aβ42 in the brain, however, this is not absolutely specific for AD and is also observed in patients with dementia with Lewy bodies.
CSF Aβ40 is another important biomarker in AD. The levels of CSF Aβ40 diminish with increased age (13), and decrease significantly in AD subjects than those with mild cognitive impairment (MCI) (14). But no significant difference was found among AD participants, nondemented controls, and patients with non-AD dementia (15).
Further discovery about other Aβ isoforms found the CSF Aβ17-40/Aβ11-40 ratio significantly higher in patients with CDR-SB ≤1.5 (Cognitive Dementia Rating-Sum of Boxes score) than in controls, may become a novel biomarker to discriminate between them (16). The assessment of Aβ17 may increase the diagnostic performance of blood-based Aβ tests which might be developed into minimally invasive first-step screening tests for people with increased risk for AD (17). These conclusions needed to be confirmed in other larger clinical independent studies.
Aβ oligomers
Exactly as deposited fibrillary Aβ, soluble Aβ oligomers, assemblies ranging from dimers to 24-mers, can also induce the formation of tau neurofibrillary pathology (18,19), although it is still unclear in the literature whether Aβ pathology is responsible for tau pathology in AD. Multiple lines of evidence suggested that Aβ oligomers may be more toxic than fibrillar Aβ aggregates (20,21). Accumulating evidences from studies of transgenic mouse models demonstrated that AD brain-derived and synthetically prepared Aβ oligomers can cause early synaptic toxicity (22), long-term potentiation (LTP) deficits, tau phosphorylation and neurofibrillary tangles (23). Specific cognitive deficits express in animals (Zebrafish Embryo) injected with Aβ peptide correlated with Aβ peptide accumulation and memory impairment in rodent, as suggested by Nery et al. (24). In the recently study shows a significant 3-to-5-fold increase in Aβ oligomers in human AD CSF compared with comparably aged controls (25). Further, oligomer levels increase as MMSE score drops (25). Of course, with a very low CSF level, probably less than 1% of total Aβ levels, it is very difficult to quantify the CSF level of Aβ oligomers in a reliable manner.
However, Santos et al. (26) thought there was a negative correlation between the levels of Aβ oligomers and cognitive status measured by the Mini-Mental Status Exam score (r=−0.65; P=0.013) in AD patients. The detection of Aβ-oligomers using flow cytometry analysis suggests a potential use for assessing disease stage in AD individuals. Another study discovered no difference the CSF level of Aβ oligomers between AD and control groups, indicating levels of small oligomers unsuitable as biomarkers for AD (27). The reason may be the levels of Aβ oligomers elevating in human and mouse brains are very low or absent in CSF (28). The increased levels of Aβ oligomers are positive association with age and levels of total tau in cognitively normal older adults, and elevated levels of both oligomers (Aβ*56 and Aβ trimers) were found in cognitively normal subjects indicating impending AD (29). It is difficult to measure minute amounts of Aβ oligomers in CSF samples, thus, reliable methods to access Aβ oligomers are urgently needed. The onset and progression of AD associated specific technique to detect Aβ oligomers would be a valuable tool in AD diagnostics.
Plasma Aβ
Since plasma and serum is noninvasive and more easily available than CSF from lumbar puncture, to find reliable plasma and serum biomarkers for AD is with great promise. With the development of measurement methodology and efforts from generation to generation, several novel blood biomarkers have been proposed, although verification and validation in independent studies remains to be clearly further established.
Aβ as a driving force in AD is very important in the pathogenesis of senile plaques, therefore plasma Aβ suffered from widespread concerns and has been studied extensively in relation to AD diagnosis and risk. However, studies of plasma Aβ have been contradictory and some cross-sectional analyses have reported higher Aβ1–42 levels (30), higher Aβ1–40 levels (30,31), while others have found lower levels of Aβ1–42 (32,33) as well as no significant differences between AD patients and controls. Some studies found also that a low ratio of Aβ42 to Aβ40 (AβR) (32,33) predicted future AD while others report an elevated ratio or no associations in the group with incipient AD compared with subjects that didn’t develop AD. Some cohort studies found higher plasma concentrations of Aβ1-40 (34,35), higher plasma concentrations of Aβ1–42 (34,36), high AβR (30) or low AβR (35-37) were associated with risk for AD. But other cohort studies suggested lower plasma Aβ1-40 levels (38), lower plasma Aβ1–42 levels predicted incident AD and were not significantly associated with AD incidence. In one study, a decrease in Aβ1–40 in early stages and an increase in AβR were associated with a worse cognitive performance among AD patients (39). Another study found that high plasma concentrations of Aβ42 was associated with a faster rate of cognitive decline among AD patients (40). Matsuoka et al. (41) got a tendentious conclusion that AβR is more strongly important to the pathophysiologic process of AD than absolute levels of the peptides in genetically susceptible populations. However, it has been very hard to reproduce above findings in independent studies (42), and this pre-eminent unsolved medical problem remains to explore.
BACE1
Chemical property of BACE1 is membrane-associated aspartic protease 2. Aβ peptide is produced by proteolytic cleavage of APP by two different enzymes, β-secretase and γ-secretase, one of which is the protein encoded by the BACE1 gene. The encoded protein, a member of the peptidase A1 protein family, is a type I integral membrane glycoprotein and aspartic protease that is found mainly in the Golgi, and its official full name is β-site APP cleaving enzyme-1.
Unlikely CSF Tau and Aβ, CSF BACE1 and soluble amyloid precursor proteins α and β are without consistent patterns in AD participants. Numerous researchers have investigated the levels of CSF BACE1 activity in patients with MCI and AD compared with age-matched controls, but the results are not univocal. Two studies found that patients with AD had increased Plasma BACE1 activity (43) and CSF BACE1 activity (44) compared with non-demented controls. Similarly, significant elevation of BACE1 levels and activity in CSF in patients with MCI due to AD compared with controls (45), and a higher elevated BACE1 activity in patients with MCI but not with AD when comparing with health controls (46) were demonstrated, respectively. Mulder et al. (47) found that no correlation between BACE1 activity and Aβ42, and subsequent large study suggested no significant differences in BACE1 activity between AD patients and controls (48).
However, when patients with a pathologic profile of the core AD biomarkers were compared with controls with a normal biomarker pattern, a significant elevation of BACE1 activity was found in the patient group. The MCI patients contributed the most to this elevation. When the AD patients were stratified into mild and moderate-severe AD, an increased BACE1 activity could be seen in the group with mild AD compared the more advanced AD patients and controls. These studies demonstrate that the levels or activity of BACE1 may be mildly elevated in the early stages of AD, which could become a useful biomarker to predict incipient AD.
sAPPα/sAPPβ
Cleavage of APP by α-secretase generates soluble N-terminal fragments of 100-130 kDa (sAPPα) and an 83 amino acid, membrane associated C-terminal fragment, which consists of the C-terminal portion of Aβ, and APP cytosolic domain. The alternative, amyloidogenic pathway involves cleavage of APP by β-secretase at the amino terminus of Aβ to release the soluble N-terminal fragment, sAPPβ, followed by processing of the remaining 99 amino acid membrane tethered C-terminal fragment by γ-secretase to release Aβ.
The CSF concentration of sAPPα and sAPPβ correlates very well with AD patients as well as controls (45). Patients with AD had increased sAPPβ and sAPPα compared with non-demented controls (43). However, no difference was showed in the levels of these biomarkers between AD patients and controls in other studies (45,48). The higher concentration of sAPPβ was found in MCI patients compared with controls (49), and MCI patients with incipient AD had higher levels of sAPPβ than patients without (50). However, Hertze et al. (51) found no differences in sAPP levels in MCI patients that upon follow up advanced AD compared with stable MCIs or patients with other dementias. Compared patients with MCI or dementia that had a pathologic core CSF AD biomarker profile with controls with a normal profile, several studies found that the former group had significant elevation of sAPPα and sAPPβ levels, but there were large overlaps between the groups (52,53). We have mountains of work to study the diagnosis value of sAPPα and sAPPβ.
According to the study by Lewczuk et al. (52), there are two well-known and one possible risk factors for AD, the effects of age, the presence of the APOEε4 allele and the integrity of the blood-CSF barrier, which may be associated with the CSF concentrations of sAPPα and sAPPβ. To further unravel the story of this newly identified, larger sample sizes, better measurement and study designs and more case-control studies are needed.
Total tau (T-tau) and phosphorylated tau (P-tau) protein
In addition to presenting morphologically with senile plaques, primarily made of extracellular Aβ deposits, AD suffers also from neurofibrillary tangles, another validated histopathological change, which consist of intracellular aggregates of hyperphosphorylated tau protein. A microtubule associated protein, Tau participates in the microtubule stabilization and organization system which regulates cellular morphogenesis, cytoskeleton functionality and axonal transport. It is comprehensible that high levels of tau in CSF of AD patients can reflect the intensity of neuronal damage and degeneration in the brain.
All of several isoforms of the tau protein in CSF contain a large number of serine and threonine phosphorylation sites (54,55), which makes hyperphosphorylation possible. The most commonly used measurement method for T-tau and P-tau is the ELISA, for T-tau based on monoclonal antibodies that detect all isoforms of tau independently of phosphorylation state and for P-tau using antibodies that are specific for phosphorylation at either threonine181 (P-Tau181) or threonine231 (P-Tau231). P-tau231 are useful for distinguishing AD and frontotemporal dementia, and p-tau181 can enhance classification between AD and dementia with Lewy bodies (56). Numerous studies have used this assay, and consistently report a prominent increase of CSF T-tau and P-tau in AD against control levels (9). The immunoassays used to analyze tau levels in blood have also been established (56). Tau is rapidly released into the bloodstream after hypoxic brain injury following cardiac arrest, but effectively (within 24 hours) cleared in patients with good neurological outcome (57). In a recent study supporting this view found that plasma tau make no difference between AD and normal control group (31). Another study found significantly higher plasma tau levels in patients with MCI or early AD compared with health elders (58). In view of tau reflecting intracellular impairment in neurocyte, it is necessary to further study to tau proteins including varied forms or locations.
Combination of tau and Aβ as biomarkers
The diagnostic accuracy for the combination of decreased Aβ42 and increased T-tau and P-tau has a higher sensitivity and specificity of more than 85% in differentiating AD from healthy controls than for any biomarker alone (59,60). The addition of P-tau to Aβ42 and T-tau further increases specificity for AD (60). Tau and Aβ as Biomarkers are two main types of aberrant proteinaceous aggregates found associated to AD. Along with the development of the AD biomarkers, specifically the Aβ/tau ratio, studies may easier identify or distinguish patients at higher risk for cognitive changes from healthy controls. Xie et al. (61) gave evidence in his clinical trial that Preoperative CSF Aβ/tau ratio is associated with neuropathogenesis of postoperative cognitive dysfunction. In a recently study, Xie et al. (62) emphasized once again lower CSF Aβ/Tau ratio could be associated with postoperative delirium or postoperative cognitive change. Notably, this combination of CSF tau and Aβ biomarker changes may predict the conversion from mild cognitive impairment (MCI) subjects to AD patients. However, it is essential to standardize the measurement methodology for CSF Aβ42 and tau concentrations before the utility of combination for diagnosis of AD is established. For example, a multiparameter assay for simultaneous quantification of these CSF biomarkers is based on the LuminexTM xMAP technology whose diagnostic performance has been good (63).
MicroRNA (miRNA)
The miRNAs are small double-stranded, non-coding RNA molecules of 21~25 nucleotides that mainly bind to 3’untranslated region (3’UTR) of target mRNAs and fine-tune gene expression at posttranscriptional level. The imperfect sequence complementarity between a miRNA and its target mRNA enables a single miRNA to regulate many mRNAs (64). Kong et al. (65) found the dysregulation of miRNAs could interrupt the metabolism of amino acids in the brain so as to accelerate the pathological process of AD by investigating miRNA expression profile of adult-onset drosophila AD model.
Accumulating data focused on the role of miRNA in APP and Aβ metabolism. The level of miR-107, regulating the expression of BACE1, is significantly lower in AD (66). Another study identified 11 microRNAs, including miR-107 and miR-26b, may be involved in cholesterol induced AD-like pathology (67). Liu et al. (68) found that the levels of miR-135a, repressing expression and activity of BACE-1, miR-200b and -429, suppressing expression of APP, in the serum or CSF of AD groups were significantly lower than that of control groups. The decreased miR-384 expression was showed in CSF and serum of Patients with MCI and dementia of Alzheimer’s type compared with the controls (69). The levels of miR-146a were significantly lower than age-matched nondemented control subjects in CSF of AD patients (70). Hébert et al. (71) found that expression levels of miRNA-29a/b-1 cluster are reduced in the cortexes of sporadic AD patients, associated with a 2- to 5-fold increase in the level of BACE1 protein. Several studies found some miRNAs such as, Let-7 (72), miR-146a (70) and miR-132 (73), miR-29a/b (74,75) could lead to the spread of CNS damage by inducing neurocyte inflammation or apoptosis (Table 1). Other instances the roles of miRNA in AD include miR-124 regulating the APP mRNA alternative splicing, MiR-101, -520c, -147, -16, -20a, -644 and - 153 targeting 3’UTR of APP mRNA, MiR-107, -29a/b1/c, -9, -328 and -298 regulating the expression of BACE1, and miR-384 suppressing the mRNA and protein expression of both APP and BACE-1.
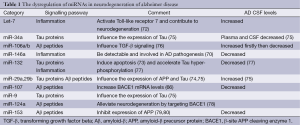
Full table
In conclusion, such alterations in miRNA levels would play an important part in the diagnosis and/or targeted treatment of AD in human patients. In the future more robust and invasion-free diagnostic methodology in complement with traditional methods involving collection of CSF, plasma or serum will be published.
Apolipoprotein E (APOE)
Convincing evidence suggests that an increase in total Aβ production, an increase in the ratio of Aβ42 to Aβ40, or generation of a mutant form of Aβ with greater amyloidogenic propensity are the main mechanisms for the rare early-onset forms of autosomal-dominant familial AD, but these are probably not the major pathogenic mechanisms underlying the more common late-onset AD. APOE genotype has been reported as the strongest genetic risk factor for late-onset AD, with the ε4 allele being an AD risk factor and the ε2 allele being protective. Many studies found the APOE is able to influence the transport and metabolism of the Aβ, and the interaction of APOE with Aβ plays an important role in AD pathogenesis. However, Zimmermann et al. found the opposite conclusion by measure plasma levels of Aβ proteins in young healthy persons (81). One study in vitro demonstrated that apoE can facilitate the proteolytic degradation of Aβ in the brain (82). As is well known that ε4 allele of ApoE protein is less efficient in proteolysis of Aβ, thus increases the brain amyloid deposition in APOE ε4 allele carriers (83). Therefore, MCI subjects with the presence of APOE ε4 allele (ε4+ individuals) have higher CSF lipid-depleted Aβ (with great propensity for transformation to soluble Aβ oligomers) levels than ε4- individuals (84). While human apoE is complexed with Aβ, the clearance of Aβ across blood-brain barrieris actually decreased compared to that of free Aβ (85).
Considering the strong effect of apoE alleles on the risk of developing AD, many studies have been conducted worldwide to investigate whether apoE protein levels are connected to AD. But, previous studies about CSF apoE levels in humans have yielded controversial results. One recent study found CSF ApoE levels weren’t associated with progression of AD (86). Maybe the concentrations of CSF apoE are not dramaticlly different between cognitively normal subjects and those with mild or moderate dementia. So researchers need more sensitive instruments or better innovation to differentiate AD cases from controls.
Other biomarkers
The conception of other pathways that may be associated with AD pathogenesis are pointed, such as the innate immune system, cholesterol metabolism and so on, although quantity of promising outcomes are obtained by the classical amyloid cascade hypothesis.
Some studies found CSF levels of YKL-40, a microglia (87) and astrocyte-derived (88) marker of neuroinflammation, were higher in preclinical and prodromal AD patients (89) and were tightly correlated with T-tau and P-tau levels (88,89). One study has shown microglial engagement in amyloid plaques with the capacity to prevent or reduce the formation of amyloid plaques in transgenic mice (90). In addition, microglial induced inflammatory processes are significantly associated with axonal degeneration and neuronal deficit in AD (91). Hence, the inflammation in this neurodegenerative disease is a double-edged sword, and it is more important to direct and instruct the inflammatory machinery than to suppress it.
Increasing evidence demonstrate that insulin resistance (IR) plays a critical role in Aβ production and accumulation (92,93), the Tau pathology (94), impaired synaptic transmission (95) and neuronal degeneration. IR could enhance β- and γ-secretase activity inducing Aβ production (93). One study demonstrated the utility of evaluating indices of IR and their consequences, i.e. oxidative stress, neuro-inflammation, and reduced neuronal plasticity combined with P-Tau and Aβ in CSF-based multiplex assays (96). IR can in the brain contribute to Aβ and tau pathology by means of oxidative stress and inflammation. In turn, Aβ accumulation can enhance IR through Aβ-mediated inflammation and oxidative stress. Additionally, hyperinsulinemia and hyperglycemia caused by IR accelerate also the formation of neuropathologic changes (97). Preclinical and clinical studies have supported that insulin could be beneficial to the treatment of AD. Thus, the insulin level may be a novel biomarker in AD.
In a pilot study, Leoni et al. (98) found similar percentage and more sensitive of AD patients with increased levels of 24S-hydroxycholesterol than that of T-tau and P-tau demonstrated that 24OHC might be a valuable tool to boost the diagnostic performance of AD. More interesting novel biomarkers are proposed, such as Visinin-like protein-1 (99) which can serve as a good candidate for dynamic biomarker of AD and may play a role in the AD pathophysiology, Hydrogen peroxide-inducible clone 5 and paxillin (100) that make a difference in AD compared with controls, and glycogen synthase kinase 3β (101) coexisting with severe brain inflammation. Matrix metalloproteinases (MMPs) play multiple roles in the pathogenesis of AD (102), with MMP-2 being a protective factor, MMP-9 and MMP-3 being potential neurotoxic enzymes. The levels of plasma TNF-α converting enzyme activity correlated conspicuously and negatively with cognition in subjects with MCI and patients with AD (103). However, the majority of them are promising hypothesis-driven biomarkers, further studies are needed to support the role of these findings.
The potential uses for body fluid biomarkers in clinical trials
More and more potential uses for body fluid biomarkers in clinical trials were discovered with the development detection techniques. Besides in favor of early diagnosis, those biomarkers may be made full use of assessing disease progression, developing treatments, monitoring treatment effects. In an attempt to higher accuracy of early diagnosis, better prognosis and more safe and effective treatment effects, we should keep up striving.
Improved early diagnosis
Currently, to make a definite diagnosis of AD can only be based upon postmortem analysis of the brain. Early diagnosis for AD is a great limitation because of the paucity of specific symptoms in MCI cases. It is crucial and effective to get an early diagnosis biomarker to initiate or interfere with an adequate treatment in the early stages of the disorder. A multitude of studies have got the consistent findings that core CSF biomarkers, such as the Aβ42, T-tau and P-tau, can make a difference in preclinical or prodromal AD (104-106). The drop of CSF Aβ42 protein levels comes before the other CSF markers changes in preclinical AD (105). Gustafson et al. (107) have demonstrated that lowering of Aβ42 in CSF is a very early change in sporadic AD. Interesting, a previous study found tau pathology priors to amyloid plaque pathology (108). Further studies are needed to validate utility of AD biomarkers as a precise tool to differentiate patients with control participants in early phase of AD, since there may be a controversy for the choice of the appropriate biomarker.
Following scientists trend to have access to novel biomarkers so as to increase the accuracy of the clinical diagnosis of AD. Serum levels of Aβ peptides may be a valuable diagnosis marker (109), and the thioredoxin super family correlated proteins could involve in the pathogenesis of early AD as hopeful early diagnostic biomarkers (110). However, the well-known reliable predictive biomarkers, brain imaging and CSF measurement are expensive and invasive procedures respectively, and several candidate blood biomarkers with insufficiently sensitive or specific aren’t fully responsible for diagnosing early AD. Under the circumstances, the concept of “biomarker panels” is put forward to get over the great present challenge.
Assessed disease progression
Biomarkers may be used to assess disease progression to further stage early, middle, and advance AD pathogenesis event so as to guide clinical treatment. Many studies found biomarker magnitude enhance constantly with conversion from incipient stage to advanced AD. Accumulating evidence from both genetic at-risk individuals and clinically normal older cohorts suggests that the pathophysiological process of AD begins 1 to 2 decades before the emergence of the clinical manifestation of dementia (111). In line with the preclinical period or prodromal stage refers to a progression that is progressing gradually towards cognitive deficit and behavioural impairment of AD. In consequence, the pathologic changes paid close attention to in early stage of AD contribute to the development of therapeutic interventions. Findings from Blennow et al. (112) suggested CSF levels of T-tau increased triple changes than control participants in developed AD.
It is clear, however, that some older individuals with the pathophysiological process of AD may not become symptomatic during their whole lifetime. Thus, it is critical to better define a kind of biomarker that best predicts progression from the preclinical to the clinical stages of MCI and AD dementia so that the sufferers can benefit from early biomarker profile intervention.
Although limitations in view of the current lack of validated peripheral biomarkers, changes in peripheral biomarkers may be useful to differ from different stages of AD. A combination of central and peripheral biomarkers could be developed to help to stage AD, and the role of biomarkers in improving the accuracy of this prediction awaits results of future studies.
Developed treatments
Neurologist and psychiatrist have hungered for potential disease modifying effects, a novel AD therapy, which the scientists are exploring strenuously to prevent or attenuate the progression of AD effectively.
Since Aβ is thought to be a central pathogenic culprit, the disease-modifying therapy is being established, especially inhibitors of Aβ-producing proteases and Aβ immunotherapy which are now considered as prophylaxis for patients with MCI. In a cell culture model study, six novel compounds reducing expression of APP resulting in decreased Aβ-levels provide valuable information for the development of Aβ-modifying therapies for AD (113). Additionally, therapeutic intervention used an anti-Aβ-oligomers antibody benefits for neuronal protection by Aβ aggregation pathway in AD (114). BACE1 inhibitors, as an indirect depressors of Aβ by lowing or reducing CSF Aβ levels, progressed into Phase 1 clinical trials in humans (115). Another novel potential biomarker associated with amyloid-modifying therapies is anti-Aβ autoantibodies (116). Lemere et al. (117) suggested the shorter Aβ immunogens might induce the higher titers of antibodies that was able to clear cerebral Aβ and they could serve as a safer vaccine to prevent and treat AD patients optimistically. Of course, blood biomarker tests may be useful in clinical trials of treatment for AD. But, the findings are still under debate due to obvious advantages or disadvantages.
Current approaches including anti-Aβ disease-modifying drugs, cholinesterase inhibitors and N-methyl-d-aspartate receptor antagonists, are symptomatic treatments for AD, and do not cut off disease progression. Both laboratory data and recent disappointing clinical trial results raise the possibility that therapeutic interventions applied earlier in the course of AD would be more probable to achieve disease modification. In other words, Aβ-modifying therapies may have limited effect if pathophysiological process of AD has begun. One recent clinical trial regarding late-stage drug development for AD shown that 95% drug development has failed to demonstrate clinical effects, even in the setting of biomarker or autopsy evidence of decreased Aβ levels (118). Opinions from secondary prevention studies suggest therapeutic interventions against asymptomatic individuals or those with subtle evidence of impairment due to AD can postpone the onset of advanced clinical manifestation. So, before significant cognitive impairment or memory loss, in the “presymptomatic” or “preclinical” stages of AD, patients would be optimally treated. Many researchers in the field suggest that a possible strategy to achieve success is earlier intervention. To delay or prevent later neurodegeneration and eventual dementia, further preclinical studies are needed to find an appropriate treatment.
What appears to be well understood is that AD is a heterogeneous disorder, at both the clinical and neuropathological levels (119). As mentioned above, the effects of disease modifying drugs will differ between subgroups of AD patients in the case of degree of plaque and tangle pathology. It is sufficient to consider desirable to stratify the patient cohort in AD clinical trials based on disease progression, which may show the better effect of anti-Aβ disease-modifying drugs in lower levels of CSF Aβ42 subjects than a normal subgroup.
Monitored treatment effects
Biomarkers well known as “theragnostic markers” are used to identify and monitor the biochemical effect of drugs (106). Although disease modifying therapies can delay progression, improve the lives of patients and prolong their period of relatively good, non-disabled life, great importance should be attached to off-target or adverse effects of treatment. For example, both active and passive immunization strategies have been investigated to increase the clearance of Aβ. However, meningoencephalitis was observed in a subset of cases with mild to moderate AD in the aggregated Aβ42 with a QS-21 adjuvant (AN1792) trial on active Aβ immunotherapy (120), leading to development of AN1792 discontinuing. Passive immunization strategies may cause local microglial activation, of which side effects including microhemorrhage and vasogenic edema also reported were associated with patients particularly carrying the ApoE e4 allele.
Of course, much attention should be paid to positive and available biochemical effect of drugs. For instance, cholinesterase inhibitors are drugs expected to an early improvement in cognitive function. Instead of an early effect on symptoms, disease-modifying drugs will lead to a less remarkable decline in cognitive function over years by retarding or ultimately even preventing the onset of cognitive impairment and dementia. Two studies found that infusion of solanezumab, an anti-β-amyloid antibody, was generally well tolerated in patients with mild-to-moderate AD (121,122). Therefore, it is meaningful to monitor this medicine treatment effects continually.
Challenges in validation and application of AD biomarkers to clinical practice
Although the number of AD biomarkers in discovery is enormous, those in clinical application are substantially low. The imperfect biomarkers may have a limit effect on clinical trials or practices. The overlap in pathology suggested a small proportion of individuals who are classified as stage 0 are probably experiencing early AD processes that detectable in advanced stage. Recent longitudinal data suggest that each year, approximately 3% of clinically normal individuals cross the threshold from “amyloid-negative” to “amyloid-positive” on PET imaging (123). The better biomarkers can stratify AD patients more distinctly, which can lead to more effective treatment, and simultaneously avoid unwanted misdiagnoses.
Since the most of AD biomarker chemical properties are proteins, it’s comprehensible that Preanalytical variations are also important factors including sample collection conditions, timing of sample processing and sample storage conditions. Besides a poor study design that does not address the specific research questions, other potential important factors in regard to study design contain heterogeneity in the inclusion of patients and controls, a lack of prospective studies or validation cohorts, insufficient sample size, and a paucity of confirmation of findings with different techniques.
Another challenge is the scarcity of assay standardization, especially the stringency of the statistical analyses. Different researchers employed different experimental techniques and methods, and gave different absolute concentrations of the protein, which led younger generation to state the difficulties in the discovery of candidate biomarkers. Combination of strict statistical criteria with biological criteria might be expected to help clinicians to focus on novel biomarkers with the most potential for validation.
Although plasma sampling is much easier, with fewer side effects, and is readily applied in primary care centers, two problems exist with limitation of utility of the plasma markers. One problem is that CSF undergoes substantial dilution as it passages into the bloodstream due to the blood-brain barrier, and this raises challenges in trying to detect brain-specific biomarkers in plasma-their concentration is likely to be orders of magnitude lower than in the brain or CSF. Another problem is that changes in the blood reflect more from the systemic effects rather than specific brain changes in AD, which bring about the lower specificity.
The low specificity and sensitivity of current biomarkers hamper the application of them in clinical practice. Some validated biomarkers are not specific for AD, for example, P-tau and T-tau can also over express in normal aging, other chronic brain injury, amyotrophic lateral sclerosis (124,125), Creutzfeldt-Jakob disease (126), Parkinson’s disease (127), epileptic seizures (128) and even breast cancer (129) and so on; similarly, the lower Aβ levels can also be detectable in other dementias and cardiac arrest survivors (130). Unfriendly physiopathologic overlaps between vascular dementia and AD create the limitation of the study design even with neuroimaging (131). It is impossible to exclude all the subjects with vascular brain injury, so most of the AD group also contains patients with vascular abnormalities.
What is the ideal biomarker in AD?
The ideal biomarker in AD should present in patients with AD and absent in healthy individuals or those with other pathological disorders, and levels would increase or decrease when the disease worsens or improves, respectively. Some other desired properties of molecular biomarkers for AD should be also considered in addition to this theoretical and simple scenario. In brief, the marker must have a scientific rationale, the marker must be measurable and reproducible, the marker must be specific for AD and the biomarker should change with disease progression in longitudinal observational studies.
The ideal biomarker should give clinicians no other alternative than to rely on clinical diagnosis by exclusion. The category of biomarkers for diagnosis should be strongly associated with onset of AD, and suggest diagnoses with no false positive or negative results presymptomatically. With the development of AD pathophysiological processes, the levels of disease activity biomarkers should have obvious changes over time, and with respect to treatment-response biomarkers, to monitor or capture absolutely the effect of treatment would be crucial (Table 2).
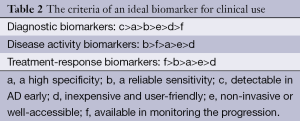
Full table
Future perspectives of biomarker studies
The use of criteria for sample collection and storage conditions as well as timing of sample processing will be crucial to scientific researches regarding discovery and validation of biomarkers in large cohorts of patients with AD.
AD is a heterogeneous disease, with many different treatments giving rise to numerous debates how to give the proper treatment to the right patient. So, it is essential that treatment-response biomarkers need to identify accurately individuals with a high risk of adverse effects as well as predict precisely the responder or nonresponder, and tolerated or untolerated status of patients. Nevertheless, consistent standards of the definitions of treatment response or not have not yet reached. In addition, a better design in treatment-response study is needed, since studies do not allow for difference between natural progression and true treatment response.
Lumbar puncture employed in the collection of CSF is an invasive procedure that limits repeated collection and its use in clinical practice can be in trouble. Well accessible body fluids (including peripheral blood, urine, saliva) less invasively collected than CSF, which seems be in favour of the use of blood-borne biomarkers or biomarkers derived other body fluids in AD clinical practice. However, the dilution of the concentration caused by the effect of blood-brain barrier restricts the process of clinical trials. Further investigation is needed to verify utilities of other body fluid biomarkers excluding CSF.
Combination of multiple biomarker modalities including various body fluids biomarkers, both structural (CT/MRI) and functional (SPECT/PET) brain imaging will improve the diagnostic accuracy as compared with the use of one biomarker alone. Vemuri et al. found that the combination of positive CSF biomarkers and MRI with clinical diagnosis, providing complementary information, increased the chance to predict the conversion from amnestic MCI to AD better than either source of data alone (132). With a high sensitivity and specificity to identify AD patients from controls attributed to the combined data on plasma TNF-α receptors signaling proteins, Aβ and the APOEε4 allele (133). One study about the combination of neuropsychological and biological markers in AD suggested that this biomarker panel could be used as a new tool to track disease progression in early AD as well as the response to disease-modifying drugs (134). To further validate the improved diagnostic and treatment-response value of combining multiple biomarkers need more multicenter studies.
Conclusions
The predecessor have implemented enormous amounts of studies about CSF AD biomarkers and procured plentiful and substantial progeny. In addition, novel biomarkers are recommended as the noninvasive markers playing an important role in the future studies in AD. We have unprecedented possibilities to be able to stratify our patients, improve diagnosis early, monitor progression and optimize treatment with the development of body fluid biomarkers. However, the mechanism of onset of AD has been unknown, to capture the conversion from undementia to dementia and the most appropriate or ideal biomarkers will be a strongly challenge in further studies.
Acknowledgements
Funding: This work was supported by grants from the National Natural Science Foundation of China (81471309, 81171209), the Shandong Provincial Outstanding Medical Academic Professional Program, Qingdao Key Health Discipline Development Fund, Qingdao Outstanding Health Professional Development Fund, and Shandong Provincial Collaborative Innovation Center for Neurodegenerative Disorders.
Disclosure: The authors declare no conflict of interest.
References
- Li Y, Tan MS, Jiang T, et al. Microglia in Alzheimer's disease. Biomed Res Int 2014;2014:437483.
- Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther 2001;69:89-95. [PubMed]
- Hardy J, Selkoe DJ. The amyloid hypothesis of Alzheimer's disease: progress and problems on the road to therapeutics. Science 2002;297:353-6. [PubMed]
- Mayeux R, Stern Y. Epidemiology of Alzheimer disease. Cold Spring Harb Perspect Med 2012;2. [PubMed]
- Garcia-Alloza M, Subramanian M, Thyssen D, et al. Existing plaques and neuritic abnormalities in APP:PS1 mice are not affected by administration of the gamma-secretase inhibitor LY-411575. Mol Neurodegener 2009;4:19. [PubMed]
- Levites Y, Das P, Price RW, et al. Anti-Abeta42- and anti-Abeta40-specific mAbs attenuate amyloid deposition in an Alzheimer disease mouse model. J Clin Invest 2006;116:193-201. [PubMed]
- Das P, Murphy MP, Younkin LH, et al. Reduced effectiveness of Abeta1-42 immunization in APP transgenic mice with significant amyloid deposition. Neurobiol Aging 2001;22:721-7. [PubMed]
- Lista S, Faltraco F, Prvulovic D, et al. Blood and plasma-based proteomic biomarker research in Alzheimer's disease. Prog Neurobiol 2013;101-102:1-17. [PubMed]
- Blennow K. Cerebrospinal fluid protein biomarkers for Alzheimer's disease. NeuroRx 2004;1:213-25. [PubMed]
- Sunderland T, Linker G, Mirza N, et al. Decreased beta-amyloid1-42 and increased tau levels in cerebrospinal fluid of patients with Alzheimer disease. JAMA 2003;289:2094-103. [PubMed]
- Potter R, Patterson BW, Elbert DL, et al. Increased in vivo amyloid-beta42 production, exchange, and loss in presenilin mutation carriers. Sci Transl Med 2013;5:189ra77.
- Reiman EM, Quiroz YT, Fleisher AS, et al. Brain imaging and fluid biomarker analysis in young adults at genetic risk for autosomal dominant Alzheimer's disease in the presenilin 1 E280A kindred: a case-control study. Lancet Neurol 2012;11:1048-56. [PubMed]
- Dobrowolska JA, Kasten T, Huang Y, et al. Diurnal patterns of soluble amyloid precursor protein metabolites in the human central nervous system. PLoS One 2014;9:e89998. [PubMed]
- Mizoi M, Yoshida M, Saiki R, et al. Distinction between mild cognitive impairment and Alzheimer's disease by CSF amyloid beta40 and beta42, and protein-conjugated acrolein. Clin Chim Acta 2014;430:150-5. [PubMed]
- Shea YF, Chu LW, Zhou L, et al. Cerebrospinal fluid biomarkers of Alzheimer's disease in Chinese patients: a pilot study. Am J Alzheimers Dis Other Demen 2013;28:769-75. [PubMed]
- Abraham JD, Prome S, Salvetat N, et al. Cerebrospinal Abeta11-x and 17-x levels as indicators of mild cognitive impairment and patients' stratification in Alzheimer's disease. Transl Psychiatry 2013;3:e281. [PubMed]
- Pérez-Grijalba V, Pesini P, Allué JA, et al. Aβ 1-17 is a major amyloid-β fragment isoform in cerebrospinal fluid and blood with possible diagnostic value in Alzheimer's disease. J Alzheimers Dis 2015;43:47-56. [PubMed]
- Bolmont T, Clavaguera F, Meyer-Luehmann M, et al. Induction of tau pathology by intracerebral infusion of amyloid-beta -containing brain extract and by amyloid-beta deposition in APP x Tau transgenic mice. Am J Pathol 2007;171:2012-20. [PubMed]
- Oddo S, Caccamo A, Tran L, et al. Temporal profile of amyloid-beta (Abeta) oligomerization in an in vivo model of Alzheimer disease. A link between Abeta and tau pathology. J Biol Chem 2006;281:1599-604. [PubMed]
- Tomic JL, Pensalfini A, Head E, et al. Soluble fibrillar oligomer levels are elevated in Alzheimer's disease brain and correlate with cognitive dysfunction. Neurobiol Dis 2009;35:352-8. [PubMed]
- Koffie RM, Hashimoto T, Tai HC, et al. Apolipoprotein E4 effects in Alzheimer's disease are mediated by synaptotoxic oligomeric amyloid-beta. Brain 2012;135:2155-68. [PubMed]
- Selkoe DJ. Alzheimer's disease is a synaptic failure. Science 2002;298:789-91. [PubMed]
- Sakono M, Zako T. Amyloid oligomers: formation and toxicity of Abeta oligomers. FEBS J 2010;277:1348-58. [PubMed]
- Nery LR, Eltz NS, Hackman C, et al. Brain intraventricular injection of amyloid-beta in zebrafish embryo impairs cognition and increases tau phosphorylation, effects reversed by lithium. PLoS One 2014;9:e105862. [PubMed]
- Savage MJ, Kalinina J, Wolfe A, et al. A sensitive aβ oligomer assay discriminates Alzheimer's and aged control cerebrospinal fluid. J Neurosci 2014;34:2884-97. [PubMed]
- Santos AN, Ewers M, Minthon L, et al. Amyloid-β oligomers in cerebrospinal fluid are associated with cognitive decline in patients with Alzheimer's disease. J Alzheimers Dis 2012;29:171-6. [PubMed]
- Bruggink KA, Jongbloed W, Biemans EA, et al. Amyloid-β oligomer detection by ELISA in cerebrospinal fluid and brain tissue. Anal Biochem 2013;433:112-20. [PubMed]
- Yang T, Hong S, O'Malley T, et al. New ELISAs with high specificity for soluble oligomers of amyloid β-protein detect natural Aβ oligomers in human brain but not CSF. Alzheimers Dement 2013;9:99-112. [PubMed]
- Handoko M, Grant M, Kuskowski M, et al. Correlation of specific amyloid-β oligomers with tau in cerebrospinal fluid from cognitively normal older adults. JAMA Neurol 2013;70:594-9. [PubMed]
- Mayeux R, Honig LS, Tang MX, et al. Plasma A[beta]40 and A[beta]42 and Alzheimer's disease: relation to age, mortality, and risk. Neurology 2003;61:1185-90. [PubMed]
- Wang T, Xiao S, Liu Y, et al. The efficacy of plasma biomarkers in early diagnosis of Alzheimer's disease. Int J Geriatr Psychiatry 2014;29:713-9. [PubMed]
- Lui JK, Laws SM, Li QX, et al. Plasma amyloid-beta as a biomarker in Alzheimer's disease: the AIBL study of aging. J Alzheimers Dis 2010;20:1233-42. [PubMed]
- Lewczuk P, Kornhuber J, Vanmechelen E, et al. Amyloid beta peptides in plasma in early diagnosis of Alzheimer's disease: A multicenter study with multiplexing. Exp Neurol 2010;223:366-70. [PubMed]
- Cosentino SA, Stern Y, Sokolov E, et al. Plasma ss-amyloid and cognitive decline. Arch Neurol 2010;67:1485-90. [PubMed]
- van Oijen M, Hofman A, Soares HD, et al. Plasma Abeta(1-40) and Abeta(1-42) and the risk of dementia: a prospective case-cohort study. Lancet Neurol 2006;5:655-60. [PubMed]
- Schupf N, Tang MX, Fukuyama H, et al. Peripheral Abeta subspecies as risk biomarkers of Alzheimer's disease. Proc Natl Acad Sci U S A 2008;105:14052-7. [PubMed]
- Yaffe K, Weston A, Graff-Radford NR, et al. Association of plasma beta-amyloid level and cognitive reserve with subsequent cognitive decline. JAMA 2011;305:261-6. [PubMed]
- Sundelöf J, Giedraitis V, Irizarry MC, et al. Plasma beta amyloid and the risk of Alzheimer disease and dementia in elderly men: a prospective, population-based cohort study. Arch Neurol 2008;65:256-63. [PubMed]
- Toledo JB, Vanderstichele H, Figurski M, et al. Factors affecting Aβ plasma levels and their utility as biomarkers in ADNI. Acta Neuropathol 2011;122:401-13. [PubMed]
- Laske C, Sopova K, Gkotsis C, et al. Amyloid-β peptides in plasma and cognitive decline after 1 year follow-up in Alzheimer's disease patients. J Alzheimers Dis 2010;21:1263-9. [PubMed]
- Matsuoka Y, Andrews HF, Becker AG, et al. The relationship of plasma Abeta levels to dementia in aging individuals with Down syndrome. Alzheimer Dis Assoc Disord 2009;23:315-8. [PubMed]
- Björkqvist M, Ohlsson M, Minthon L, et al. Evaluation of a previously suggested plasma biomarker panel to identify Alzheimer's disease. PLoS One 2012;7:e29868. [PubMed]
- Wu G, Sankaranarayanan S, Wong J, et al. Characterization of plasma-secretase (BACE1) activity and soluble amyloid precursor proteins as potential biomarkers for Alzheimer's disease. J Neurosci Res 2012;90:2247-58. [PubMed]
- Verheijen JH, Huisman LG, van Lent N, et al. Detection of a soluble form of BACE-1 in human cerebrospinal fluid by a sensitive activity assay. Clin Chem 2006;52:1168-74. [PubMed]
- Zetterberg H, Andreasson U, Hansson O, et al. Elevated cerebrospinal fluid BACE1 activity in incipient Alzheimer disease. Arch Neurol 2008;65:1102-7. [PubMed]
- Zhong Z, Ewers M, Teipel S, et al. Levels of beta-secretase (BACE1) in cerebrospinal fluid as a predictor of risk in mild cognitive impairment. Arch Gen Psychiatry 2007;64:718-26. [PubMed]
- Mulder SD, van der Flier WM, Verheijen JH, et al. BACE1 activity in cerebrospinal fluid and its relation to markers of AD pathology. J Alzheimers Dis 2010;20:253-60. [PubMed]
- Rosén C, Andreasson U, Mattsson N, et al. Cerebrospinal fluid profiles of amyloid beta-related biomarkers in Alzheimer's disease. Neuromolecular Med 2012;14:65-73. [PubMed]
- Olsson A, Hoglund K, Sjogren M, et al. Measurement of alpha- and beta-secretase cleaved amyloid precursor protein in cerebrospinal fluid from Alzheimer patients. Exp Neurol 2003;183:74-80. [PubMed]
- Perneczky R, Tsolakidou A, Arnold A, et al. CSF soluble amyloid precursor proteins in the diagnosis of incipient Alzheimer disease. Neurology 2011;77:35-8. [PubMed]
- Hertze J, Minthon L, Zetterberg H, et al. Evaluation of CSF biomarkers as predictors of Alzheimer's disease: a clinical follow-up study of 4.7 years. J Alzheimers Dis 2010;21:1119-28. [PubMed]
- Lewczuk P, Popp J, Lelental N, et al. Cerebrospinal fluid soluble amyloid-beta protein precursor as a potential novel biomarkers of Alzheimer's disease. J Alzheimers Dis 2012;28:119-25. [PubMed]
- Gabelle A, Roche S, Geny C, et al. Correlations between soluble alpha/beta forms of amyloid precursor protein and Abeta38, 40, and 42 in human cerebrospinal fluid. Brain Res 2010;1357:175-83. [PubMed]
- Camero S, Benitez MJ, Cuadros R, et al. Thermodynamics of the interaction between Alzheimer's disease related tau protein and DNA. PLoS One 2014;9:e104690. [PubMed]
- Portelius E, Hansson SF, Tran AJ, et al. Characterization of tau in cerebrospinal fluid using mass spectrometry. J Proteome Res 2008;7:2114-20. [PubMed]
- Hampel H, Blennow K, Shaw LM, et al. Total and phosphorylated tau protein as biological markers of Alzheimer's disease. Exp Gerontol 2010;45:30-40. [PubMed]
- Randall J, Mortberg E, Provuncher GK, et al. Tau proteins in serum predict neurological outcome after hypoxic brain injury from cardiac arrest: results of a pilot study. Resuscitation 2013;84:351-6. [PubMed]
- Chiu MJ, Chen YF, Chen TF, et al. Plasma tau as a window to the brain-negative associations with brain volume and memory function in mild cognitive impairment and early Alzheimer's disease. Hum Brain Mapp 2014;35:3132-42. [PubMed]
- Hansson O, Zetterberg H, Buchhave P, et al. Association between CSF biomarkers and incipient Alzheimer's disease in patients with mild cognitive impairment: a follow-up study. Lancet Neurol 2006;5:228-34. [PubMed]
- Verbeek MM, De Jong D, Kremer HP. Brain-specific proteins in cerebrospinal fluid for the diagnosis of neurodegenerative diseases. Ann Clin Biochem 2003;40:25-40. [PubMed]
- Xie Z, McAuliffe S, Swain CA, et al. Cerebrospinal fluid abeta to tau ratio and postoperative cognitive change. Ann Surg 2013;258:364-9. [PubMed]
- Xie Z, Swain CA, Ward SA, et al. Preoperative cerebrospinal fluid beta-Amyloid/Tau ratio and postoperative delirium. Ann Clin Transl Neurol 2014;1:319-28. [PubMed]
- Shaw LM, Vanderstichele H, Knapik-Czajka M, et al. Cerebrospinal fluid biomarker signature in Alzheimer's disease neuroimaging initiative subjects. Ann Neurol 2009;65:403-13. [PubMed]
- Filipowicz W, Bhattacharyya SN, Sonenberg N. Mechanisms of post-transcriptional regulation by microRNAs: are the answers in sight? Nat Rev Genet 2008;9:102-14. [PubMed]
- Kong Y, Wu J, Yuan L. MicroRNA expression analysis of adult-onset Drosophila Alzheimer's disease model. Curr Alzheimer Res 2014;11:882-91. [PubMed]
- Wang WX, Rajeev BW, Stromberg AJ, et al. The expression of microRNA miR-107 decreases early in Alzheimer's disease and may accelerate disease progression through regulation of beta-site amyloid precursor protein-cleaving enzyme 1. J Neurosci 2008;28:1213-23. [PubMed]
- Liu QY, Chang MN, Lei JX, et al. Identification of microRNAs involved in Alzheimer's progression using a rabbit model of the disease. Am J Neurodegener Dis 2014;3:33-44. eCollection 2014.
- Liu CG, Wang JL, Li L, et al. MicroRNA-135a and -200b, potential Biomarkers for Alzheimers disease, regulate beta secretase and amyloid precursor protein. Brain Res 2014;1583:55-64. [PubMed]
- Liu CG, Wang JL, Li L, et al. MicroRNA-384 regulates both amyloid precursor protein and beta-secretase expression and is a potential biomarker for Alzheimer's disease. Int J Mol Med 2014;34:160-6. [PubMed]
- Müller M, Kuiperij HB, Claassen JA, et al. MicroRNAs in Alzheimer's disease: differential expression in hippocampus and cell-free cerebrospinal fluid. Neurobiol Aging 2014;35:152-8. [PubMed]
- Hébert SS, Horré K, Nicolaï L, et al. Loss of microRNA cluster miR-29a/b-1 in sporadic Alzheimer's disease correlates with increased BACE1/beta-secretase expression. Proc Natl Acad Sci U S A 2008;105:6415-20. [PubMed]
- Lehmann SM, Kruger C, Park B, et al. An unconventional role for miRNA: let-7 activates Toll-like receptor 7 and causes neurodegeneration. Nat Neurosci 2012;15:827-35. [PubMed]
- Wong HK, Veremeyko T, Patel N, et al. De-repression of FOXO3a death axis by microRNA-132 and -212 causes neuronal apoptosis in Alzheimer's disease. Hum Mol Genet 2013;22:3077-92. [PubMed]
- Villa C, Ridolfi E, Fenoglio C, et al. Expression of the transcription factor Sp1 and its regulatory hsa-miR-29b in peripheral blood mononuclear cells from patients with Alzheimer's disease. J Alzheimers Dis 2013;35:487-94. [PubMed]
- Kiko T, Nakagawa K, Tsuduki T, et al. MicroRNAs in plasma and cerebrospinal fluid as potential markers for Alzheimer's disease. J Alzheimers Dis 2014;39:253-9. [PubMed]
- Wang H, Liu J, Zong Y, et al. miR-106b aberrantly expressed in a double transgenic mouse model for Alzheimer's disease targets TGF-beta type II receptor. Brain Res 2010;1357:166-74. [PubMed]
- Lau P, Bossers K, Janky R, et al. Alteration of the microRNA network during the progression of Alzheimer's disease. EMBO Mol Med 2013;5:1613-34. [PubMed]
- Fang M, Wang J, Zhang X, et al. The miR-124 regulates the expression of BACE1/beta-secretase correlated with cell death in Alzheimer's disease. Toxicol Lett 2012;209:94-105. [PubMed]
- Long JM, Ray B, Lahiri DK. MicroRNA-153 physiologically inhibits expression of amyloid-beta precursor protein in cultured human fetal brain cells and is dysregulated in a subset of Alzheimer disease patients. J Biol Chem 2012;287:31298-310. [PubMed]
- Liang C, Zhu H, Xu Y, et al. MicroRNA-153 negatively regulates the expression of amyloid precursor protein and amyloid precursor-like protein 2. Brain Res 2012;1455:103-13. [PubMed]
- Zimmermann R, Huber E, Schamber C, et al. Plasma concentrations of the amyloid-beta peptides in young volunteers: the influence of the APOE genotype. J Alzheimers Dis 2014;40:1055-60. [PubMed]
- Jiang Q, Lee CY, Mandrekar S, et al. ApoE promotes the proteolytic degradation of Abeta. Neuron 2008;58:681-93. [PubMed]
- Leduc V, Domenger D, De Beaumont L, et al. Function and comorbidities of apolipoprotein e in Alzheimer's disease. Int J Alzheimers Dis 2011;2011:974361.
- Hanson AJ, Bayer-Carter JL, Green PS, et al. Effect of apolipoprotein E genotype and diet on apolipoprotein E lipidation and amyloid peptides: randomized clinical trial. JAMA Neurol 2013;70:972-80. [PubMed]
- Deane R, Sagare A, Hamm K, et al. apoE isoform-specific disruption of amyloid beta peptide clearance from mouse brain. J Clin Invest 2008;118:4002-13. [PubMed]
- Schmidt C, Gerlach N, Peter C, et al. Cerebrospinal fluid apolipoproteine concentration and progression of Alzheimer's disease. J Alzheimers Dis 2015;43:1229-36. [PubMed]
- Olsson B, Hertze J, Lautner R, et al. Microglial markers are elevated in the prodromal phase of Alzheimer's disease and vascular dementia. J Alzheimers Dis 2013;33:45-53. [PubMed]
- Craig-Schapiro R, Perrin RJ, Roe CM, et al. YKL-40: a novel prognostic fluid biomarker for preclinical Alzheimer's disease. Biol Psychiatry 2010;68:903-12. [PubMed]
- Antonell A, Mansilla A, Rami L, et al. Cerebrospinal fluid level of YKL-40 protein in preclinical and prodromal Alzheimer's disease. J Alzheimers Dis 2014;42:901-8. [PubMed]
- Simard AR, Soulet D, Gowing G, et al. Bone marrow-derived microglia play a critical role in restricting senile plaque formation in Alzheimer's disease. Neuron 2006;49:489-502. [PubMed]
- Wirths O, Breyhan H, Marcello A, et al. Inflammatory changes are tightly associated with neurodegeneration in the brain and spinal cord of the APP/PS1KI mouse model of Alzheimer's disease. Neurobiol Aging 2010;31:747-57. [PubMed]
- Stöhr O, Schilbach K, Moll L, et al. Insulin receptor signaling mediates APP processing and beta-amyloid accumulation without altering survival in a transgenic mouse model of Alzheimer's disease. Age (Dordr) 2013;35:83-101. [PubMed]
- Ho L, Qin W, Pompl PN, et al. Diet-induced insulin resistance promotes amyloidosis in a transgenic mouse model of Alzheimer's disease. FASEB J 2004;18:902-4. [PubMed]
- Špolcová A, Mikulášková B, Kršková K, et al. Deficient hippocampal insulin signaling and augmented Tau phosphorylation is related to obesity- and age-induced peripheral insulin resistance: a study in Zucker rats. BMC Neurosci 2014;15:111. [PubMed]
- Nisticò R, Cavallucci V, Piccinin S, et al. Insulin receptor β-subunit haploinsufficiency impairs hippocampal late-phase LTP and recognition memory. Neuromolecular Med 2012;14:262-9. [PubMed]
- Lee S, Tong M, Hang S, et al. CSF and Brain Indices of Insulin Resistance, Oxidative Stress and Neuro-Inflammation in Early versus Late Alzheimer's Disease. J Alzheimers Dis Parkinsonism 2013;3:128. [PubMed]
- Matsuzaki T, Sasaki K, Tanizaki Y, et al. Insulin resistance is associated with the pathology of Alzheimer disease: the Hisayama study. Neurology 2010;75:764-70. [PubMed]
- Leoni V, Solomon A, Lovgren-Sandblom A, et al. Diagnostic power of 24S-hydroxycholesterol in cerebrospinal fluid: candidate marker of brain health. J Alzheimers Dis 2013;36:739-47. [PubMed]
- Mroczko B, Groblewska M, Zboch M, et al. Evaluation of visinin-like protein 1 concentrations in the cerebrospinal fluid of patients with mild cognitive impairment as a dynamic biomarker of Alzheimer's disease. J Alzheimers Dis 2015;43:1031-7. [PubMed]
- Caltagarone J, Hamilton RL, Murdoch G, et al. Paxillin and hydrogen peroxide-inducible clone 5 expression and distribution in control and Alzheimer disease hippocampi. J Neuropathol Exp Neurol 2010;69:356-71. [PubMed]
- Llorens-Martín M, Jurado-Arjona J, Fuster-Matanzo A, et al. Peripherally triggered and GSK-3beta-driven brain inflammation differentially skew adult hippocampal neurogenesis, behavioral pattern separation and microglial activation in response to ibuprofen. Transl Psychiatry 2014;4:e463. [PubMed]
- Wang XX, Tan MS, Yu JT, et al. Matrix metalloproteinases and their multiple roles in Alzheimer's disease. Biomed Res Int 2014;2014:908636.
- Sun Q, Hampel H, Blennow K, et al. Increased plasma TACE activity in subjects with mild cognitive impairment and patients with Alzheimer's disease. J Alzheimers Dis 2014;41:877-86. [PubMed]
- Blennow K, Zetterberg H, Fagan AM. Fluid biomarkers in Alzheimer disease. Cold Spring Harb Perspect Med 2012;2:a006221. [PubMed]
- Berenguer RG, Monge Argiles JA, Ruiz CM, et al. Alzheimer disease cerebrospinal fluid biomarkers predict cognitive decline in healthy elderly over 2 years. Alzheimer Dis Assoc Disord 2014;28:234-8. [PubMed]
- Blennow K, Hampel H, Weiner M, et al. Cerebrospinal fluid and plasma biomarkers in Alzheimer disease. Nat Rev Neurol 2010;6:131-44. [PubMed]
- Gustafson DR, Skoog I, Rosengren L, et al. Cerebrospinal fluid beta-amyloid 1-42 concentration may predict cognitive decline in older women. J Neurol Neurosurg Psychiatry 2007;78:461-4. [PubMed]
- Braak H, Braak E. Frequency of stages of Alzheimer-related lesions in different age categories. Neurobiol Aging 1997;18:351-7. [PubMed]
- He J, Qiao JP, Zhu S, et al. Serum beta-amyloid peptide levels spike in the early stage of Alzheimer-like plaque pathology in an APP/PS1 double transgenic mouse model. Curr Alzheimer Res 2013;10:979-86. [PubMed]
- Arodin L, Lamparter H, Karlsson H, et al. Alteration of thioredoxin and glutaredoxin in the progression of Alzheimer's disease. J Alzheimers Dis 2014;39:787-97. [PubMed]
- Holtzman DM, Morris JC, Goate AM. Alzheimer's disease: the challenge of the second century. Sci Transl Med 2011;3:77sr1.
- Blennow K, Vanmechelen E, Hampel H. CSF total tau, Abeta42 and phosphorylated tau protein as biomarkers for Alzheimer's disease. Mol Neurobiol 2001;24:87-97. [PubMed]
- Rosenkranz SC, Geissen M, Harter K, et al. Amyloid-precursor-protein-lowering small molecules for disease modifying therapy of Alzheimer's disease. PLoS One 2013;8:e82255. [PubMed]
- Matsubara E, Takamura A, Okamoto Y, et al. Disease modifying therapies for Alzheimer's disease targeting Abeta oligomers: implications for therapeutic mechanisms. Biomed Res Int 2013;2013:984041.
- Jeppsson F, Eketjall S, Janson J, et al. Discovery of AZD3839, a potent and selective BACE1 inhibitor clinical candidate for the treatment of Alzheimer disease. J Biol Chem 2012;287:41245-57. [PubMed]
- Bach JP, Dodel R. Naturally occurring autoantibodies against beta-Amyloid. Adv Exp Med Biol 2012;750:91-9. [PubMed]
- Lemere CA, Maier M, Peng Y, et al. Novel Abeta immunogens: is shorter better? Curr Alzheimer Res 2007;4:427-36. [PubMed]
- Schneider LS, Mangialasche F, Andreasen N, et al. Clinical trials and late-stage drug development for Alzheimer's disease: an appraisal from 1984 to 2014. J Intern Med 2014;275:251-83. [PubMed]
- Blennow K, de Leon MJ, Zetterberg H. Alzheimer's disease. Lancet 2006;368:387-403. [PubMed]
- Salloway S, Sperling R, Gilman S, et al. A phase 2 multiple ascending dose trial of bapineuzumab in mild to moderate Alzheimer disease. Neurology 2009;73:2061-70. [PubMed]
- Farlow M, Arnold SE, van Dyck CH, et al. Safety and biomarker effects of solanezumab in patients with Alzheimer's disease. Alzheimers Dement 2012;8:261-71. [PubMed]
- Siemers ER, Friedrich S, Dean RA, et al. Safety and changes in plasma and cerebrospinal fluid amyloid beta after a single administration of an amyloid beta monoclonal antibody in subjects with Alzheimer disease. Clin Neuropharmacol 2010;33:67-73. [PubMed]
- Vlassenko AG, Mintun MA, Xiong C, et al. Amyloid-beta plaque growth in cognitively normal adults: longitudinal [11C]Pittsburgh compound B data. Ann Neurol 2011;70:857-61. [PubMed]
- Wang X, Blanchard J, Grundke-Iqbal I, et al. Alzheimer disease and amyotrophic lateral sclerosis: an etiopathogenic connection. Acta Neuropathol 2014;127:243-56. [PubMed]
- Grossman M, Elman L, McCluskey L, et al. Phosphorylated tau as a candidate biomarker for amyotrophic lateral sclerosis. JAMA Neurol 2014;71:442-8. [PubMed]
- Skillbäck T, Rosén C, Asztely F, et al. Diagnostic performance of cerebrospinal fluid total tau and phosphorylated tau in Creutzfeldt-Jakob disease: results from the Swedish Mortality Registry. JAMA Neurol 2014;71:476-83. [PubMed]
- Herbert MK, Eeftens JM, Aerts MB, et al. CSF levels of DJ-1 and tau distinguish MSA patients from PD patients and controls. Parkinsonism Relat Disord 2014;20:112-5. [PubMed]
- Shahim P, Rejdak R, Ksiazek P, et al. Cerebrospinal fluid biomarkers of beta-amyloid metabolism and neuronal damage in epileptic seizures. Eur J Neurol 2014;21:486-91. [PubMed]
- Won HS, Lee KE, Sung SH, et al. Topoisomerase II alpha and microtubule-associated protein-tau as a predictive marker in axillary lymph node positive breast cancer. Tumori 2014;100:80-6. [PubMed]
- Rosén C, Rosén H, Andreasson U, et al. Cerebrospinal fluid biomarkers in cardiac arrest survivors. Resuscitation 2014;85:227-32. [PubMed]
- Risacher SL, Saykin AJ. Neuroimaging biomarkers of neurodegenerative diseases and dementia. Semin Neurol 2013;33:386-416. [PubMed]
- Vemuri P, Wiste HJ, Weigand SD, et al. MRI and CSF biomarkers in normal, MCI, and AD subjects: diagnostic discrimination and cognitive correlations. Neurology 2009;73:287-93. [PubMed]
- Zhang J, Jia J, Qin W, et al. Combination of plasma tumor necrosis factor receptors signaling proteins, beta-amyloid and apolipoprotein E for the detection of Alzheimer's disease. Neurosci Lett 2013;541:99-104. [PubMed]
- Caraci F, Castellano S, Salomone S, et al. Searching for disease-modifying drugs in AD: can we combine neuropsychological tools with biological markers? CNS Neurol Disord Drug Targets 2014;13:173-86. [PubMed]


