Acute incarcerated external abdominal hernia
Introduction
External abdominal hernia occurs when abdominal organs or tissue leave their normal anatomic site and protrude outside the skin through the congenital or acquired weakness, defects or holes on the abdominal wall. Hernia protruding through the groin area (the triangle area formed by the line between bilateral anterior superior iliac spines and the outer edge of the rectus abdominis and the inguinal ligament) is called inguinal hernia, accounting for over 95% of abdominal hernia. Those protruding through the umbilical ring are umbilical hernias, accounting for 6% in adults (including paraumbilical hernia), mostly seen in middle-aged obese women, with a male to female ratio of about 1:3. Hernia protruding through the femoral ring and femoral canal into the oval fossa is called femoral hernia, accounting for 3-5%. Hernia protruding through the abdominal white line is white line hernia, also known as upper abdominal hernia for it is mostly seen above the umbilicus as the abdominal white line there is wider than its narrower and stiffer counterpart below the umbilicus, accounting for 1%. White line hernia below the umbilicus (lower abdominal hernia) is rare. Hernia protruding through the obturator tube is obturator hernia, with a low incidence, accounting for only 0.05-0.14%. Those protruding through an abdominal incision are abdominal incisional hernia, accounting for 1.5%.
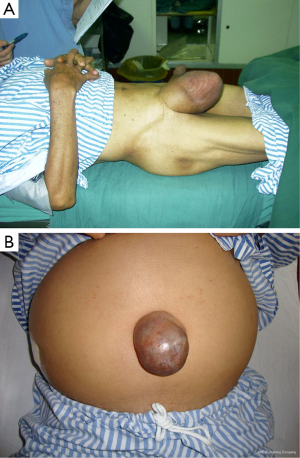
Acute incarcerated hernia is a common surgical emergency (Figure 1A). With advances in minimally invasive devices and techniques, the diagnosis and treatment have witnessed major changes, such as the use of laparoscopic surgery in some cases to achieve minimally invasive treatment. However, strict adherence to the indications and contraindications is still required.
Causes
Reduced abdominal wall strength
Congenital weakness in the abdominal wall: presence of only fascia in the inguinal region, with congenital lack of muscle tissue; unclosed processus vaginalis in some patients; developmental disorders related to umbilical ring closure or abdominal white line fascia fibers, or penetration by blood vessels or fat masses, in a few patients, resulting in holes or defects. Acquired precipitating factors: abdominal surgery or abdominal injuries that cause abdominal wall weakness and infection, or reduced synthesis of collagen fibers and consequently weak wall strength due to old ages, poor nutrition and smoking.
Factors of increased intra-abdominal pressure
Physiological: crying children, pregnant women, and strenuous physical activities. Pathological: abdominal tumors, ascites, chronic coughing, chronic constipation, and long-term difficulty urinating.
Pathophysiology
In the event of a sudden increase in intra-abdominal pressure, hernial contents are squeezed through a narrow hernia sac neck into the sac. The subsequent recoil of sac neck entraps the hernial contents, preventing them from returning into the abdomen, and incarcerated hernia occurs. Incarceration may also occur when omental or mesenteric tumors occasionally enter the abdominal sac and get trapped. As the incarceration persists, venous reflux disorders will first take place with partial arterial perfusion to hernia contents, though blood circulation disorders will gradually develop, leading eventually to necrosis of the hernial contents, or strangulated hernia. When the intestine is involved in the incarcerated hernial contents, intestinal obstruction can be the result, of which excessive expansion over time may lead to ischemia and necrosis, and finally intestinal rupture. Due to severe water and electrolyte loss and absorption of toxins in intestinal obstruction, and following severe abdominal infections and massive release of inflammatory mediators as the result of intestinal rupture, toxic reactions will take place, leading eventually to multiple organ dysfunction syndrome (MODS).
Supplementary examination
X-ray KUB: upright or lateral abdominal plain films often show bowel dilatation, multiple air-fluid levels or other characteristic findings related to intestinal obstruction.
Ultrasound examination: this often shows expansion of the intestines with reverse peristalsis, or fixed masses without peristalsis, or expansion of a fluid-filled bowel; intestinal fluid reflux and thickening and edema of the intestinal wall can be observed, as well as a slightly echogenic, long strip-shaped omentum in the hernia sac. The occurrence of hernia incarceration can be determined by observation of the blood supply in the hernia contents with color Doppler ultrasound.
CT scan: bowel dilation, mesangial thickening and other signs can be observed at abdominal wall defects. A CT scan following oral iodinated contrast is more conducive to determining whether the contents in the sac are intestinal and, if so, the intestinal type. Enhanced scans can help identify the presence of bowel strangulation. For incarcerated hernia with smaller abdominal wall defects, especially femoral and obturator incarcerated hernia that are difficult to diagnosis, CT has its important clinical value. Soft tissue signals seen between the pubic muscle and the obturator muscle, upper and lower bundles of the external obturator muscle, or internal and external obturator muscle, on pelvic CT, support the diagnosis of obturator hernia.
Diagnosis
Identification of the incarcerated hernia site: incarcerated hernia is mainly characterized by tenderness at the incarcerated site, followed by whole abdominal pain, bloating, nausea, vomiting, and intestinal obstruction such as absence of bowel movements. The development of disease course is a key aspect during collection of medical history. Full exposure of the abdomen is required during physical examination, especially the bilateral inguinal region, to rule out incarcerated inguinal hernia. It should be noted that in cases of incarcerated femoral hernia, the small size and thick abdominal wall fat can make the lesion hardly palpable, leading to misdiagnosis. Treatment for incarcerated hernia is often delayed in elderly patients due to unresponsiveness and insensitive to local pain, with abdominal pain, bloating, nausea, vomiting and other intestinal obstruction symptoms being the only clinical manifestations. In this case, the condition can be easily misdiagnosed as general acute intestinal obstruction. Due to hardness of the hernial ring, umbilical hernia is likely to be incarcerated (Figure 1B). In the case of obturator hernia, hernia contents penetrate through the obturator tube from the hip, so the mass is not easily noticeable on the face and may lead to difficulty in diagnosis. The focus of examination should include inner thigh pain and history of inability to straighten the thigh, as well as the unique Howship-Romberg (HR) syndrome of obturator hernia: tingling pain of the inner thigh (symptoms caused by compression of the obturator nerve by hernia contents), radiating to the popliteal and knee area, accompanied by paresthesia. Palpable cords of the incarcerated hernia can be noticed in transrectal or transvaginal pelvic digital examination, with significant tenderness (Figure 2A).
Identification of the presence of incarceration: incarcerated hernia is associated with poor prognosis, and it should be thus suspected with any of the following clinical manifestations: (I) severe abdominal pain, with persistent pain during the interim periods of paroxysmal pain; (II) gradually increased shock; (III) evident peritoneal irritation, and increased body temperature, pulse rate and white blood cell count; (IV) bloody fluid in vomit or intestinal excreta, or from abdominal puncture; and (V) asymmetrical bloating, palpable and tender intestinal loops with rebound tenderness.

Differential diagnosis
Acute intestinal obstruction: standing and supine abdominal plain film, CT and other testings may suggest the nature and location of obstruction, and rule out abdominal wall defects and incarcerated hernia masses.
Hydrocele of the spermatic cord or testicular sheath: in male patients, hydrocele lumps are located in the scrotum, which are oval and the upper end does not enter the outer ring; the upper boundary is often clearly palpable, with a cystic feeling, and the testicle is located in the center of fluid, making it hardly palpable. Spermatic cord hydrocele lumps are elongated oval along the spermatic cord, of which the upper end can enter the outer ring and the lower may be located within the scrotum. Mass movement is visible while pulling the ipsilateral testis. Transillumination test and ultrasound are the main bases for differential diagnosis.
Testicular torsion and ischemic necrosis: incarcerated inguinal hernia can sometimes lead to compression to the ipsilateral spermatic cord and testicle, causing testicular torsion and ischemia. During examination, attention should be paid to the position of the testicle, and disappearance of ipsilateral cremaster reflex. Doppler ultrasound can confirm testicular ischemia.
Cyst of the round ligament: in female patients, a cyst of the uterine round ligament can occur along the full length from inside the inguinal canal to the inner end of the round ligament (the deep fascia fibers at the labia majora and mons pubis). Cysts located in the inguinal canal are present as inguinal mass, while those occurring below in the outer ring are usually pubic masses. Cysts of the round ligament are round, solid masses with clear boundaries, with a cystic feeling. They can not be inserted back, and feel sore when pressed, without a sessile extending deep into the abdominal cavity. Ultrasound can provide evidence for the differentiation.
Enlarged inguinal lymph nodes: a single enlarged lymph node with acute inflammation can be easily misdiagnosed as incarcerated femoral hernia, but the primary focus can often be found in the ipsilateral lower extremity, and the shape is not hemispherical as is the case in femoral hernia. Intestinal symptoms are not present. Multiple inflammatory and enlarged lymph nodes are often distributed along the inguinal ligament, with separation between the hard nodes. The lymph node structure shown on Doppler ultrasound is the main basis for differential diagnosis.
Cellulitis at the thigh root: when incarcerated femoral hernia occurs, swelling or necrotic hernia contents can lead to severe inflammation of the surrounding area of the hernial sac, represented by an enlarged mass with redness and pain, which can often be misdiagnosed as cellulitis. However, patients usually have symptoms of intestinal obstruction, and therefore abdominal X-ray, Doppler ultrasound and abdominal CT or MRI are helpful in the diagnosis.
Cold abscess of the iliac fossa: this is a rare condition that occurs when the spinal tuberculosis pus flows along the psoas muscle into the groin area. There can be a sense of shock when coughing. The mass is slightly reduced if supine, mostly located at the iliac fossa, independent of the outer ring or scrotum. On ultrasound examination, an oval mass is visible along the long axis running from upper outside to inward along the iliac fossa, with rough fuzzy reflective coating full of internal reflection of light points inside, which are evenly distributed, as well as posterior acoustic enhancement. Signs of bone destruction are clear at the discs, and the size, shape and location of the lesion can be located, on spine CT and MRI.
Amyand’s hernia: when acute inflammation of the appendix occurs, it can enter the existing groin hernia on the right side and form incarceration. Since the signs and symptoms of shifting right lower abdominal pain are not typical in these patients, this can be easy confused with incarcerated inguinal hernia. The swelling appendix incarcerated in the hernia sac and abdominal pus found during exploratory surgery provides the basis for differential diagnosis.
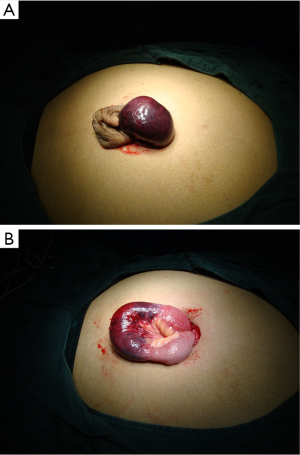
Spontaneous torsion and infarction of greater omentum: this occurs when the tip of the greater omentum enters the underlying open inguinal canal, and forms cord-like adhesion with the bottom of the sac so that the distal and proximal ends of the omentum maintain in a relatively fixed state. Induced by a variety of factors, the distal end rotates around itself and leads to torsion and infarction of the most part of the omentum (Figure 2B). The cord-like adhesion can be revealed during intraoperative exploration (Figure 2C). Abdominal CT is of certain value for the diagnosis of omental infarction.
Treatment
Manual reduction
This is considered for inguinal hernia incarcerated in less than 4-8 h without suspicious strangulation. The patient should be placed supine, with the hip padded at 30°, both hip and knees flexed. Children can be given sedative drugs, and adults given intramuscular analgesic tramadol, or administration of 1% lidocaine on the inside of the anterior superior iliac spine for blocking the iliohypogastric and ilioinguinal nerves, in order to facilitate manual reduction. The physician holds the sac neck with one hand and squeeze the bottom of the sac towards the inguinal canal evenly and continuously with four fingers of the other hand, until all the hernial contents return into the abdomen cavity. Approximately 70% of incarcerated hernia can be reduced manually. Manual reduction may result in serious complications, such as intestinal rupture, peritonitis and even testicular necrosis. Therefore, in the case of failure, surgery should be immediately performed for incarcerated hernia. Obvious scrotal redness and swelling condition warrants routine exploration. Even if the reduction is successful, the patient should be closely observed for 1-3 d. In the event of recurrent abdominal pain, peritonitis, or other signs, laparotomy should be actively performed. For incarcerated hernia where strangulation is highly possible from the appearance, reduction should not be considered. Immediate surgical treatment is required in such case (Figure 3).
Surgery
Elective surgery is recommended for patients whose manual reduction has been successful in 3-5 d to avoid recurrence of incarceration. Failure of manual reduction and signs of strangulation should warrant immediate surgical treatment. Although open and laparoscopic minimally invasive surgery can be considered, laparoscopic surgery has more advantages in the treatment of incarcerated hernia, such as smaller incisions, complete and accurate diagnosis through abdominal exploration, ease of returning incarcerated hernial contents, reduced unnecessary bowel resection, thorough hernia repair, and discovery of other occult hernia, with a low incidence of incision and patch infections. In the surgery for incarcerated hernia, a synthetic patch with anti- infection properties can be used (lightweight, single braid, with antibacterial coating) to perform primary tension-free hernia repair. In the case of bowel strangulation, rupture and infections such as intraperitoneal or sac empyema, however, patches are prohibited and high ligation of the sac or incision closure alone should be preferred, with placement of a drainage catheter at the distal end of the hernial sac. The repair can be performed in half a year after complete wound healing of the weak hernia defects. In recent years, there have been reports of successful primary repair on the infection wounds with biological patches. In the following section, laparoscopic surgery for the treatment of incarcerated inguinal hernia will be described as an example.
Preoperative preparation
Comprehensive assessment before surgery is carried out to exclude contraindications for general anesthesia (such as cirrhosis, severe heart and lung disease); a proper amount of corticosteroids may be used to reduce the systemic toxicity caused by bowel necrosis, or to relieve the reperfusion injury following the return of surviving ischemic bowel; Examination is done to determine whether are predisposing conditions that require perioperative attention such as obesity, diabetes, hormone therapy, pneumonia, skin infections, cirrhosis, use of immunosuppressive agents, immune dysfunction, and appropriate treatment is given accordingly at the stage; Antibiotics are routinely delivered before surgery, which can reduce the postoperative wound infection rate by 50% for cases with inguinal hernia; The abdominal skin is prepared following the conventional laparoscopic practice. The umbilical area is washed, and the patient is instructed to empty the bladder. The surgery is performed usually without an indwelling catheter, though one can be placed for better operative field exposure after anesthesia, and removed on completion of the surgery.
Anesthesia: general anesthesia with endotracheal intubation is used.
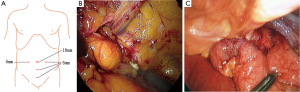
Positioning and the trocars: the patient is placed supine. In the event that the bowel is stacked in the pelvic cavity or iliac fossa blocking the bilateral inguinal region, the operating table can be placed at 15°-30° Trendelenburg position to facilitate exposure of the groin area and protect the intestine. The placement of trocars is dependent on the specific procedure, operating needs and surgeon habits. The recommended options include transabdominal preperitoneal (TAPP) and total extraperitoneal (TEP), which employs a 10 mm trocar at the inferior umbilical edge, a 5 mm trocar at each side of the outer edge of rectus at the umbilical level, and a 5 mm trocar at each of the trisection points of the line between the pubic symphysis and the umbilicus (Figure 4A). The 5 mm trocar close to the pubic symphysis can be moved to the inner superior site of the ipsilateral anterior superior iliac spine to facilitate operation with both hands.
Establishment of pneumoperitoneum and abdominal exploration: a 1.5 cm skin incision is made at the lower umbilical edge. With the help of the small retractor, the umbilical midline is exposed. A veress needle is inserted into the abdominal cavity through the anterior rectus sheath at the contralateral side to the incarcerated hernia to establish pneumoperitoneum at a pressure of 12-14 mmHg. A 10 mm needle sleeve and a 30° laparoscope are placed for exploration. If the patient has a history of abdominal surgery, it is recommended that pneumoperitoneum should be established using an open method, which is completed by placing the trocars after gradual exposure of the abdominal layers under direct vision. Aspects to be explored after the placement of laparoscopic instrument include the establishment of pneumoperitoneum observed, injury to vessels or the intestine during the placement of trocars; traits, presence of empyema; presence of bowel, mesentery, epiploic appendices and other intestinal hernia in the bilateral inguinal, femoral, obturator, original abdominal incision areas; identification of the site of incarcerated hernia and hernial contents; preliminary determination as to whether the bowel, mesentery or omentum is strangulated and necrotic; and complication by abdominal tumors or variations.
Reduction of incarcerated hernial contents: it is significantly easier to return hernial contents under anesthesia with pneumoperitoneum than using open surgery. Under laparoscopic vision, reduction of hernial contents is first attempted with squeezing from outside following the same procedures as in manual reduction. The procedure should be gently done with appropriate force. Violent operation may result in rupture of the bowel or mesentery. In the case of failure, a 0.5 cm incision can be made at each side of the outer edge of rectus at the umbilical level to place a 5 mm trocar, from which the contents can be returned with the help of non-invasive intestinal forceps. The preferred site for retraction is the greater omentum, followed by the intestine. If intestinal edema and inflammation is obvious, gauze can be placed in to wrap the intestinal contents before them are pulled with the clamp. If the above procedure still fails to return the hernial contents, forced retraction should be avoided. In this case, a 1-2 cm incision made to the narrow hernial ring can be of great help. For indirect inguinal hernia, the incision can be made to the outer superior site of the inner ring, while an incision to the inner or inferior site may result in damage of the inferior epigastric artery or iliac artery and vein; for direct inguinal hernia, an incision can be made to the inner site to separate the outer edge of the rectus. In the case of femoral hernia, the lacunar ligament in the femoral ring can be divided (Figure 4B). If the above procedure still fails, an additional 5-6 cm incision can be made at the ipsilateral inguinal site to expose the incarcerated omentum or bowel. The omentum that is difficult to return can be resected, if necessary, followed by high ligation of the hernia sac, and suture closured by layer before continuing the laparoscopic surgery.
Secondary exploration to identify strangulated contents: Multiple observations of the changes in the affected area are key to identifying the presence of strangulated hernia. When incarcerated hernia contents are returned into the abdomen, they can be flipped in the abdominal cavity to observe the color, elasticity, damage, leakage of intestinal contents, intestinal peristalsis, mesentery artery pulses and so on, to establish a comprehensive assessment of the strangulation (Figure 4C). In the case of difficulty in determination, warm saline can be applied into the abdominal cavity to immerse the intestine for 20-30 min before judgment. For a small amount of incarcerated greater omentum or epiploic appendices can be left untreated and simply returned. In the case of strangulated omentum, particularly torsion and infarction, the infarct part can be resected and extract from the abdominal cavity with a sample bag before continuing with the repair. In the case of incarcerated or strangulated hernia or abdominal and hernial empyema, it is advisable to perform laparoscopic ligation of the ring for the inguinal hernia only. For femoral hernia, interrupted suture of the iliopubic bundles and the Cooper ligament and lacunae ligament can be used; for obturator hernia, interrupted suture of the internal obturator muscle and fascia can be performed. Afterwards, the procedure is switched to open surgical resection of necrotic intestines, or the umbilical incision can be expanded to a 4 cm incision to pull out the necrotic intestines and complete resection and anastomosis. The hernial defects are left for secondary repair later.
Laparoscopic inguinal hernia repair: in laparoscopic surgery for incarcerated hernia without strangulation necrosis, TAPP or TEP repair can be considered (Figure 5). Despite its simpleness, the TAPP technique destroys the peritoneal integrity and is thus associated with increased risk of patch infections, and the procedure may be compromised due to intestinal swelling. TEP surgery is, on the other hand, more complex, but with the reserved integrity of the peritoneum, the risk of patch infections and possibility of being affected by swelling intestines is low. Surgeons may choose either surgical option based on their experience and skills.
After returning the hernia contents and confirming there is no strangulation, the abdominal air is exhausted, the umbilical tube removed, and the incision to the anterior rectus sheath is closed. The lower umbilical edge is exposed with the assistance of small hook retraction, and the anterior sheath is divided in an area of about 1 cm at the affected side. A transverse incision of 0.6 cm is made to place a 10 mm trocar along the rectus and the posterior sheath, followed by placement of the laparoscope. As the posterior pubic area and the posterior groin extraperitoneal space are initially divided using the scope, a 5 mm trocar can be placed at each of the trisectional points of the line between the pubic symphysis and the umbilicus to insert a dividing clamp and a pair of scissors for complete separation of the extraperitoneal space with blunt and sharp dividing techniques to expose the pubic symphysis, pubic tubercle and ipsilateral Cooper ligaments. Attention should be paid as to whether there is a direct hernial mass across the Cooper ligament into the Hesselbach triangle. As the separation continues outward along the Cooper ligament, the abnormal obturator artery and vein can be seen about 5 cm away from the pubic symphysis, that is, Corona Mortis vessels, as well as the femoral ring located anterior and superior to them. Attention should be given to rule out femoral hernia. If the incarcerated femoral hernia contents are greater omentum or epiploic appendices, the intestinal tube should be excluded. The returning can be done after the separation of the extraperitoneal space. As soon as the lacunar ligament inside the ring is divided, the incarcerated greater omentum or epiploic appendices can usually be released immediately.
Although it is relatively easy to peel off a direct hernial sac, the difficulty can vary in the case of an indirect hernial sac depending closely on the sac diameter, thickness, depth, and adhesions and edema around the inner opening. In men patients, care should be given to protect the vas deferens and testicular blood vessels, without the need for deliberately separating the bottom of the sac. After separation surrounding the internal ring, the sac can be ligated and cut, and left as is after stopping the bleeding at the distal end. In women, due to the close relationship between the uterine round ligament and the hernial sac, there can be difficulties in the separation. Hence, it can be highly ligated together with the sac for future placement of the patch incision. During the ligation, the distal sac should be open to avoid postoperative hernia effusion.
The proximal sac and the peritoneal return are separated to completely divide the Bogrus space. A separate clamp is used to grab the ligated site of the inguinal hernia sac and pull it to the head, and another clamp is used to separate the testicular blood vessels and the vas deferens from the sac. Lipomas attached to the spermatic cord should be separated as well to free the testicular vessels and vas deferens from the abdominal wall. The sac and peritoneal return should be more than 5 cm away from the inferior epigastric vessels, or the opening of the inner ring. The Bogrus space is thoroughly separated outwards along the peritoneal return until the level of the anterior superior iliac spine, so as to provide sufficient area to place the patch. Since the surrounding structures are often involved in incarceration, leading to peritoneal swelling and fragileness around the inner opening, the operation should be done accurately and gently, taking care to protect the reproductive femoral nerve and lateral femoral cutaneous nerve.
A polypropylene patch in the size of 14-15 cm × 10-11 cm is placed into the extraperitoneal space through the 10 mm umbilical trocar, expanded flat until the inner side exceeds about 1 cm beyond the pubic symphysis and the outer side reaches the bottom of the anterior superior iliac spine, covering to 1 cm below the Cooper ligament, so as to completely cover the pubic muscle hole and avoid missing the obturator. The outer bottom edge of the patch is attached closely to the psoas muscle to ensure it is not floating on top of the peritoneal return, and it is fixed with screw nails. For female patients, the patch can be notched to bypass the round ligament of the uterus before stitching or stapling cracks to avoid excessive use of multi-strand braided nonabsorbable suture. A single strand of absorbable suture is recommended. The patch should be placed flat, fixed firmly to prevent curling, folding or excessive overlapping, which may result in redundant space around the patch and the subsequent infections. The choice of patches should be based on those with larger holes, lightweight, thin types, or those with an anti-bacterial coating.
After the surgery for incarcerated inguinal hernia, peritoneal drainage should be routinely placed posterior to the pubic symphysis, which is removed in 24-48 h or even 72 h when necessary until daily drainage is <5 mL. If the hernia mass is relatively large (>15 cm), another thin drainage should be placed at the bottom of the residual sac, penetrating out through the groin or scrotum and fixed. The outer bottom edge of the patch is attached closely to the psoas muscle with a clamp to avoid a gap between the lower outer edge of the patch and the psoas muscle, which can become a risk of hernia recurrence. The abdomen is then slowly deflated, and the peritoneal membrane will naturally cover the patch with the effect of intra-abdominal pressure to complete the inguinal hernia repair.
Final abdominal exploration and repair of peritoneal defects: a 10 mm trocar is again placed into the abdominal from the original pole to establish pneumoperitoneum for exploration and confirmation as to whether there are strangulation and necrosis of the contents of incarcerated hernia, active omentum bleeding, retroperitoneal rupture, patch shift, and so on. If any, such issues can be resolved by placing instrument through the bilateral trocars along the rectus abdominis. Large peritoneal defects can be repaired using titanium clips and screws or directly closed with suture. The wounds at bilateral rectus sheaths at the umbilical midline are sutured to complete the surgery.
Postoperative care
Prophylactic antibiotics for 3-5 d, extended properly for patients with strangulation or diabetes; Active treatment of accompanying medical conditions such as liver cirrhosis, heart disease, and respiratory tract infections; Wound infections, which can be divided into shallow and deep infections according to the clinical manifestations (patch infection). The former generally occurs in 30 days after surgery, which involves only the skin and subcutaneous tissue and can mostly be treated through open drainage and dressing changes. The latter generally occurs after 30 days, involving fascia, muscles and patches, and in most cases all patches are required to be removed. Follow-up: the reported incidence of patch infections is 0.35%, with a significant late onset nature in about 2 to 4.5 years after surgery. Therefore, close follow-up and timely diagnosis and treatment can be helpful.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Yang XF, Liu JL. A 52-year-old man with right incarcerated inguinal hernia for 10 hours receives emergency laparoscopic surgery. Asvide 2014;1:351. Available online: http://www.asvide.com/articles/369